Atrial Tachycardias
Atrial tachycardias are differentiated by the morphology of the P wave, the atrial rate, AV conduction, the length of the arrhythmia, hemodynamic effects, the electrophysiologic mechanism, and the cause of the arrhythmia.
All P waves naturally precede the QRS complex because the origin of the impulse is atrial. The most striking characteristic of atrial tachycardia is the morphology of the P wave, which differs in appearance from the normal sinus P wave. Most atrial tachycardias have a regular rhythm.
Classification of Atrial Tachycardia
- “salvos” of PABs
- focal atrial tachycardia
- atrial reentry tachycardia
- repetitive paroxysmal atrial tachycardia
- paroxysmal atrial tachycardia
- left atrial tachycardia
- multifocal atrial tachycardia
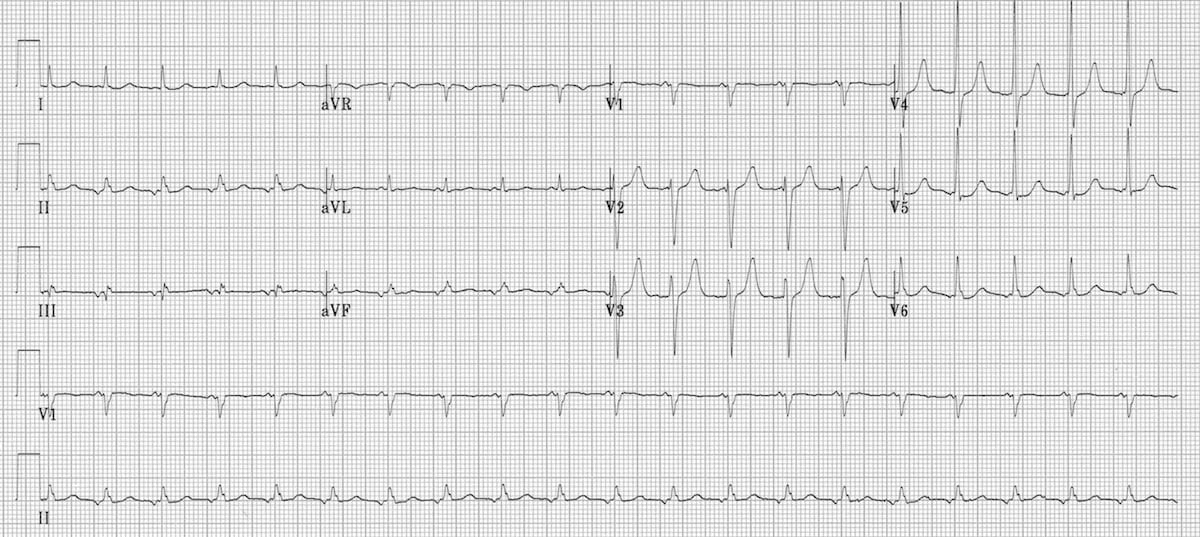
Ectopic Atrial Tachycardia ECG 31
The ECG in figure 1 shows a narrow complex tachycardia with a rate of 120 bpm. The P wave is abnormal and upright in precordial lead V1 and inverted in leads II, III, and aVF.
Salvos of Premature Atrial Contractions
A salvo of PABs is present with three to five PACs occurring in succession in the setting of tachycardia. Patients with this condition are often without symptoms. Salvos of PABs are without atrial fibrillation or atrial flutter.
Focal Atrial Tachycardia
Focal atrial tachycardias result from ectopic impulses from a single site within the right atrium. Focal atrial tachycardias may be automatic, triggered, or caused by micro-reentrant aberrations. These impulse etiologies cannot be distinguished by ECG tracings.
Focal atrial tachycardias are paroxysmal and usually self-limited, but sometimes patients develop incessant atrial tachycardia, which can last for weeks or months and may eventually lead to left ventricular dysfunction. Over time, ventricular dilatation and heart failure may occur. The effects can be reversed after catheter ablation of the aberrant focus. Incessant atrial tachycardia is seen in younger patients.
The P waves in focal atrial tachycardia do not change, and the ECG does not give many clues as to the site of impulse generation. However, positive P waves in leads III and aVF denote a focus in the superior aspect of the atria. A negative P wave in leads III and aVF denotes a focus in the inferior aspect of the atria.
The rhythm is regular, and the tachycardia may last up to 30 seconds at a rate of 100–150 bpm. A rate over 180 bpm is rare.
At the start of the tachycardia, an aberrant conduction pattern such as a right bundle-branch block can be observed, but that usually disappears after several beats. When a longer run of tachycardia occurs, rate variation may be observed. Alterations of depolarization may persist after the tachycardia resolves, but only for a few hours.
Vagal maneuvers do not influence the atrial rate but can induce second-degree AV block. Some patients respond to adenosine, but the most effective therapy is catheter ablation of the aberrant focus.
