Using Pacing
Using Pacing
TCP is a temporizing measure until transvenous pacing is initiated in patients with unstable bradycardias who do not improve with atropine. TCP can also be used in patients with acute MI who have signs of conduction pathway abnormalities such as new bundle branch or bifascicular blocks. For these patients, the team should obtain cardiac consultation as they will need complex management. Additional information can be obtained by reviewing the ACC/AHA Guidelines for treating STEMI at https://www.ahajournals.org/doi/10.1161/circ.110.9.e82.
Related Video: Transcutaneous Pacing
Pacing the heart
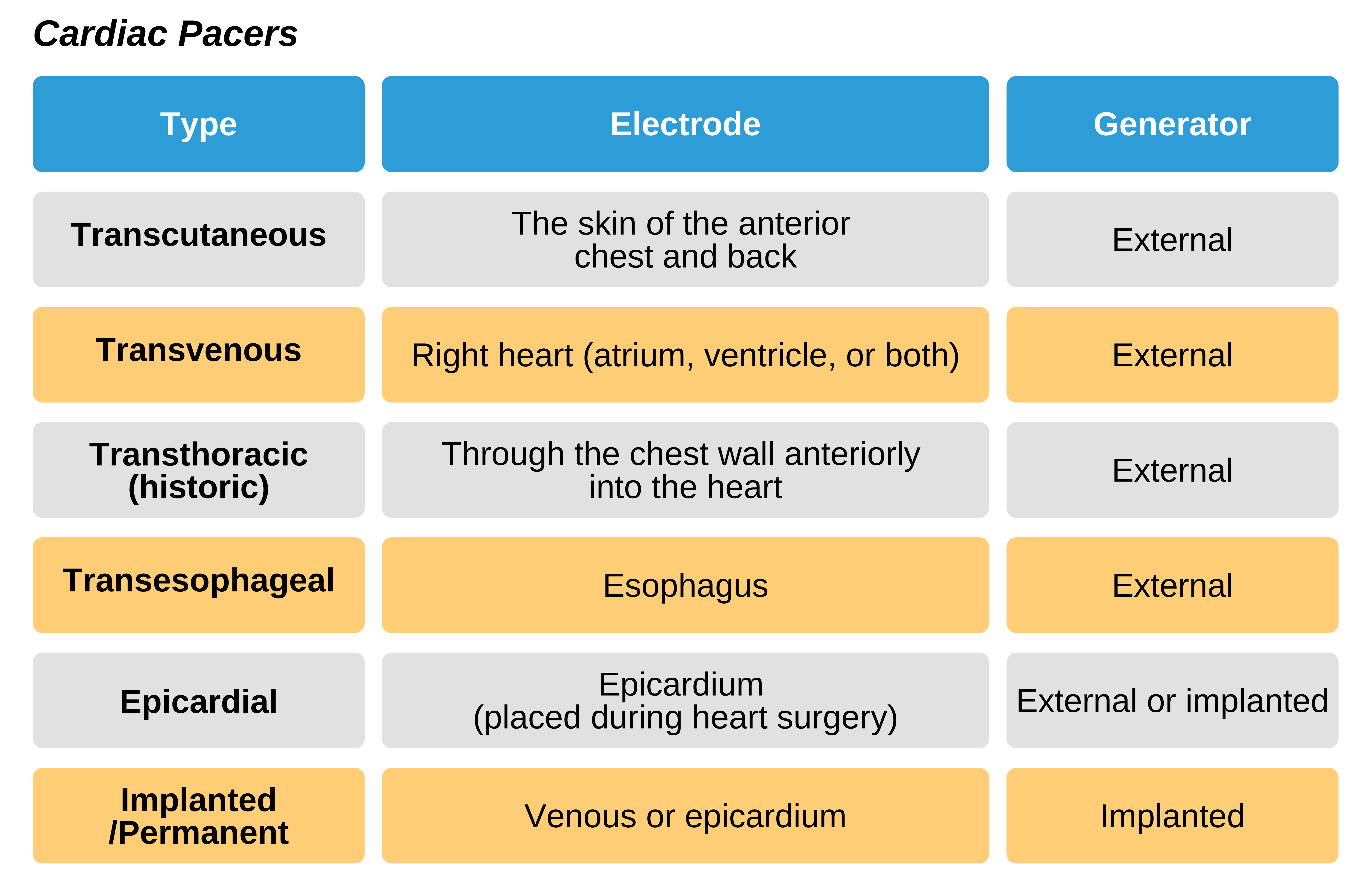
Cardiac pacing has been utilized since the 1800s and has gone through considerable evolution. Pacing uses electrical impulses originating from electrodes to cause depolarization of the cardiac myocytes and subsequent contractions. TCP is performed via skin electrodes, while transvenous pacing is performed via electrodes passed intravenously into the right heart or (less commonly) the heart surface.
