Introduction
Care following cardiac arrest is vital for ensuring good patient outcomes. Studies reveal that overall survival is increased in hospitals that manage more cases of cardiac arrest. The majority of cardiac arrests occur in the first 24 hours after the event. During care following arrest, there is the opportunity to optimize hemodynamic status while ensuring that the organ systems recover adequately to prevent short-term mortality and minimize long-term morbidity. Care following arrest must assess for and manage neurological, metabolic, and hemodynamic concerns that usually occur soon after the return of spontaneous circulation (ROSC). Health care providers must be aware that ROSC does not signify a return to normal functioning or guaranteed survival. Rather patients achieving ROSC will often still require the support of many of the organ systems with intravenous medications and invasive medical devices. This is also a time that temperature management, such as induced medical hypothermia, will play a role. Cardiovascular disorder and brain injury are the key determinants of survival following cardiac arrest.
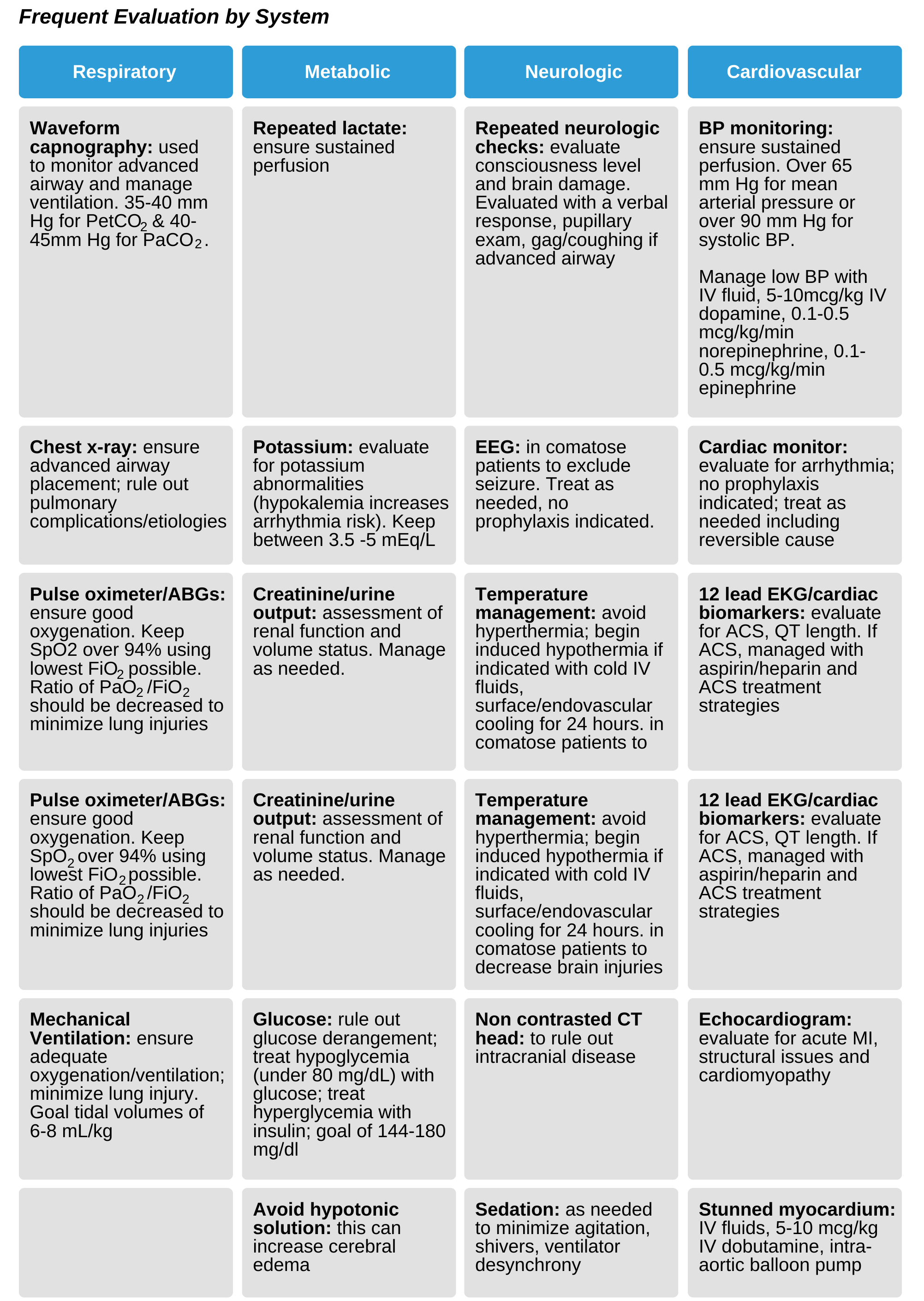
Well-rounded and structured care following ROSC is important for supporting the multiple organ systems as well as preventing future complications. Care should incorporate temperature management, cardiovascular optimization, reperfusion strategies for ACS, neurologic specialty care, and intensive care assessment. Underlying causes must be addressed, and reevaluation of patient status is necessary.