Introduction
Introduction
The pregnant patient presents a challenge as there are actually two patients in one- the mother and fetus. However, maternal survival usually is in line with fetal survival. Clinicians must be aware of pregnancy-associated physiologic changes when caring for the pregnant woman.
Numerous changes alter physiology in pregnancy. Due to the implications, few randomized trials are done on pregnant patients. As a result, there is no high-quality evidence. Guidelines are based on the little research available on pregnancy-related resuscitation, clinical consensus, and knowledge of pregnancy physiology.

Clinicians must be aware of a pregnant woman’s pregnancy-associated physiologic changes.
Luckily cardiac emergency in pregnancy is rare. Cardiac arrest in pregnancy occurs in 1 of 12000 delivery admissions; however, the deaths associated with cardiac arrest does appear to be increasing from 7.2 to 17.8 in 100,000 deliveries between 1987 and 2009.
There are certain important physiological changes during pregnancy that can affect resuscitation efforts.
Respiratory Changes
- 20% increased oxygen consumption
- Increased minute ventilation and tidal volume to mitigate the increased oxygen consumption
- Respiratory alkalosis with mild metabolic acidosis compensation. The mild hypocapnia (PaCO2 of 28-32 mm Hg) is needed to allow the fetus to release carbon dioxide. Any added acid insult will be difficult to compensate for due to the baseline respiratory alkalosis.
- Elevated diaphragm leading to diminished functional residual capacities (FRC) and volume (FRV). This can increase the risk for sudden desaturation with hypoxia
- Anteriorly displaced larynx with increased blood flow and edema
Cardiovascular Changes
- 40% increased plasma volume and cardiac output. Decreasing cardiac output occurs towards the end of pregnancy (late 3rd trimester), especially in the supine position.
- Vascular resistance decreases (pulmonary and systemic)
- After 20 week gestation, the uterus compresses on the aorta and inferior vena cava (IVC), leading to decreased venous return as well as blood flow systemically. This can occasionally occur earlier in gestation.
- Decreased venous return leads to lower stroke volume and cardiac output
- Physiologic anemia leads to reduced oxygen arterial content in the setting of normal PaO2 or SpO2.
Gastrointestinal Changes
- The incompetence of the gastroesophageal sphincter increases reflux disease at baseline and increased aspiration risk if unconscious.
The other patient
Always be conscious of the fetus as a patient. At 20 weeks gestation, the fetal size can adversely affect resuscitation effects. The fetus becomes potentially viable outside the womb at 23 weeks gestation.
Considering Cesarean Section (C/S)
Cesarean section reverses aortic compression and aid efforts at resuscitation, so in the second half of pregnancy, it may be considered in resuscitation efforts. The little research done shows that over half of women will have ROSC following the cesarean section, and there was no associated worsening in maternal status. However, due to the heterogeneity of cases, the preferred timing for this treatment. Maternal survival is documented as much as 15 minutes following arrest. In comparison, neonatal survival is documented as much as 30 minutes following arrest.