Related Video – ECG Rhythm Review – Atrial Tachycardia
Atrial Reentry Tachycardia
Cardiac arrhythmias are caused by either enhanced automaticity, triggered activity, or reentry. Reentry is caused by a circuit within the myocardium and persists when the propagating impulse does not halt, despite normal activation in the SA node. It causes continuous activity around the circuit, which excites the heart even though the refractory period has ended. Atrial fibrillation, atrial flutter, atrioventricular nodal reentry, and atrioventricular reentry tachycardia are caused by the above-mentioned electrophysiology.
The reentry circuit for atrial reentry tachycardia has two distinct intra-atrial functional pathways.
- The P wave morphology differs from the sinus P wave.
- The P wave can be positive or negative in limb leads III and aVF.
- The P wave is preceded by a premature atrial beat.
- P wave morphology changes according to variations in the circuit (unlike the persistent morphology in focal atrial tachycardia).
- A “warming up effect” characterized by an increase in HR occurs just prior to the event.
- The heart rate is faster compared to focal atrial tachycardia, with rates of up to 240 bpm.
The incidence of atrial reentry tachycardia is 6% in patients diagnosed with paroxysmal supraventricular tachycardia. Atrial reentry tachycardia is also found in patients with congenital heart disease as well as some healthy patients. Treatment with adenosine and vagal maneuvers is likely to be unsuccessful.
Repetitive Paroxysmal Atrial Tachycardia
Repetitive paroxysmal atrial tachycardia is an irregular atrial tachycardia with a rate of 130–150 bpm that occurs suddenly. It can occur incessantly with frequent interruption by sinus beats. This condition is very rare, and the treatment is usually directed to the underlying cardiac disease.
Paroxysmal Atrial Tachycardia with AV Block
Paroxysmal atrial tachycardia with AV block mostly involves second-degree AV block (as opposed to first- and third-degree AV block). Paroxysmal atrial tachycardia is thought to be the result of an ectopic focus.
- The rate is between 150 bpm and 200 bpm.
- The tachycardia occurs with either a 2:1 or 3:1 AV block.
- The 2:1 AV block rarely displays the Wenckebach phenomenon.
- The atrial rhythm is regularly irregular, noted by different manifestations of the P wave in ECG.
- The tachycardia results in an irregular ventricular rhythm.
- An AV-blocked P wave appears after a QRS complex that was produced by a normally conducted P wave.
- The AV-blocked P wave is not followed by a QRS complex.
- This blocked P wave is then followed up by a normally conducted P wave.
Paroxysmal atrial tachycardia with AV block is difficult to differentiate from type 2 (uncommon) atrial flutter with 2:1 AV block. Neither has a saw-tooth appearance. The isoelectric line between the flutter waves is preserved.
Clinically, the ventricular rate in atrial flutter can be slowed with digitalis drugs. Conversely, the arrhythmia in paroxysmal atrial tachycardia with AV block is caused by digitalis toxicity.
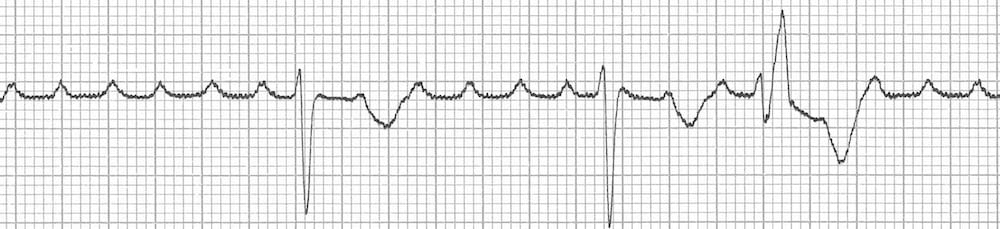
Paroxysmal Atrial Tachycardia With Atrioventricular Block ECG 32
The ECG in figure 2 is from a patient with digoxin toxicity. The patient’s ECG shows atrial tachycardia with an atrial rate of 250 bpm and a high-grade 5:1/3:1 AV block with PVCs. Hemodynamic instability will not be evident unless the ventricular rate exceeds 220 bpm.
Left Atrial Tachycardia
Left atrial tachycardia causes a very high cardiac rate of 150–200 bpm or higher. Patients with left atrial tachycardia do develop hemodynamic instability. The ECG shows negative P waves in precordial leads I and aVL. Positive P waves are seen in V1.
The positive P wave in lead V1 is caused by abnormal activation of both atria with both of its vectors projected anteriorly. To treat these patients, clinicians must determine if the focal origin comes from the left or right atrium and direct catheter ablation to the ectopic focus.
Multifocal Atrial Tachycardia
Multifocal atrial tachycardia is a chaotic arrhythmia. When the rate is 110–150 bpm, it is termed chaotic atrial tachycardia. When the rate is < 100 bpm, it is classified as a chaotic atrial mechanism.
Multifocal atrial tachycardia shows at least three different morphologies of the P wave in one lead. It has variable P-P intervals, P-R intervals, and R-R intervals because there is not a dominant atrial focus of impulse conduction. It is readily differentiated from sinus rhythm with salvos of PABs.
First-degree AV-block and singular AV junction escape beats can occur. The arrhythmia can last for a few minutes to days. It can progress into atrial flutter or atrial fibrillation. Patients may develop hemodynamic instability. Patients diagnosed with comorbidities such as COPD are prone to poor prognosis.
