The QRS Complex
The QRS complex morphology is inconsistent in the frontal plane. The ÅQRSF is also dependent on the age of the patient. Table 1 presents the QRS morphology in the frontal plane at varying ages.
A sudden change in ÅQRSF to the left likely represents an inferior myocardial infarction or a new left anterior fascicular block (LAFB). A sudden change of ÅQRSF to the right represents an acute pulmonary embolism.
Table 1. Frontal QRS Axis by Age
The QRS complex in the horizontal plane has a rather uniform morphology. In the chest leads, there is a transition from a more negative QRS complex to a positive one.
- Leads V1 and V2 have an rS complex, characterized by a small R wave and a deep S wave, which is more pronounced in V2.
- Beginning in V3, the R wave increases its amplitude, although the S wave still predominates.
- In V4, the R wave is more positive than the S wave, exhibiting an Rs complex (big R wave, small S wave).
- This progression continues in V5 through V6.
- Leads V5 and V6 have a small initial deflection, forming a qRs complex (small Q wave, large R wave, small S wave).
- The R wave’s transition from a negative deflection to a positive deflection, as seen in Figure 6, is known as the R wave progression.
Figure 5. QRS Complex Transitioning from Negative to Positive Deflection
Figure 6. R-Wave Progression
Clockwise and Counterclockwise Rotation in the Horizontal Plane
