Electrocardiographic Criteria for Diagnosing Left Ventricular Hypertrophy
Reliable ECG findings of LVH:
- The presence of prominent voltage with left atrial and ST-T abnormalities
- Leftward axis
- Widening of the QRS complex
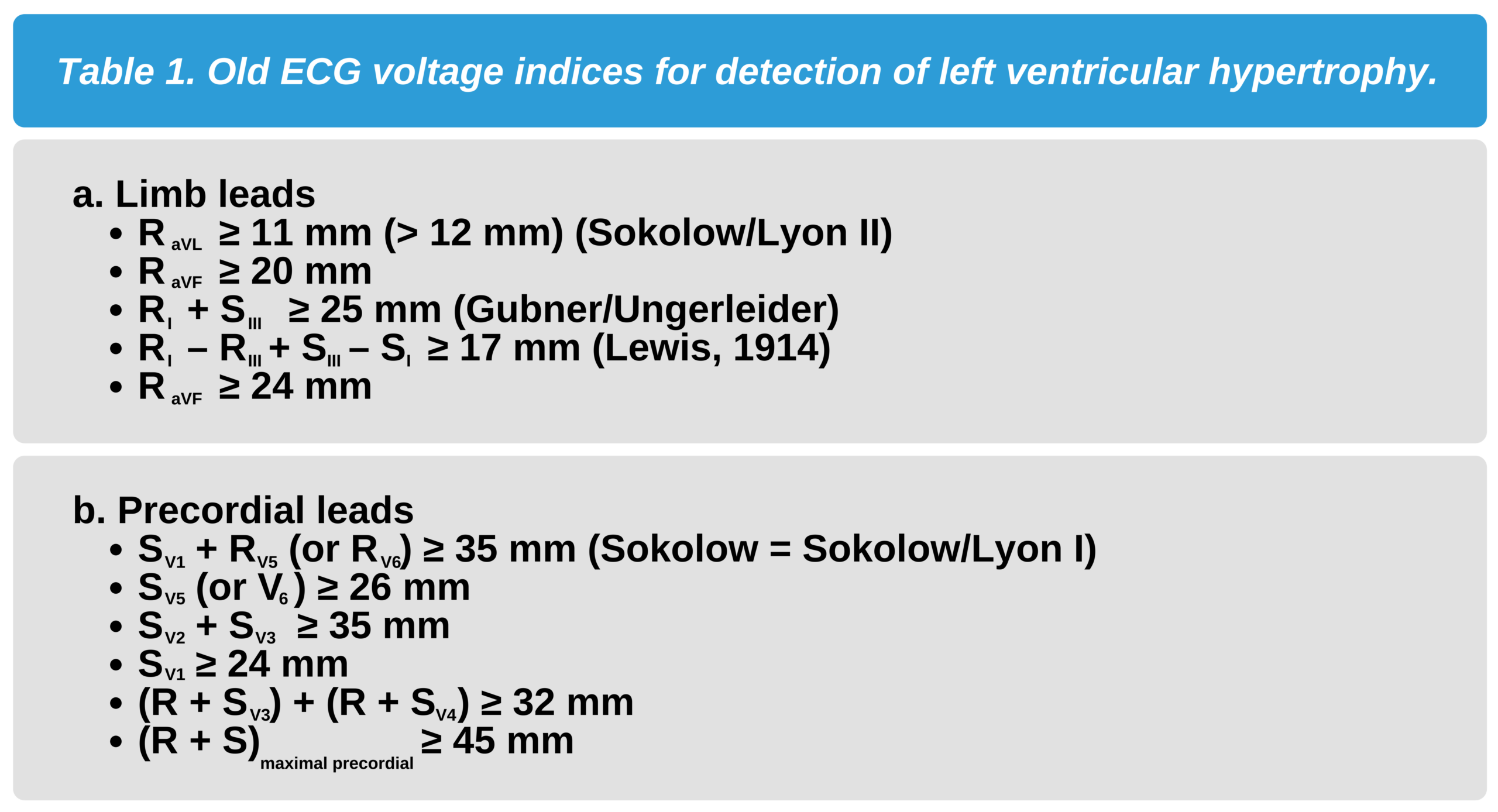
These three findings are not always present together. The indices showcased below are commonly used to accurately diagnose LVH. Some of the indices were proposed in the first half of the 20th century but still have value today.