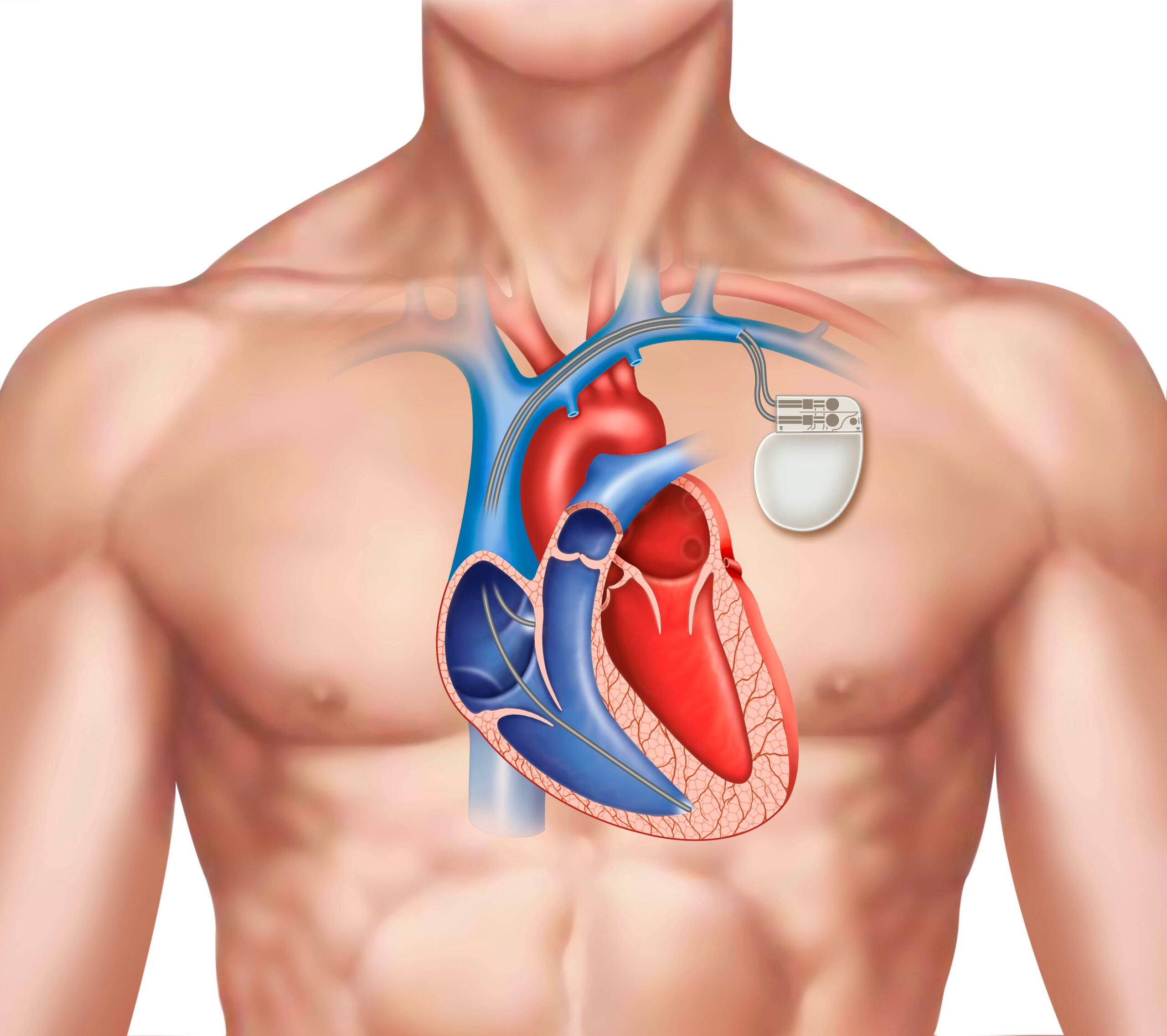
Pacemaker Illustration
A pulse generator is used to initiate pacemaker activity and can be external or implanted surgically as a permanent pacemaker. Temporary transvenous pacing utilizes an external pacemaker. Typically, this is used until the bradycardia resolves or the patient undergoes surgical implantation of a permanent pacemaker. Responders should be aware that permanent pacemakers can cause ECG artifacts that can be mistaken for arrhythmias.