The normal R wave progression across the chest leads results in a switch to a positive R wave deflection in V3 or V4. If the transition happens after V4, then there is a clockwise rotation (of the heart’s axis) in the horizontal plane. If the transition period happens before V3, then there is a counterclockwise rotation in the horizontal plane.
This shows QRS variation and the clockwise/counterclockwise rotation.
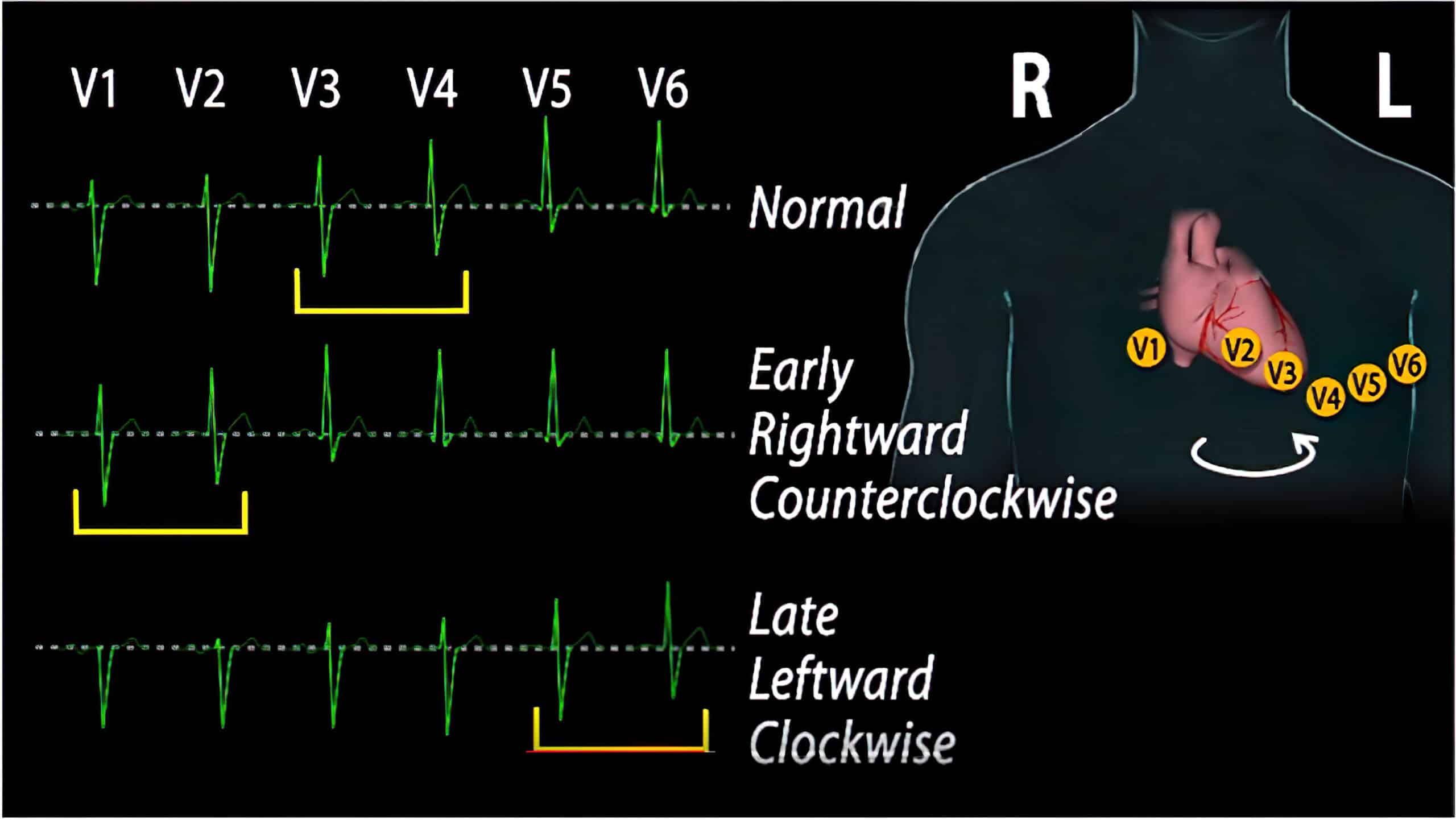
QRS Variation
Suboptimal placement of the precordial leads V1 through V6 is the most likely cause of a clockwise or counterclockwise rotation of the QRS complex in the chest leads in a patient with no medical history.
A late transition (V5 to V6) caused by a clockwise rotation is indicative of heart rotation and may be present in patients with chronic obstructive pulmonary disease, an anterior myocardial infarction that has caused conductive defects, or dilated cardiomyopathies. Severe clockwise rotation causes poor R wave progression and is seen in severe myocardial infarction.
An early shift of the transition zone (i.e., appearing in V1 or V2) caused by a counterclockwise rotation is indicative of conduction defects secondary to a posterior myocardial infarction. It may also be caused by an electrical shift to the right secondary to right ventricular hypertrophy.
QRS Variants
Q waves are usually a sign of an old infarct, but they can be a normal variant in lead III. A distinguishing characteristic of normal variants is that there is no clinical indication of any pathologic disease.