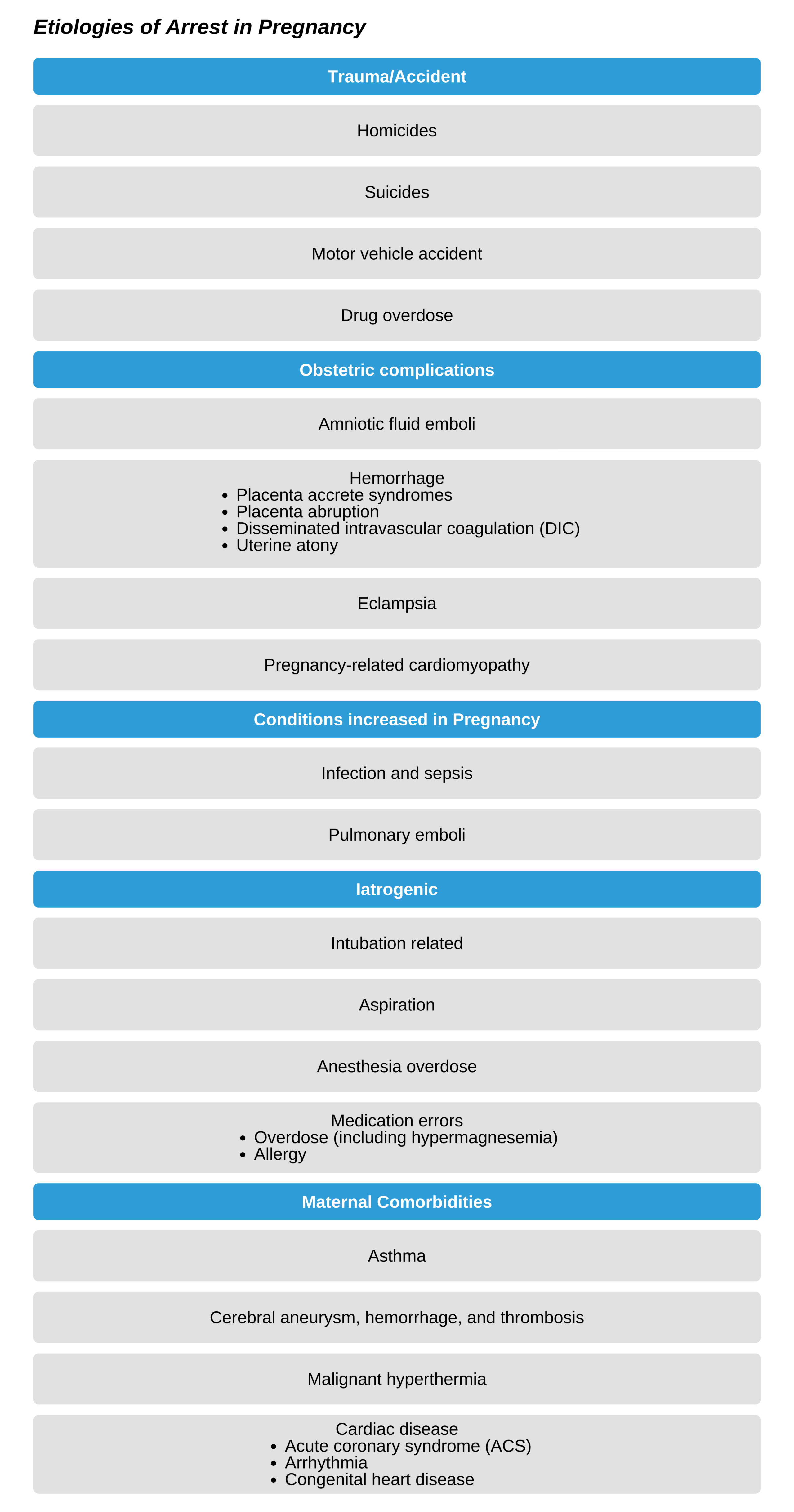
Etiologies of Arrest in Pregnancy
There are several causes of pregnancy-associated arrest. The most common underlying etiology is heart disease, and the deaths associated with the cause have been increasing. The most common cardiac concerns are sudden death syndrome, acute MI, cardiomyopathy, and aortic dissection. Importantly there is also a risk in the postpartum period in patients with underlying cardiac disease.
Managing pregnancy-associated Cardiac Arrest
Immediate care should include:
- Left lateral decubitus positioning to minimize IVC compression. Positioning alone can incite arrest in a severely ill patient.
- 100% oxygen supplementation
- IV fluid bolus. Ensure access is above the level of the diaphragm
- Evaluate for hypotension. In pregnancy, hypotension is defined as systolic BP under 100mm Hg or under 80% baseline. Maternal hypotension negatively affects perfusion of the placenta.
- Evaluate for reversible causes as well as underlying comorbidities.

Left Lateral Decubitus Positioning