The increasing availability of transcutaneous pacers over the past three decades ensures they are more available when needed for emergency treatment.
Emergency and Temporizing Pacing
Emergency Pacers
In an emergency, TCP is used for managing symptomatic bradycardia. It is painful and less reliable than transvenous pacing and should be used only until transvenous pacing is available.
TCP may also be utilized for stable patients with significant conduction pathway abnormalities that are at risk for deteriorating (e.g., asymptomatic Mobitz II 2nd-degree block or narrow QRS 3rd-degree block). It is a temporary measure and should not be used for long-term management.
In patients managed with TCP, close monitoring for response is necessary. The goal heart rate should be the lowest possible required for adequate perfusion and resolution of symptoms as increasing the heart rate leads to increased oxygen use. For most patients, a rate between 60 and 70 bpm is reasonable. It is vital to understand that pacing will only improve symptoms due to bradycardia.
Alert patients may have significant pain from TCP due to the contraction of skeletal muscle with each beat. Patients will also need to be prepared for transvenous pacing, regardless of the efficacy of TCP. Cardiac consultation is indicated in these patients.
- Electrodes should be placed to improve the chance that the ventricle is captured. Typically, the anterior-posterior placement is best as long as this effectively ensures the heart is in between the two electrodes. Options include right scapular and left parasternal placement as well as left scapular and left parasternal placement. If a particular positioning is not effective, one or both electrodes can be moved.
- Both electrical and mechanical capturing must be ensured. There may be TCP artifact on surface ECG that can erroneously simulate ventricle capture (QRS) that is not occurring. A QRS complex followed by a repolarizing T wave indicates capture. If a T wave does not follow the QRS, capture is not happening, and the team must either increase TCP output or move the electrodes.
- Assessing for the pulse after TCP is important. However, the associated contraction of skeletal muscle can make this difficult. Typically, feeling for the femoral pulse is more reliable due to its distant location from the pacer.
- The patient should be reassessed for symptoms and perfusion status.
- The team should always look for and manage the underlying cause of the bradycardia.
As TCP may be painful, adequate analgesia or sedation is required. Specific sedatives can negatively affect the cardiac rhythm by further slowing it. When considering analgesics and sedation, the following pathway may be a beneficial approach:
- IV benzodiazepines are used to decrease anxiety and relax the muscles.
- IV narcotic are given for pain control.
- If significant sedation is needed, the patient may require an advanced airway for ventilatory support.
- Cardiology should be consulted when transvenous pacing is needed.
Standby Pacers
Standby pacers are used for those patients at high risk for needing pacing in the future. Often these patients have stable vital signs, but they have significant conduction pathway abnormalities that are likely to deteriorate. Their ECG findings suggest a block at locations associated with a poor prognosis and an extensive acute MI that may lead to significant cardiac dysfunction. Reperfusion of the coronary vessels is vital in indicated patients as well as TCP or transvenous pacing.
Typically, TCP is the best option for patients in this category who are at risk for advanced heart block. It may also be used in patients with conduction pathway abnormalities (such as left bundle branch or bifascicular block in association with 1st-degree heart block) who require surgical intervention but who are not candidates for transvenous pacing because the likelihood of deterioration into unstable bradycardia is not enough to warrant the risks of placement. Instead, TCP can be used on standby in case a heart block develops during a surgical intervention. When using TCP in these situations, it serves as temporary management until transvenous pacing is available.
Pacing in Bradycardia or Asystole without a Pulse
Research has evaluated the role of pacers in bradycardic and asystolic patients with no pulse. Some research indicates a benefit in those patients who receive pacing within 10 minutes of cardiac arrest, while others show no short- (survival to admission) or long-term (survival to discharge) benefits.
Research does not indicate that TCP improves outcomes in patients with symptomatic bradycardia compared to adrenergic medications. Additionally, there does not seem to be a benefit for out-of-hospital TCP in patients with cardiac arrest due to asystole or new-onset asystole following defibrillation. Randomized controlled trials of CPR in combination with pacing do not improve outcomes in post-defibrillator asystole.
