Pacemaker Electrocardiogram
Pacemakers are implanted intravenously through the subclavian vein, and an electrode is placed over the right ventricle. Thirty percent of patients may have an extra electrode placed over the right atrium.
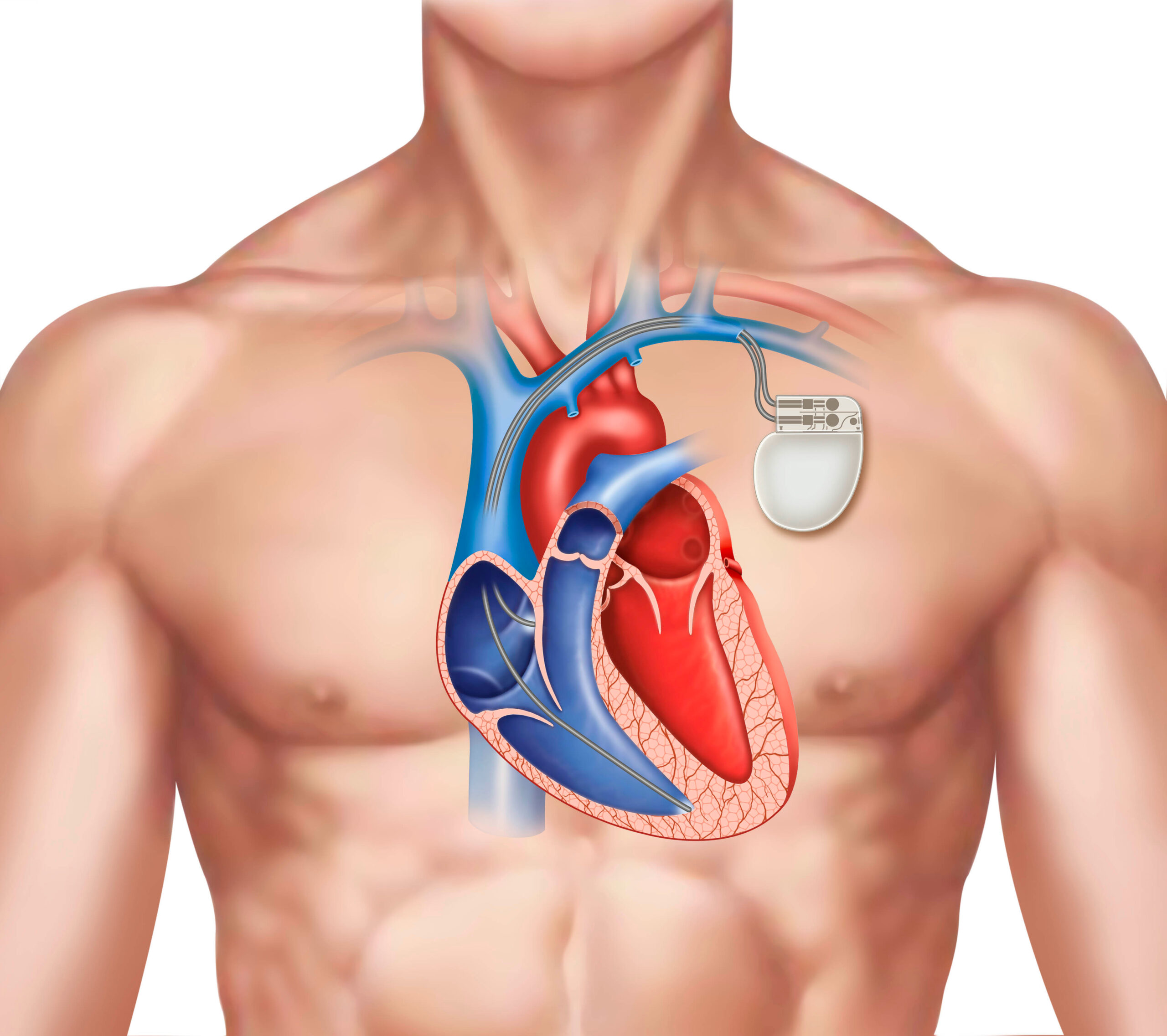
Pacemaker and Electrode Placement
In standard ventricular pacing, the right ventricle is stimulated before the left ventricle. A latency period occurs over the septum, which shows as a left bundle-branch block pattern on ECG. The depolarization and repolarization patterns are uniform throughout the limb leads.
Broad R waves appear in limb leads I and aVL, with a wide QRS complex in leads II, III, and aVF. In the precordial leads, a positive QRS deflection in V5 and V6 may be missed. This is a typical finding in left bundle-branch block aberration with a supraventricular rhythm.
Directly after a pacemaker stimulus (represented by a “spike” on ECG), a QS complex is seen in precordial leads V1 through V5, and an rS complex is seen in V6. The placement of the pacemaker lead within the right ventricle may show a rare Rs pattern in precordial lead V1. This pattern is never seen in left bundle-branch block aberration.
In rare instances, a surgeon may opt to place the pacemaker electrode in the epicardium of the left ventricle. This is done in special cases, such as in patients with severe tricuspid incompetence. When performed this way, the left ventricle is activated prior to the right ventricle. A right bundle-branch block pattern is expected.
A broad Q or QS wave appears in the inferior and anteroseptal leads, mimicking an infarction pattern. A wide QRS complex may also be present. The pacemaker spike has a greater amplitude because it is unipolar. However, if the generator output is set low (2.0–2.5 volts), then the pacemaker spike may be missed.