QIII
Finding a QR, Qr, or QS complex in lead III is a normal variant (see Figure 7). The same is true in lead aVF, but this is a rare occurrence. A nonpathologic QIII presents with T waves that have a positive and asymmetric deflection.
A normal variant diagnosis is made if the patient presents without relevant medical history, such as coronary artery disease or a previous inferior wall myocardial infarction. Sometimes an old inferior wall infarct can present with a positive T wave deflection. QIII can also be seen in cardiac disease with systolic overload, LVH, or a LBBB.
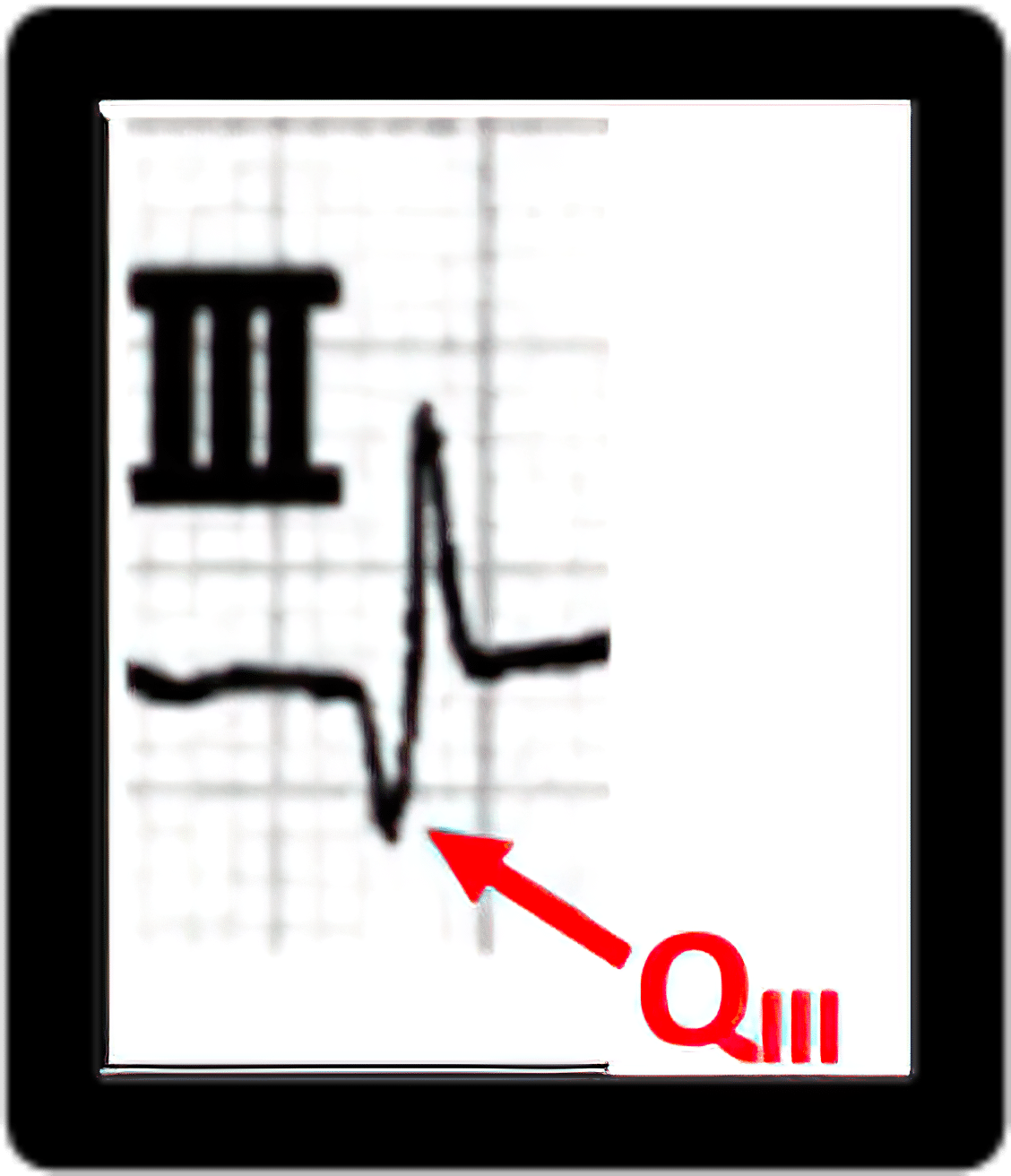
Figure 7. QIII
QSV1/V2 Type
The QS pattern in V1 and V2 is also a normal variant or can be produced by placing the precordial leads too high (usually by one intercostal space). Patients with cardiac conditions who present with a QS pattern in V1 and V2, together with a Q wave in V3, notching in other precordial leads, and a negative deflection of the T wave, may have an old anteroseptal myocardial infarction. Figure 8 is an example of a QS pattern.
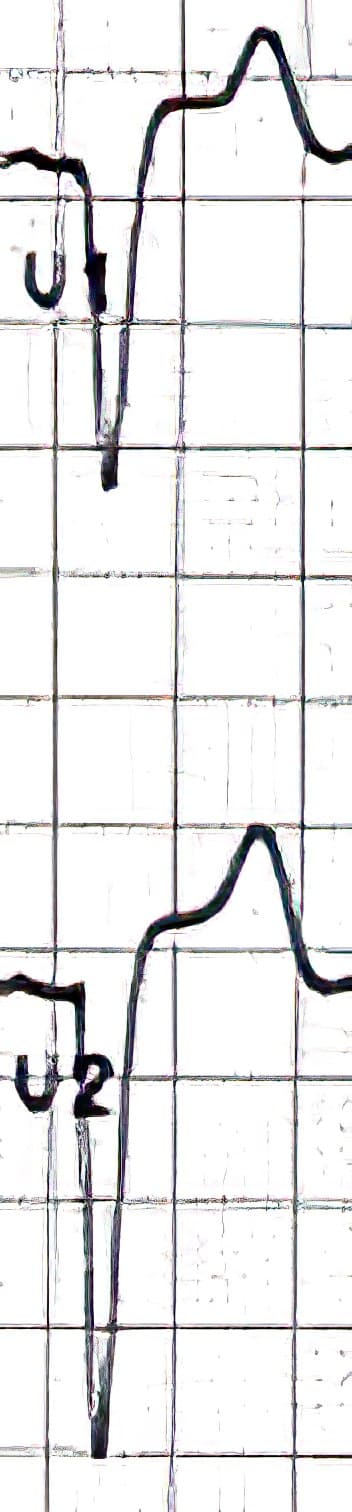
Figure 8. QS Pattern in V1 and V2
Pseudo-Preexcitation (Pseudo-Delta Wave)
A delta wave is a slurring of the upstroke on the QRS complex. It occurs when the ventricles are excited earlier than normally expected, i.e., in the first 0.20 seconds.