Pacing in Overdose-Associated Arrest
On the other hand, patients with cardiac arrest associated with a drug overdose may benefit from pacing as it can be temporizing management for unstable bradycardia or pulseless electrical activity (PEA). Similarly, pacing may benefit patients with acid-base or electrolyte abnormalities. The similarities are that these patients usually have a normal heart that has been temporarily affected by the condition.
Since pacing can provide adequate myocyte contractions, it is life-preserving until the electrolyte or acid-base imbalance or drug overdose has been managed and the conduction pathway returns to its normal function.
Pacing Contraindications
Patients who have profound hypothermia are usually not candidates for pacing. In this case, bradycardia is physiologic as the metabolic rate responds by slowing to match the hypothermic state. Additionally, hypothermic myocytes are at risk for pacing-associated ventricular fibrillation that may be refractory to defibrillation. In such patients, pacing may not be appropriate.
Pacing does not improve survival for adults or children with witnessed OHCA. However, it may still be indicated in the case of bradycardia associated with congenital heart conditions, 3rd-degree block, sinus node abnormities, post-cardiac surgery dysfunction, and drug overdoses.
Administering Transcutaneous Pacing (TCP)
TCP allows cardiac stimulation via the administration of an electrical impulse through the chest wall into the cardiac muscle. It is also referred to as external or non-invasive pacing. TCP is not benign and does have some adverse effects. The skeletal muscle contractions can be uncomfortable for patients, and it may instigate ventricular arrhythmias.
TCP is useful in the emergency setting as it is easy to initiate and often readily available on external defibrillators. These devices have multipurpose electrodes that administer defibrillation, pacing, and monitor the ECG. It is important to note that the placement of a right and anterior subclavicular with a left apex chest electrode may not be effective for TCP. In this situation, the electrode placed on the right side should be moved to the back. TCP is also useful in patients receiving or who will need to receive fibrinolytics because no venipuncture is necessary.
Transcutaneous Pacing Pad Placements
TCP Equipment
As noted above, TCP devices are readily available both inside and outside of the hospital with standard defibrillators. These modern devices allow several output options. The features of TCPs include:
- Operational mode: fixed rate (i.e., asynchronous or nondemand) or demand mode
- Rate setting: ranges between 30 and 180 bpm
- Current output: ranges between 0 and 200 mA
- Pulse length: ranges between 20 and 40 ms. However, this is only monitored (via rectangular markers on the monitor) and not adjusted by the responder.
- Monitor blanking: stops the large electrical impulse caused by the pacemaker overshadowing the patient’s native ECG rhythm. This is a necessary feature as pacer electrical activity may easily obscure significant cardiac arrhythmias like VF that need defibrillation.
When using TCP, it is vital to ensure that capture is achievable and the patient can tolerate it. If there is too much pain, the clinician can administer benzodiazepines to decrease anxiety and relax the musculature along with narcotics for pain control.
Procedure for using TCP
- Pacer electrodes are placed on the chest in an anterior-posterior position with the anterior electrode left of the sternum at the location of maximal cardiac impulse and the posterior electrode either just to the right or left of the spine and between the patient’s shoulder blades. Chest and back hair can be removed as needed.
- The rate is set between 60 and 80 bpm.
- The current is set by beginning with the lowest current and increasing slowly until there is a pacer spike on the monitor and continued until pacing capture is noted.
- The ECG is monitored for visualization of electrical capture indicated by a QRS and T wave following each pacer spike.
- The captured ventricular depolarization will manifest a wide QRS and stable ST segment followed by a broad sloping (repolarizing) T wave in the opposite polarity (direction) to the QRS.
- A T wave must be visualized as this indicates true capture. A pacer spike and sloping potential afterward do not indicate true capture.
- Evaluate cardiac output and ventricular activity (i.e., mechanical capture) by assessing the patient’s blood pressure and pulse.
- Assessing for the pulse after TCP is important. However, the associated contraction of skeletal muscles can make this difficult. Typically, feeling for the femoral pulse is more reliable due to its distant location from the pacer.
- Pacing is continued with a higher output (usually 10% higher) than needed for electrical capture in order to balance reliable capture and patient comfort.
