Electrocardiogram Characteristics of Sinus Node Dysfunction
Sinus Bradycardia
A heart rate < 50 bpm is classified as sinus bradycardia. When a patient has undergone sympathetic stimulation through exercise or with pharmacologic sympathomimetics (drugs that induce the sympathetic nervous system), a rate < 90 bpm is considered sinus bradycardia.
Sinus Arrest
In sinus arrest, no impulse comes from the sinus node. The ECG tracing in patients with sinus arrest resembles that of patients with second-degree or complete sinoatrial block. However, longer episodes without any P waves favor the diagnosis of sinus arrest. The periodic absence of P waves is more indicative of second-degree sinoatrial block.
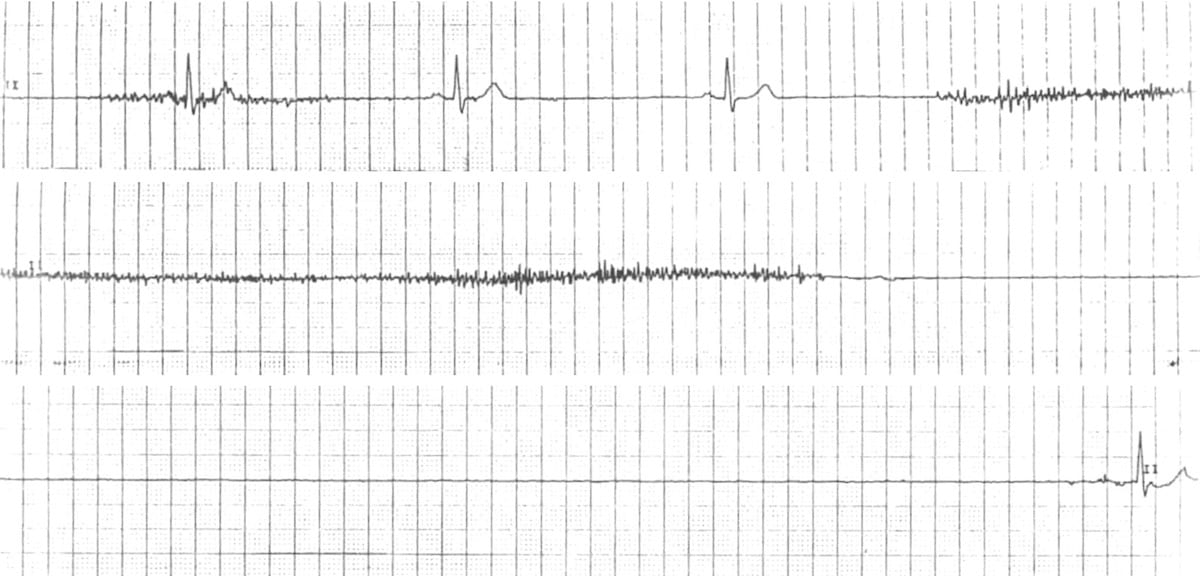
Sinus Arrest ECG 37
The ECG above represents sinus arrest. The tracing shows a prolonged absence of sinus node activity represented by the absence of P waves for more than 3 seconds.
Sinoatrial Block
Sinoatrial block (or exit-block) is caused by a conduction block near or surrounding the sinus node fibers. This produces a conducted sinus impulse into the atria and AV node.
Sinoatrial block is classified as first-degree, second-degree, and complete sinoatrial block. ECG monitoring with a Holter monitor can only detect second-degree sinoatrial block. It is common to see a 2:1 or 3:1 block.
Distinguishing complete sinoatrial block from sinus arrest when the duration of the sinoatrial block is prolonged is difficult.
The ECG below exhibits second-degree sinoatrial exit block. An impulse that was not able to exit through the normal transitional cells of the SA node has exited elsewhere. This caused abnormal P wave morphology in the second PQRS complex. The “second” sinus impulse is observed to be completely blocked since there is no P wave or QRS complex.