If one or two of the older indices listed in Table 1 are present with positive indices in Table 2, then a clinician can diagnose LVH with great accuracy.
The following are the indices for detecting LVH:
ECG Findings in LVH Sokolow-Lyon Criteria
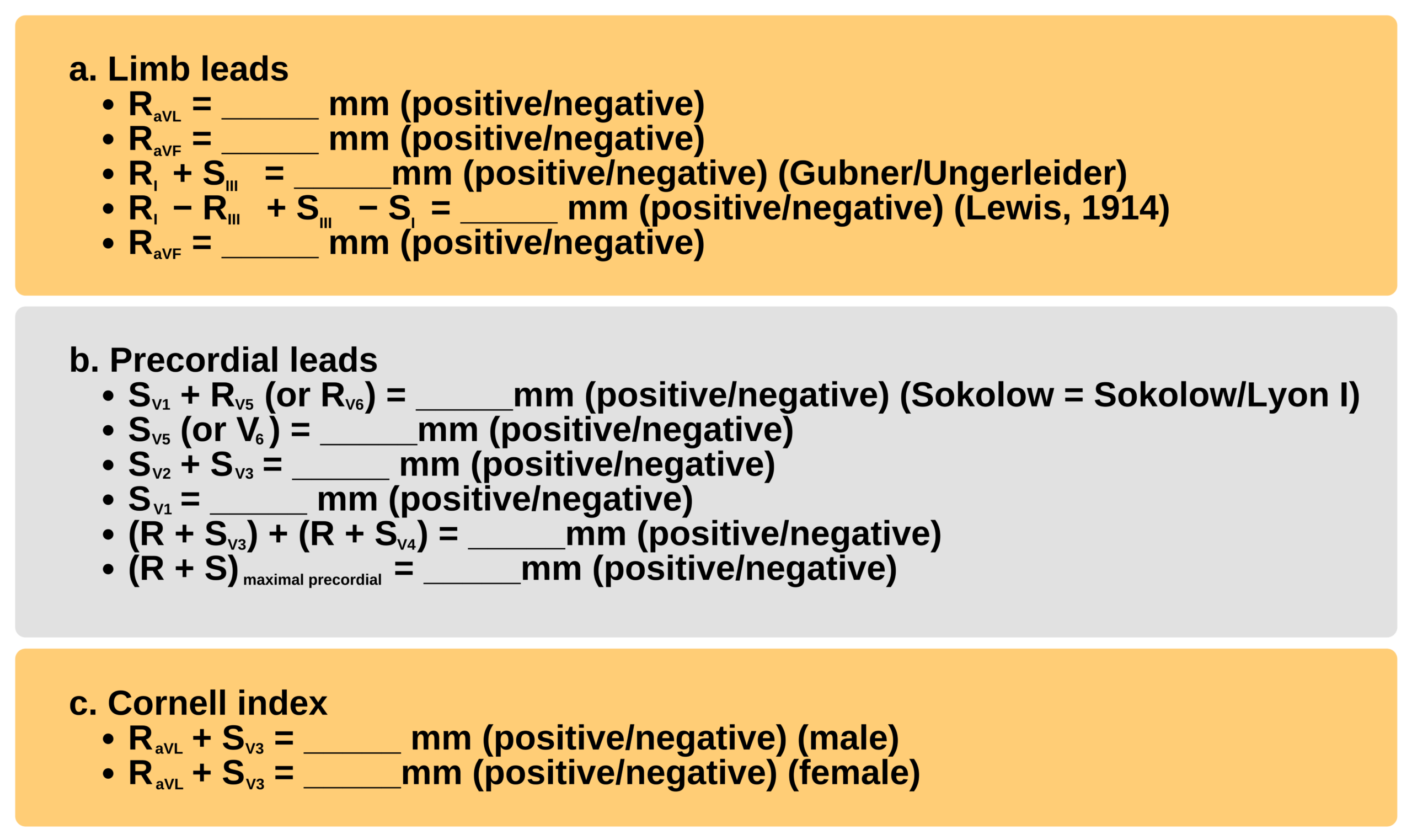
EXERCISE 1:
Directions: Fill in the blanks below and indicate whether the ECG finding in Figure 1 is positive or negative for LVH.