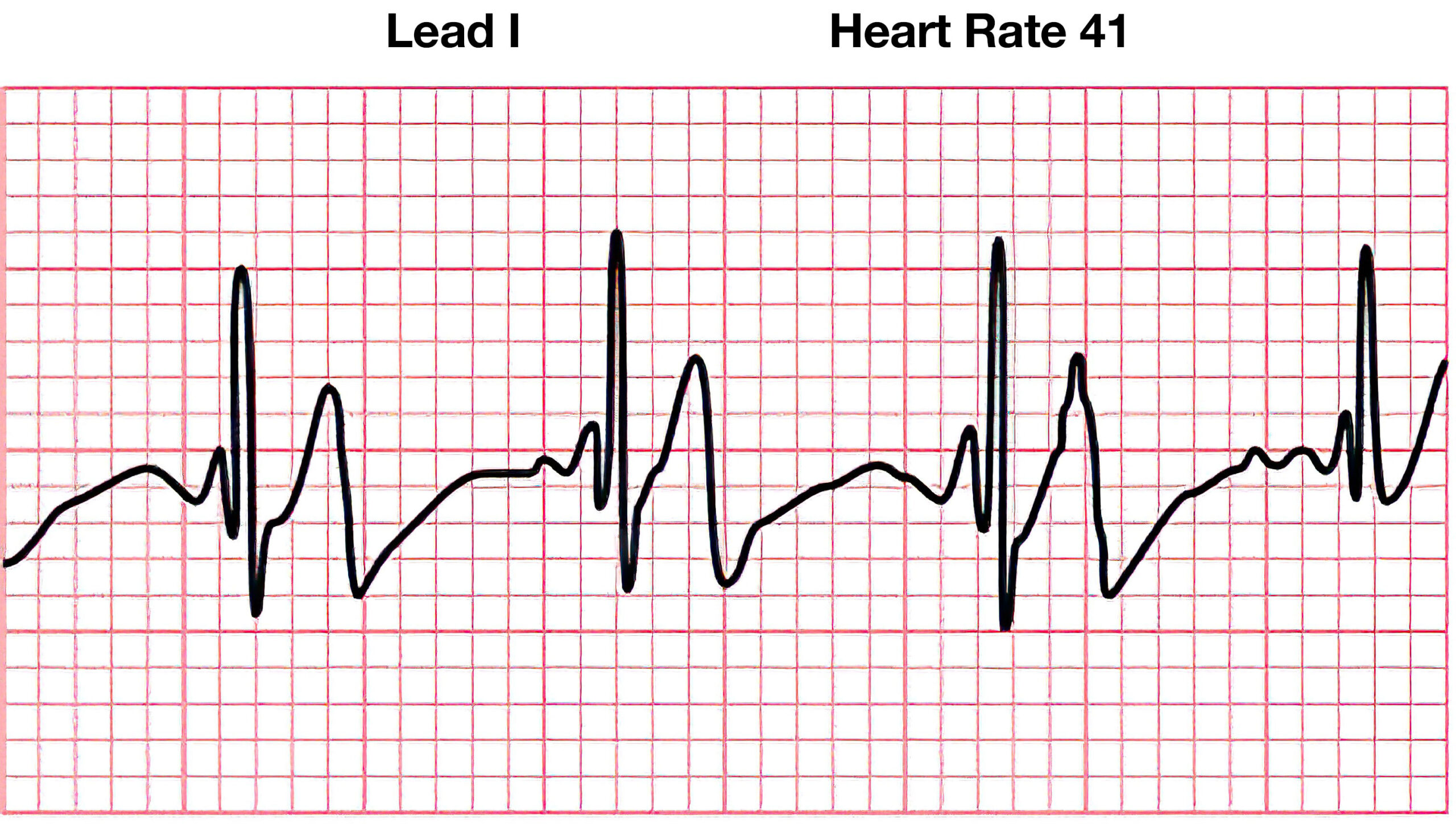
Initial Bradycardia Before TCP
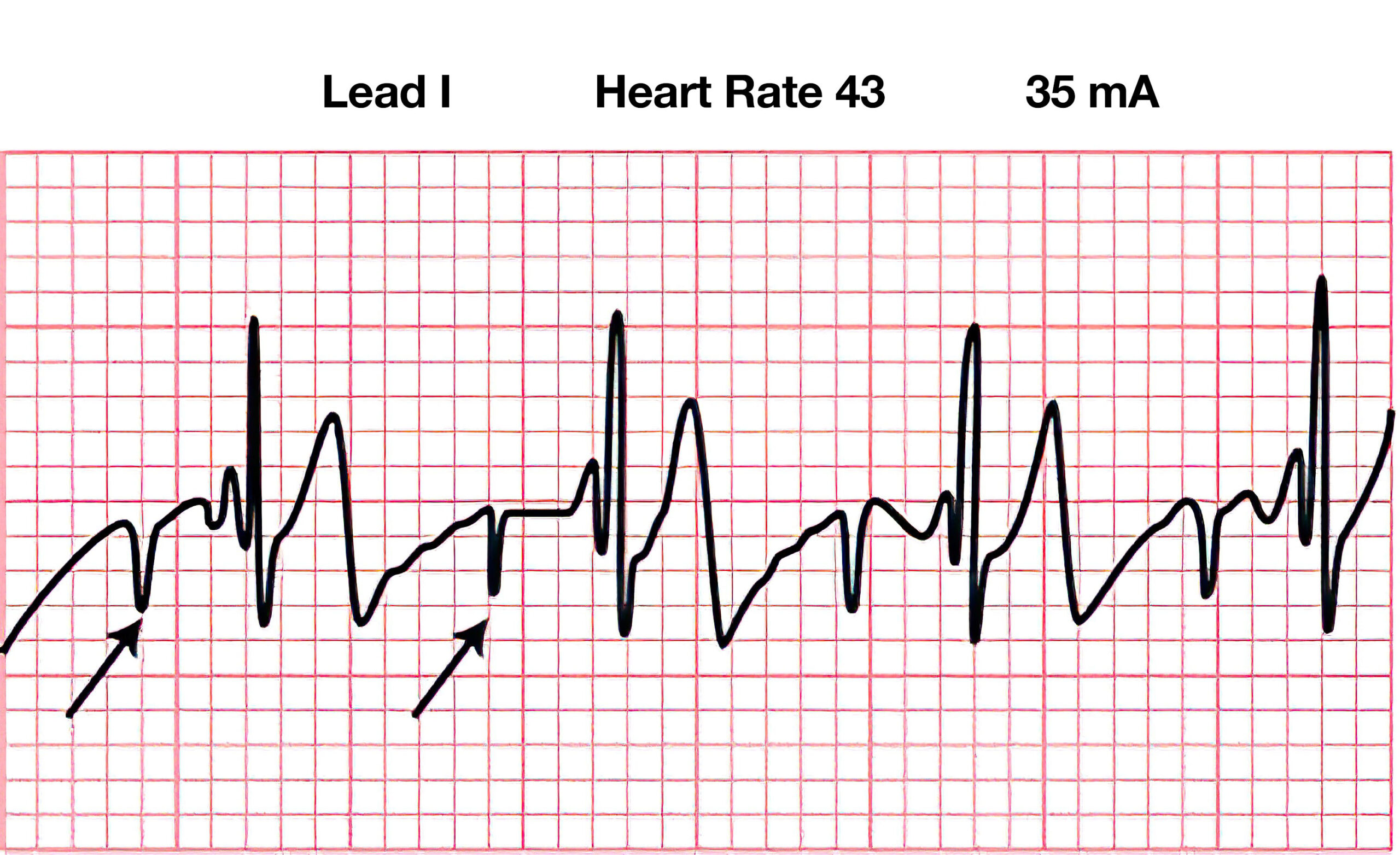
TCP Attempted at Too Low a Threshold
Complications of TCP
There can be complications associated with TCP:
- Unnoticed underlying shockable VF: patients managed with TCP may have VF or pVT. A large electrical artifact from the pacer may obscure this critical finding. This is more likely to happen if monitor blanking is not effective or if the patient is using a transport monitor for pacing in which monitor blanking is not available.
- To manage: responders implement TCP using a device equipped with monitor blanking so that the underlying rhythm is visible. The femoral pulse should be monitored as this can help determine adequate ventricular contractions. If a pulse cannot be found, this could mean an underlying pulseless rhythm (VF or pVT) or a lack of pacer capture.
- Inability to capture: this can be secondary to low output or improper electrode placement. While capture is not related to patient weight, conditions increasing intrathoracic air (significant emphysema or pneumothorax) may limit the ability to capture. Likewise, a fluid collection around the heart, such as pericardial or pleural effusion, may also limit the ability to capture. Additionally, some metabolic derangements, such as severe hyperkalemia, are incompatible with capture.