Related Video – ECG Rhythm Review – 2nd Degree Heart Block (Type 2)
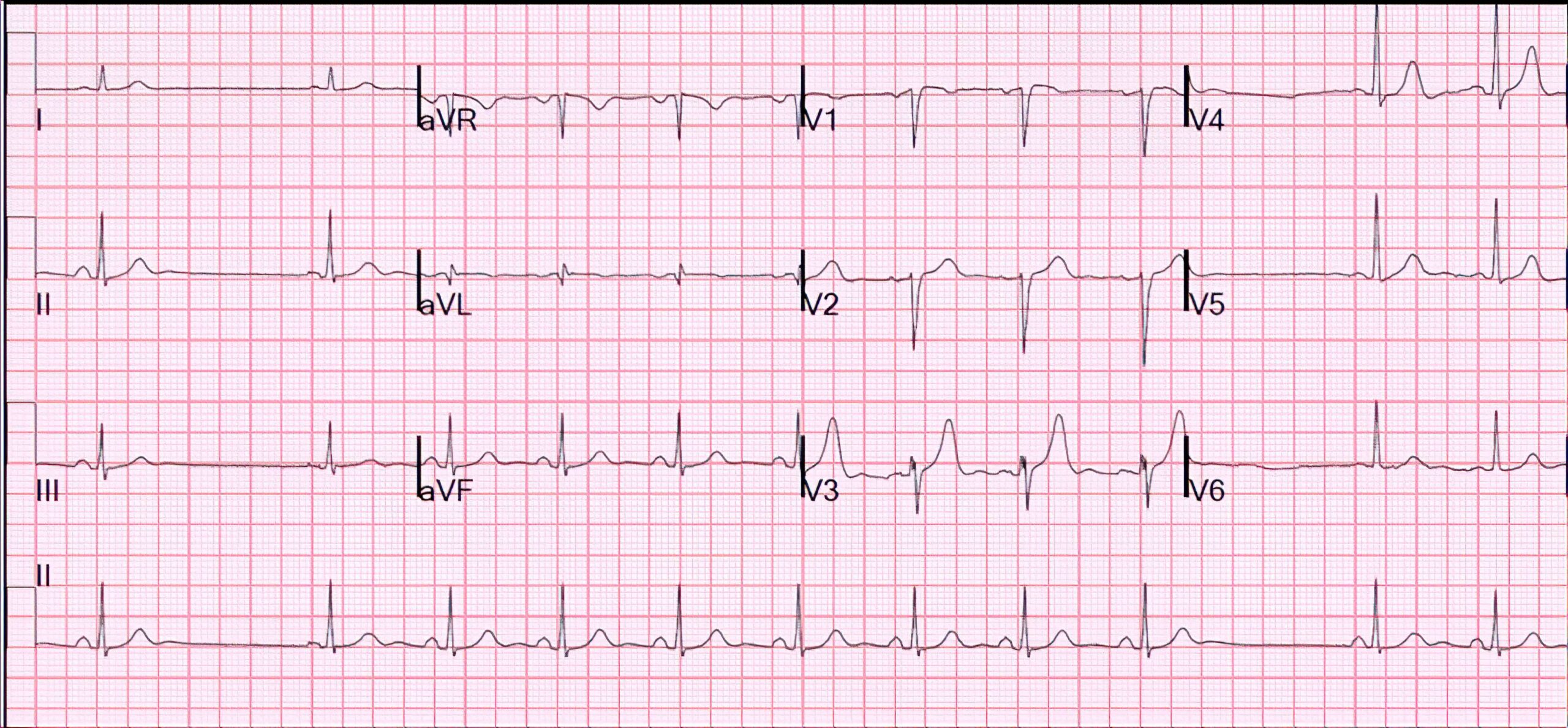
Young Patient Palpitations ECG
Bradycardia-Tachycardia Variant
Due to the bradycardia component of sinus node dysfunction, some patients experience a compensatory increase in the firing rate that produces PACs, irregular atrial tachycardia, atrial flutter, AV nodal reentry tachycardia, or atrial fibrillation. These compensatory consequences can cause episodes of tachycardia.