A delta wave in the inferior leads III and aVF and in the precordial transition zone is a normal variant if there is a normal PQ interval. Figure 9 presents a delta wave in the presence of a normal PQ interval.
A delta wave may suggest an underlying pathological condition if the PQ interval is prolonged.
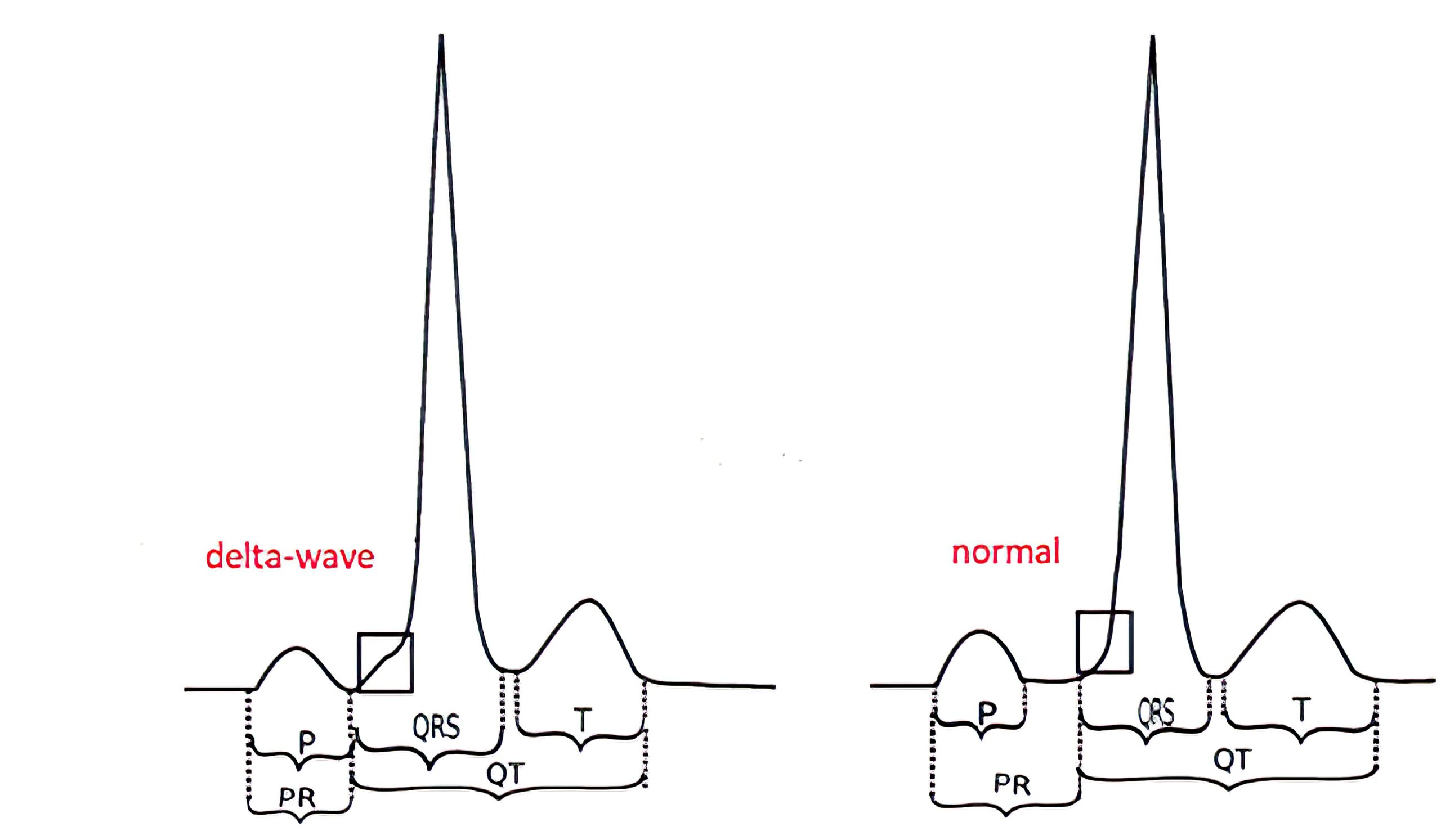
Figure 9. Delta Wave Morphology ECG
SI/SII /SIII Type
Also known as a sagittal type, the SI/SII/SIII type presents with an S wave in limb leads I through III and usually has no significance. When the SI/SII/SIII pattern is present as a normal variant, the T waves should present with an upward deflection. This pattern is also seen in patients with right ventricular hypertrophy, though that presentation is rare.