- To manage: First, the output is increased. If this is not successful, the pacer electrodes should be moved. Anterior-posterior electrode placement is more effective and prevents placement over bones such as the spine or scapula. Multiple trials of pad placement may be required to gain capture. If this is still unsuccessful, adrenergic medications are recommended as the next step.
- Not recognizing inability to capture: this is often due to the large artifact from the pacing impulse and lack of monitor blanking. Additionally, the contraction of skeletal muscle may also make this more difficult to discern.
- To manage: responders should always ensure a post-QRS T wave on ECG. The palpated pulse should be equivalent to the pacer-generated rate. If available, cardiac ultrasound can help to evaluate wall motion to determine effective TCP.
- Not recognizing electrical capture without mechanical capture: the goal of TCP is mechanical capture or effective ventricular contraction leading to a palpated pulse, cardiac output, and hemodynamic stability. If electrical capture occurs without an effective mechanical response, TCP is unsuccessful, and electrical-mechanical disassociation has occurred. In this case, chest compressions are required, and the patient is considered to be in asystole or PEA and should be managed with the algorithm for cardiac arrest due to asystole/PEA.
- To manage: CPR should begin immediately with chest compressions. In such cases, when using CPR and TCP in conjunction, electrical capture can become re-associated with mechanical capture. The amount of current used in TCP is unlikely to cause damage to responders, but using gloves helps to diminish the risk of a noticeable current.
- Pacer-associated arrhythmia and VF: TCP is rarely associated with arrhythmias, as the current used for TCP is usually lower than that needed to instigate fibrillation. However, even a low level of current given at the incorrect timing of the cardiac cycle may instigate VF or VT.
- To Manage: Rhythm and pulse should always be monitored when using TCP.
- Pain: Awake patients generally have discomfort from TCP due to the associated skeletal muscle contractions. Some studies suggest that 1/3 of patients will have significant pain with TCP.
- To Manage: Adequate analgesia or sedation must be ensured. Providers generally use IV benzodiazepines for anxiety and muscle relaxation and IV narcotics for pain control. If significant sedation is needed, the patient may require an advanced airway for ventilatory support.
Electrical-Mechanical Association
Electrical activity (myocyte depolarization) must be coupled with mechanical activity (myocyte contraction) to be effective. This requires complex interactions of the myocytes, extracellular space, electrolyte gradient as well as effective actin and myosin interactions. As noted above, electrical-mechanical disassociation can occur in which the cell depolarizes with no adequate muscular contraction. This is a failure of electrical-mechanical association.
With pacing, each pacing spike has a subsequent myocyte depolarization. In temporary transvenous pacemakers, the pacer electrode is most often in the right ventricle. However, in permanent or implanted pacemakers, it may be placed in the atrium, the ventricle, or both. The placement of a permanent pacer leads to a difference in the observed ECG strip. As with temporary pacers, the associated QRS indicates electrical capture only and must be combined with an evaluation of the patient’s hemodynamic state to ensure good electrical-mechanical association.
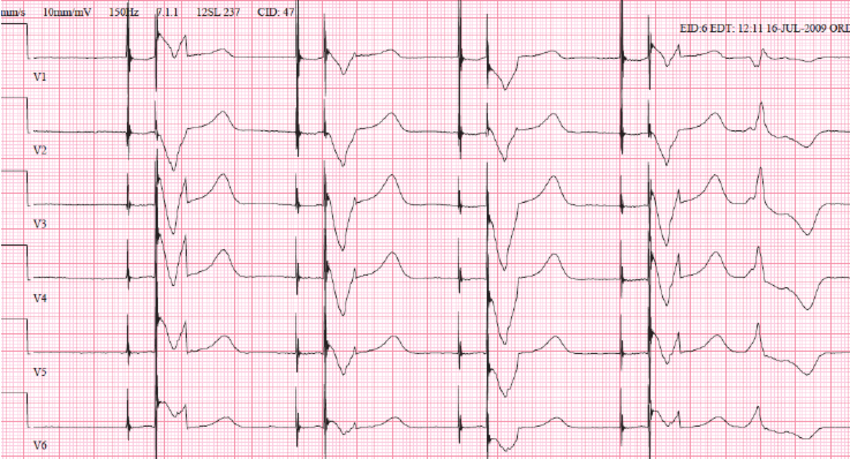
Dual-Chamber Pacemaker ECG