Atrial fibrillation is an important consequence of sinus nodal dysfunction. In most cases, it is caused by anomalies in the left atrium, e.g., hemodynamic overload from hypertensive cardiac disease. However, the sinus node is in the right atrium. Cor pulmonale is a possible cause of right atrial overload in patients with chronic obstructive pulmonary disease.
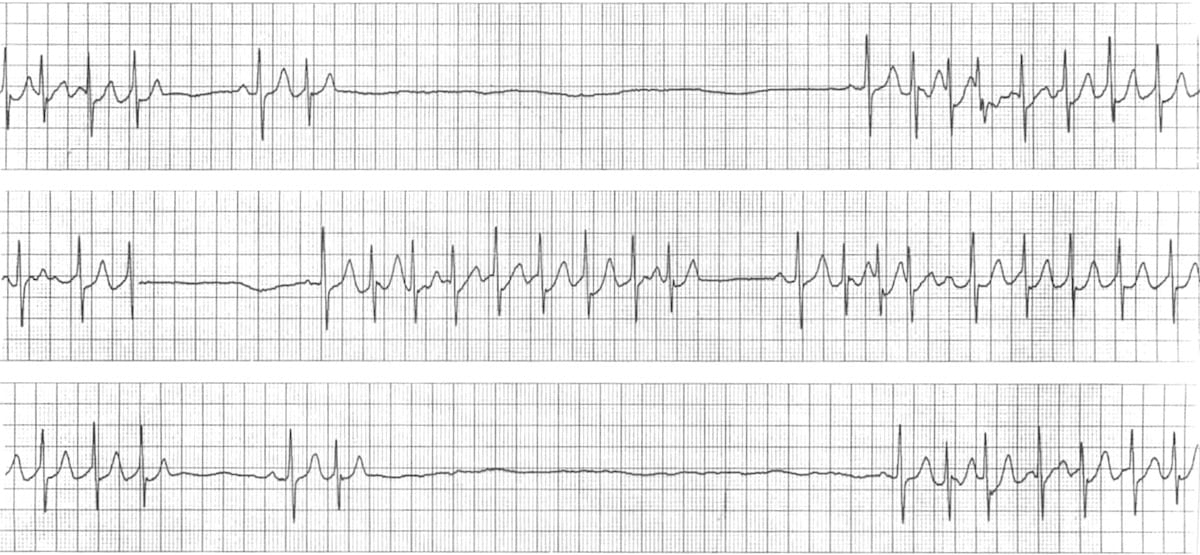
Bradycardia-Tachycardia Syndrome ECG 38
The ECG tracing in Figure 2 depicts bradycardia-tachycardia syndrome. Runs of tachycardia are followed by long sinus pauses lasting up to 6 seconds. The sinus rate is slow at 40 bpm; next, it drops to 10 bpm, and then the sinus beats are followed by paroxysmal junctional tachycardia at a rate of 140 bpm.
Atrioventricular Node and Bundle Branches In Sinus Node Dysfunction
The AV node can cause sinus node dysfunction when there is a sinoatrial block or sinus standstill. About 16% of patients diagnosed with sinoatrial node dysfunction have AV block and bundle-branch block.
37 Burns E. Sinus node dysfunction (sick sinus syndrome). Life in the fastlane website. Accessed September 24, 2020.
https://litfl.com/wp-content/uploads/2018/08/ECG-Sinus-Arrest-1-strip-3.jpg
38 Burns E. Sinus node dysfunction (sick sinus syndrome). Life in the fastlane website. Accessed September 24, 2020.
https://litfl.com/wp-content/uploads/2018/08/Brady-Tachy-Brady-Syndrome.jpg