Neurologic Prognosis following Coma
Neurologic Prognosis following Coma
Post-arrest care is successful when patients can return to their baseline function. On the other hand, negative outcomes include death, vegetative state, and inability to perform activities of daily living independently at 6 months.
However, no single parameter of arrest (i.e., length of arrest, initial rhythm, the timing of CPR) can predict long-term outcomes. Even in the early ROSC period, the neurologic assessment may not be predictive of long-term outcomes.
Following ROSC after cardiac arrest, the clinicians are responsible for determining the patient’s neurological status. The team must understand the assessments that will aid in developing a realistic prognosis for the patient.
The team uses multiple modalities in this process:
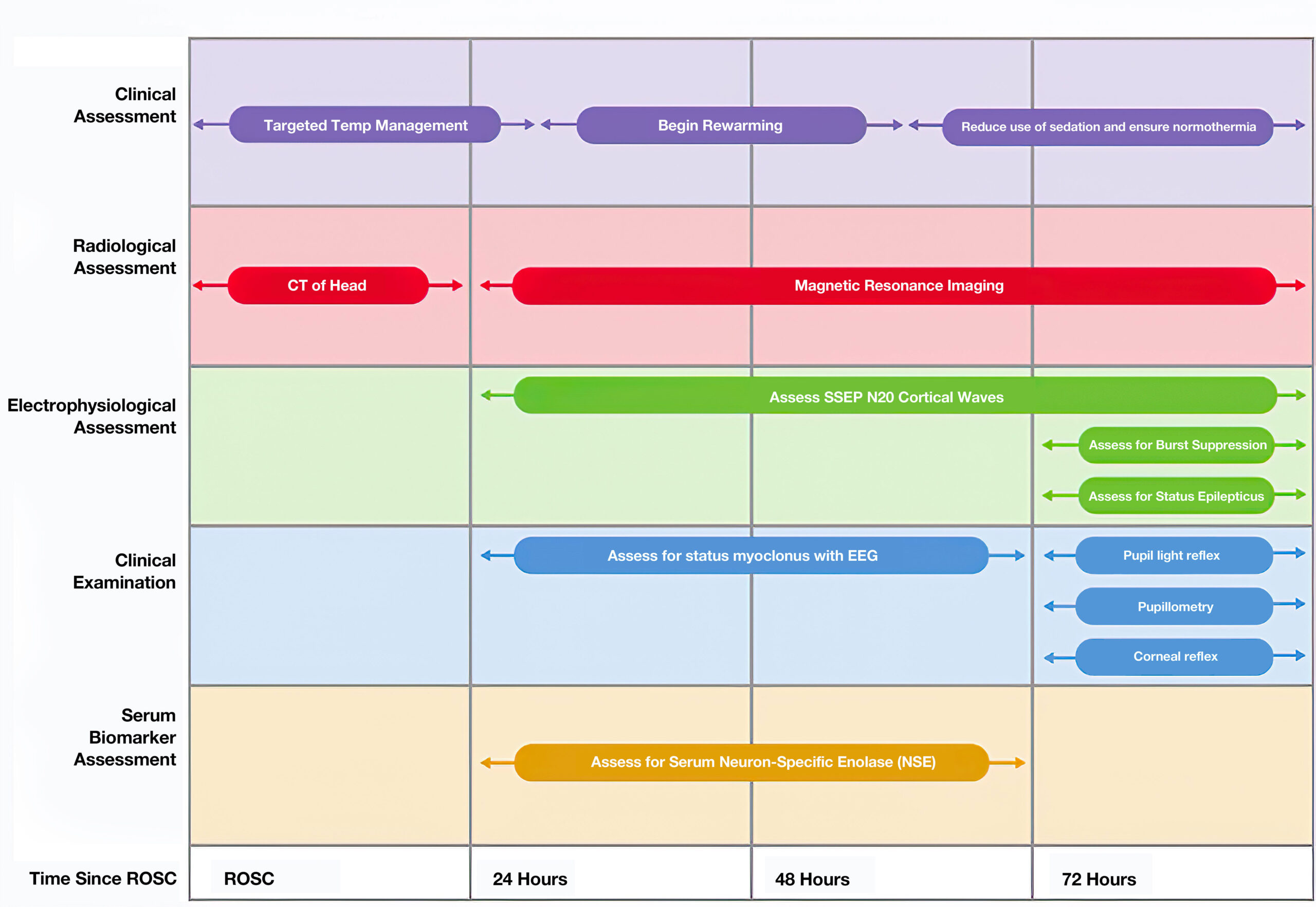
Timeline Proceeding ROSC
- Clinical Assessment begins at the time of ROSC and continues throughout the patient’s stay.The assessments include:
- Targeted temperature management (TTM), beginning at ROSC and continuing for approximately 36 hours.