Figure 10 depicts the SI/SII/SIII pattern. The presence of inverted T waves suggests a right ventricular strain characteristic of right ventricular hypertrophy. If this were a normal variant, the T waves would have an upward deflection.
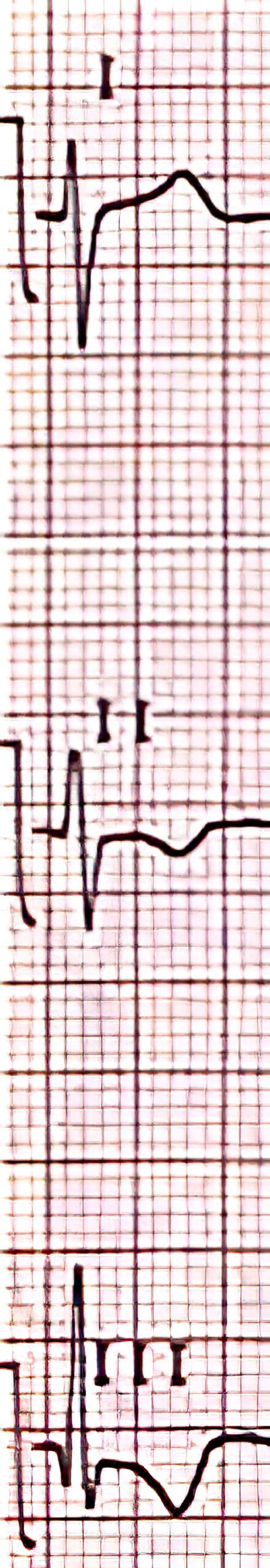
Figure 10. SI/SII/SIII Pattern With Inverted T Waves Indicating Right Ventricular Hypertrophy
Pseudo-Notching or Pseudo-Slurring
Notching and pseudo-notching are caused by a localized delay of conduction, excitation, or projections. Pseudo-notching is a normal variant in the QRS complex when present in the inferior frontal leads III and aVF or in the precordial transition zone that is restricted to one or two precordial leads. It is characterized by the formation of a notch about 1 to 2 mm high within the Q, R, or S wave. If there is only slight notching (< 1 mm), then it is called pseudo-slurring.
Left posterior fascicular block (LPFB) is a pathological cause of notching. LPFB presents with notching or slurring in the R downstroke in leads III, aVF, and V6. Notching or slurring can also be caused by left anterior fascicular block (LAFB) in the presence of left-axis deviation. In this case, the notching is seen in the R downstroke at leads I and aVL.
Notching in the limb leads may represent an old myocardial infarction. Notching in three or more precordial leads indicates an intraventricular conduction disturbance likely from scarring caused by myocardial infarction.
Figure 11. Notching Versus Slurring
Low-Voltage QRS
A low-voltage QRS complex exhibits an amplitude < 5 mm (0.5 mV) in five out of the six limb leads. This assumes the amplitude on the ECG machine is set with conventional settings.
A low-voltage QRS complex is rare in patients without certain medical conditions. Low voltage QRS complexes are seen in patients with lung empyema, obesity, or extensive pericardial effusion. Patients treated with adriablastin, a chemotherapeutic agent for the treatment of cancer, often present with low-voltage QRS, likely due to the cardiotoxic effect of the drug. Other cardiotoxic medications may also cause a low-voltage QRS.
Incomplete Right Bundle Branch Block
Incomplete right bundle branch block (iRBBB) is a common finding, especially in young patients. The characteristic pattern of iRBBB is the presence of notching or rSr’ in lead III. A normal variant is likely if the r is greater than r’ as seen in Figure 12.

Figure 12. r-S-r’ Complex Notching
An r’ greater than r is a characteristic of right ventricular overload and is typically seen in patients with pulmonary embolism, pulmonary hypertension, or right ventricular hypertrophy.
New-onset iRBBB suggests acute right ventricular overload. However, it can also be caused by the misplacement of the V1 precordial lead.