Limb leads: RaVL = _____ mm; RaVF = _____ mm; RI = _____ mm; RIII = _____mm; SI = _____ mm;
SIII = _____ mm
Precordial leads: RV3 = _____ mm; RV4 = _____ mm; RV5 = _____ mm; RV6 = _____ mm;
SV1 = _____ mm; SV2 = _____ mm; SV3 = _____ mm; SV4 = _____ mm; SV5 = _____mm;
SV6 = _____ mm
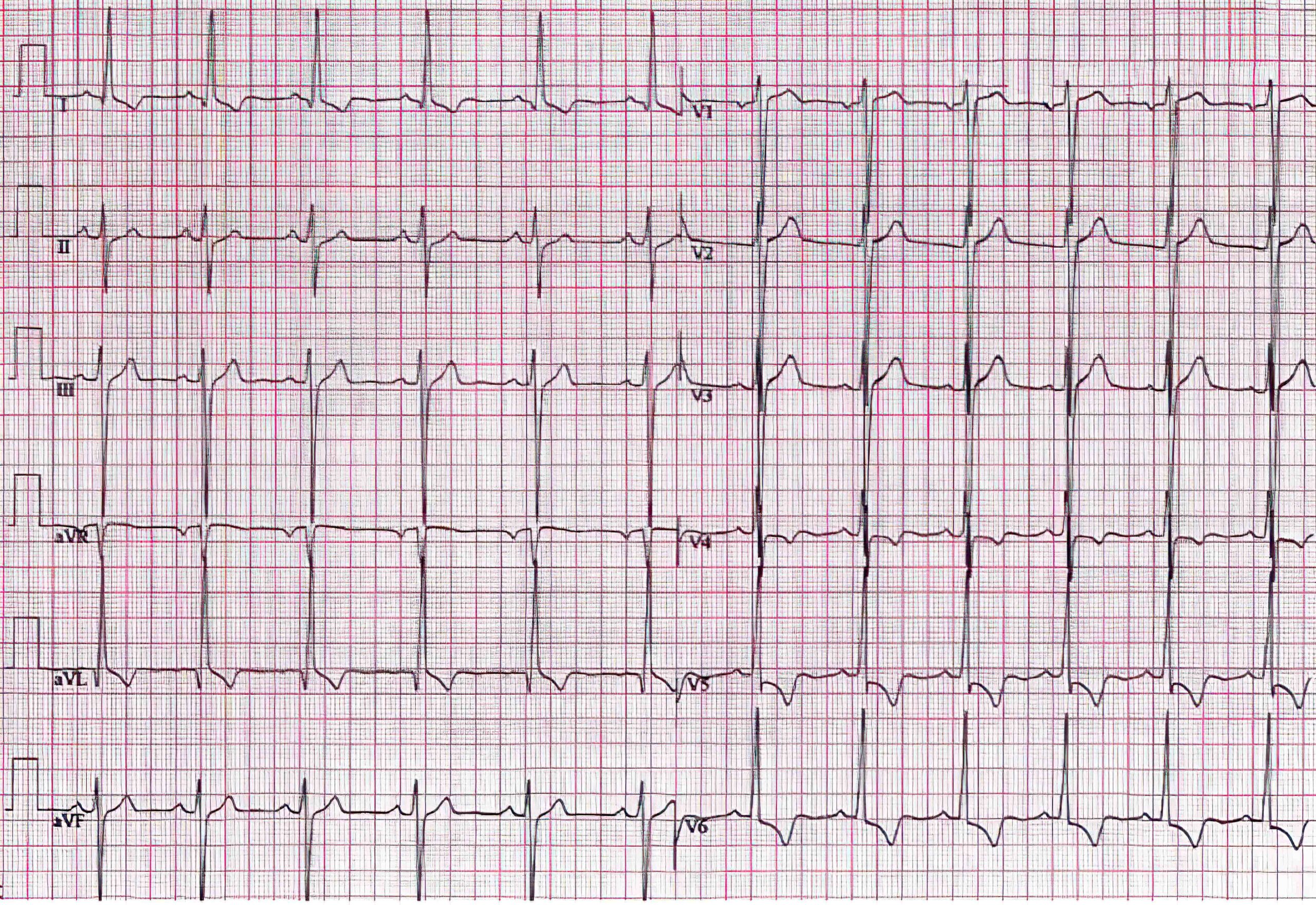
12-Lead ECG of a 52-Year-Old Man With Severe LVH 1 Year After Aortic Valve Replacement for Valve Incompetence
Accuracy
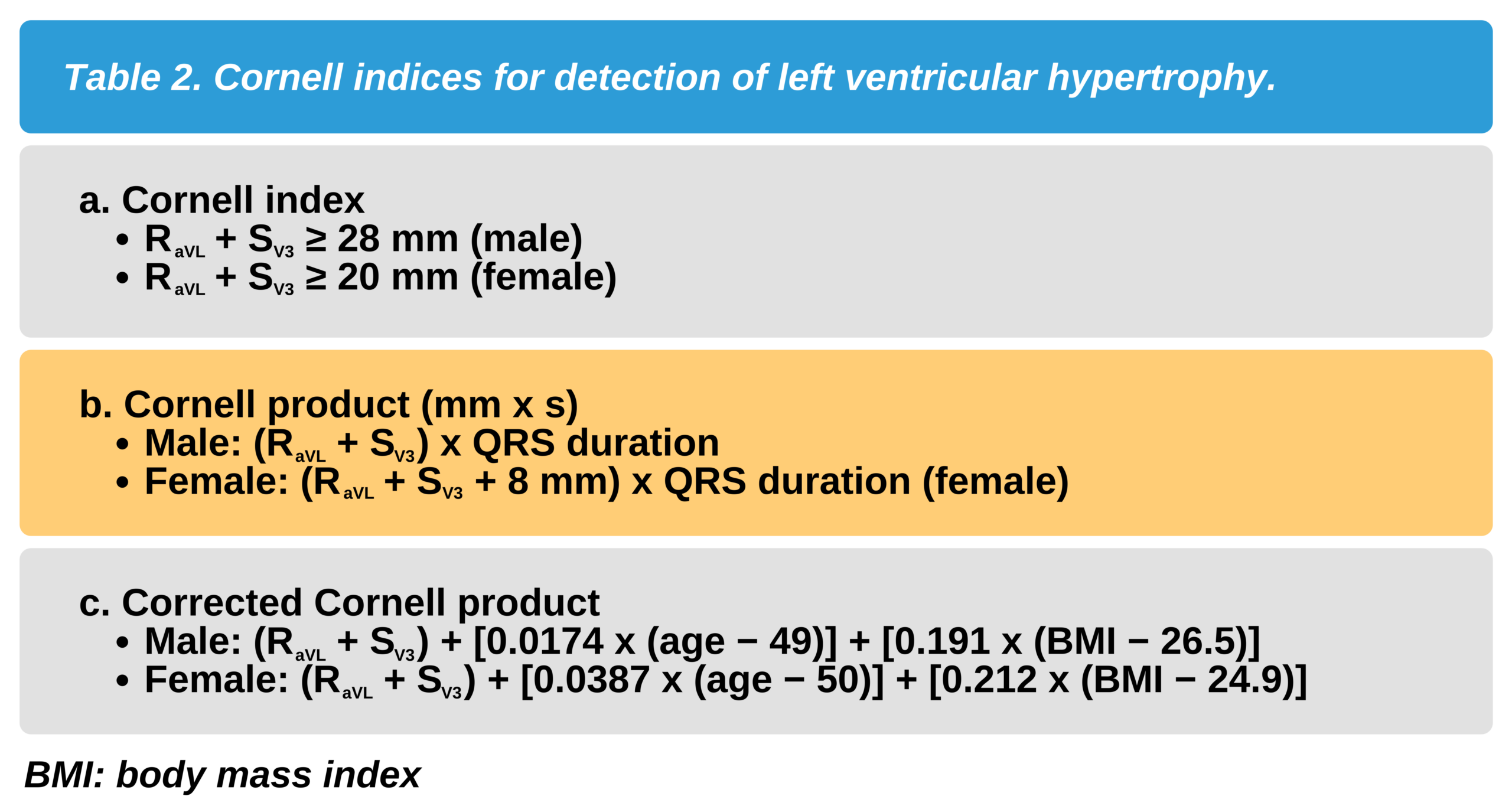
The Cornell index proposes that LVH is present if the sum of the voltage of the R wave in lead aVL and the voltage of the S wave in lead V3 is ≥ 28 mm in men or ≥ 20 mm in women.
Cornell Index: RaVL + SV3 ≥ 28 mm in men and ≥ 20 mm in women
The Cornell index has a specificity of 80–90% and a sensitivity of 30%. In other words, the index is very good at avoiding false negatives but may not detect LVH in 70% of patients where it is present.
In practice, both the Cornell and Sokolow indices should be assessed and viewed together when diagnosing LVH to achieve a higher specificity.
Due to the lower sensitivity, ECG findings of high R waves or deep S waves in leads that are not part of the indices must not be ignored. Patients who present with high R waves and deep S waves in other leads are still suspicious for LVH.