- After TTM, the team begins rewarming the patient. This process continues until 60 hours following ROSC.
- At that time, the team ensures normothermia and begins to reduce sedation.
- Radiological Assessment includes:
- CT of the head at the time of ROSC and as needed for 24 hours.
- After 24 hours, MRI is a better tool for predicting neurological outcomes.
- Electrophysiological Assessment includes:
- Assessment of SSEP N20 cortical waves beginning at 24 hours after ROSC.
- Burst suppression and status epilepticus assessment beginning at 72 hours after ROSC.
- Clinical Examination includes:
- Continual EEG assessment for status myoclonus beginning at 24 hours after ROSC.
- Assessment of pupillary light reflex, pupillometry, and corneal reflex beginning at 72 hours after ROSC.
- Serum Biomarker Assessment includes assessment for serum neuron-specific enzyme (NSE) at 24 hours after ROSC.
Long-term outcomes are difficult to predict and require neurologic expertise. The patient’s baseline function and comorbidities are included in this assessment, as well as multiple assessments, including neurologic exam, EEG, and laboratory evaluation. Overall, some guidelines for assessment in patients include:
-
- Lack of pupillary reflex at 72 hours following rewarming/ROSC is a negative predictor. (The false positive rate is 1% with 95% confidence interval between 1-3%; Class I, Evidence level B-NR)
- Do not use a lack of motor movement or extensor posture alone for predictive purposes. (The false positive rate is 10% with 95% confidence interval between 7-15%; Class III; harmful, Evidence level B-NR)
- Do not use myoclonus presence (separate from status myoclonus) for predictive purposes. (The false positive rate is 5-11% with 95% confidence interval between 3-26%; Class III; harmful, Evidence level B-NR)
- Status myoclonus used in combination with other testing at 72 hours following rewarming/ROSC is a negative predictor. (The false positive rate is 0% with 95% confidence interval between 0-3%; Class IIb, Evidence level B-NR)
- Lack of a reactive EEG to stimuli or persisting EEG burst suppression at 72 hours following rewarming/ROSC is a negative predictor. (The false positive rate is 0% with 95% confidence interval between 0-3%; Class IIb, Evidence level B-NR)
- Persisting and refractory status epilepticus without reactive EEG at 72 hours following rewarming/ROSC is a negative predictor. (Class IIb, Evidence level B-NR).
- In comatose patients not undergoing temperature management, persisting EEG burst suppression used in combination with other testing at 72 hours following ROSC is a negative predictor. (The false positive rate is 0% with 95% confidence interval between 0-11%; Class IIb, Evidence level B-NR)
- In all patients, regardless of temperature management, the bilateral lack of N20 somatosensory evoked potential waves between 24-72 hours following rewarming (or ROSC) is a negative predictor. (The false positive rate is 1% with 95% confidence interval between 0-3%; Class IIa, Evidence level B-NR)
- Do not use markers, including neuron-specific enolase or S-100B alone, for predictive purposes. (Class III; harmful, Evidence level C-LD).
- Markers, including neuron-specific enolase or S-100B used in combination with other testing at 48-72 hours following rewarming/ROSCH is a negative predictor. (Class IIb, Evidence level B-NR).Repeated elevation further increases negative prediction. (Class IIb, Evidence level C-LD).
- Brain MRI findings of significant diffusion restriction in combination with other testing at 2-6 days following rewarming/ROSC is a negative predictor. (Class IIb, Evidence level B-NR).