Patients who have comorbidities and multifocal atrial tachycardia have a 50% of survival over 6 months.
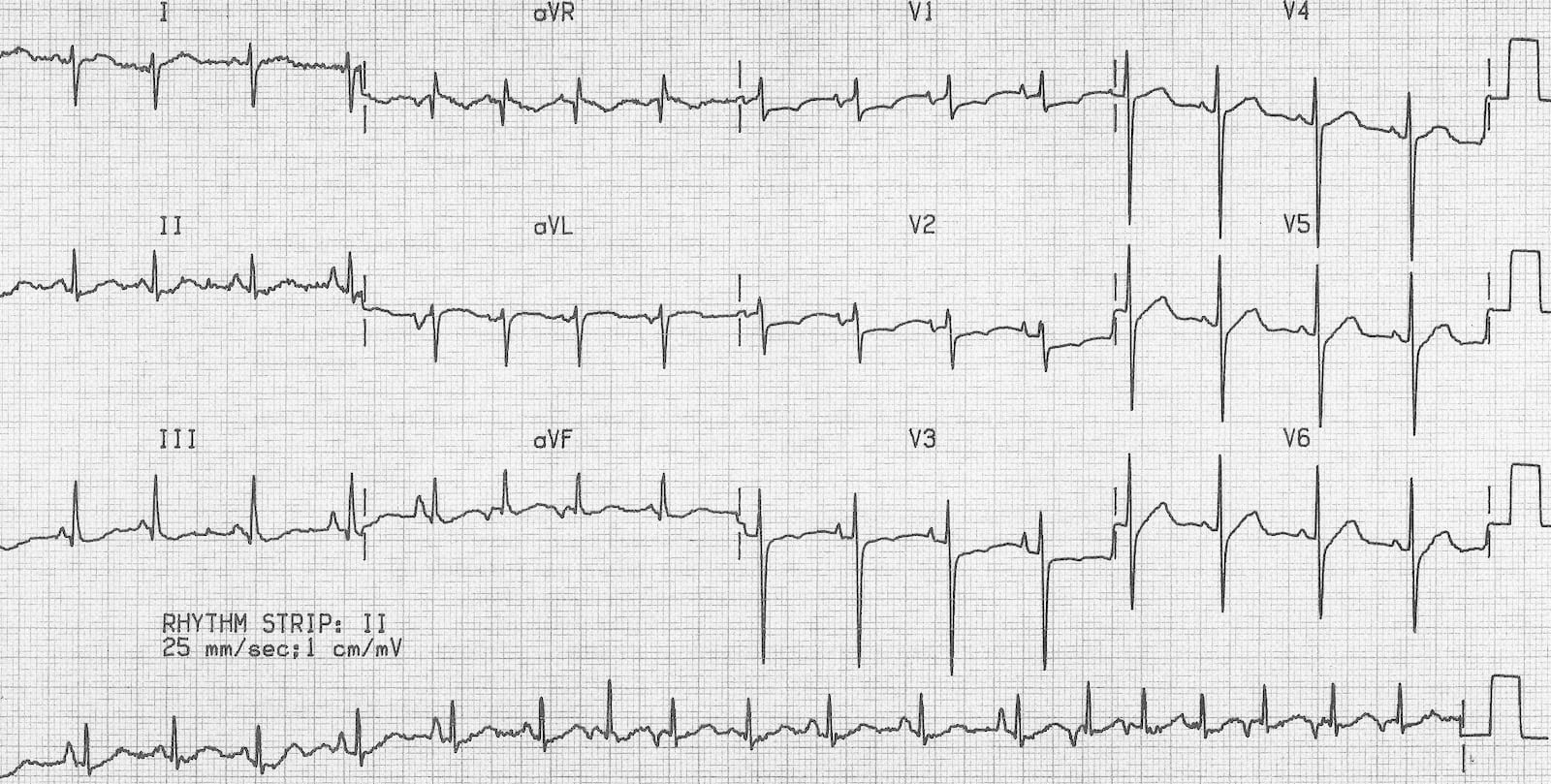
Multifocal Atrial Tachycardia ECG 33
The ECG above is an example of multifocal atrial tachycardia from a patient with COPD. There is a rapid, irregular rhythm with multiple P wave morphologies. The ECG also shows right axis deviation and a positive Sokolow index due to a dominant R wave in V1 with a deep S wave in V6 — indications of RVH, probably from cor pulmonale due to COPD.
31 Burns E. Atrial tachycardia. Life in the fastlane website. Accessed August 20, 2020.
https://litfl.com/wp-content/uploads/2018/08/ECG-Ectopic-atrial-tachycardia-inverted-p-waves.jpg
32 Burns E. Digoxin toxicity. Life in the fastlane website. Accessed August 20, 2020.
https://litfl.com/wp-content/uploads/2018/08/Digoxin-toxicity-PAT-with-block-PVC.jpg
33 Burns E. Multifocal atrial tachycardia. Life in the fastlane website. Accessed September 1, 2020.
https://litfl.com/wp-content/uploads/2018/08/Multifocal-Atrial-Tachycardia-MAT-COPD-2.jpg.