The typical signs of diastolic overload include:
- High but thin R waves
- A slightly elevated ST segment in the lateral leads (ST elevation in leads V1 and V2 is a normal finding)
- High, almost symmetric, positive T waves
False positives are common in young or thin individuals who may have voltages exceeding the conventional ECG findings. Increased voltage is seen in athletes and is a normal variant in these patients. False negatives are common in patients with RBBB, obesity, or chronic obstructive pulmonary disease.
Sensitivity is reduced in women and patients who are obese. Patients with RBBB with decreased S waves in leads V1 and V2 may not meet some of the voltage criteria listed above in Table 1 and Table 2 and go undiagnosed if only the index is used.
Image Findings
Echocardiography is the radiologic imaging of choice for identifying LVH. It provides immediate results, is readily available, and is cost-effective. It is also noninvasive and does not expose the patient to radiation or require intravenous contrast administration.
Prognostication
An ECG finding of LVH has some prognostic significance. Studies have shown that ECG markers of LVH are associated with a significant increase in mortality.
Patients with LVH and ST-T wave abnormalities have a three-fold rate of heart failure over 5 years. These patients also have a four-fold risk of heart failure-related mortality compared to patients without ST-T wave abnormalities.6
Studies have also shown that the presence of LVH on ECG with associated echocardiographic findings provides information regarding the risk of atrial and ventricular arrhythmias in susceptible patients.7
6 Bang CN, Devereux RB, Okin PM. Regression of electrocardiographic left ventricular hypertrophy or strain is associated with lower incidence of cardiovascular morbidity and mortality in hypertensive patients independent of blood pressure reduction – A LIFE review. J Electrocardiol. 2014;47(5):630–635.
https://www.sciencedirect.com/science/article/abs/pii/S0022073614002131
7 Aro AL, Chugh SS. Clinical diagnosis of electrical versus anatomic left ventricular hypertrophy: prognostic and therapeutic implications. Circ Arrhythm Electrophysiol. 2016;9(4):e003629.
https://www.ahajournals.org/doi/full/10.1161/CIRCEP.115.003629