STEMI
STEMI is the ECG reflection of the acute death of myocardial cells, usually caused by an acute MI. The ST elevation is an early finding that allows time for rapid diagnosis and treatment with reperfusion.
Responders should be aware that troponin elevation may be delayed up to 4–6 hours after ECG findings and may not be confirmatory early in the disease process. Typically, if myocardial cell death continues, ECG findings will progress to Q waves, indicating scarring (and irreversible death) of the cells. At this point, an elevation in troponins can help differentiate angina from and MI. However, since Q waves are a later ECG finding, they are not useful for the acute management of patients.
Measuring ST-segments
Changes (elevation and depression) of the ST-segment must be accurately measured. To measure:
- The base of the ST should be at the level of the TP segments (the terminal part of the T wave to the initial part of the P wave). Conventionally, the PR segment is used, but the TP is actually more accurate. It is also useful when the ST segment is curved or when the T waves are hyperacute.
- The J point is the angle between the QRS and ST segments.
- The ST segment is measured from the TP segment to 1 mm (or 0.04 seconds) from the J point.
ST Change Measurement
Related Video: ST Segment Elevation Explained
Alternate causes of ST elevation
There are many non-ACS causes for chest pain, both emergent and nonemergent. A rapid evaluation should be done to rule out life-threatening causes as well as the likelihood that a patient would have one of these conditions.
Healthcare responders must integrate clinical information and ECG findings. The acuity of the situation will determine the benefit of obtaining other laboratory studies and imaging, such as an an echocardiogram or CT scan.
Importantly, other conditions may cause ST elevation:
- Left ventricular hypertrophy (LVH)
- Left ventricular aneurysm
- Neurologic events
- Prior left bundle branch block (LBBB)
- Early repolarization events
From Wang et al. Copyright 2003 Massachusetts Medical Society. With permission from the Massachusetts Medical Society.
NSTEMI
In patients who have decreased but not absent blood flow, the ECG may show normal or depressed ST changes. Elevation in troponin levels indicates the NSTE variant of ACS.
Natural history of 12-lead ECG changes in ACS
The ECG is not stable but changes with cardiac pathology. Initially, there will be signs of loss of blood supply to the area, followed by myocyte injury, and finally myocyte death. While the progression and findings are not uniform in all patients, there will be a progression of changes.
Early in the course of STEMI, the ECG will show peaked T waves, which are considered hyperacute changes. Towards the end of the course, Q waves typically will appear, and they indicate myocyte death. However, this is not guaranteed as sometimes Q waves will appear early and resolve over time.
STEMI ST Change Progression
Sudden Cardiac Deaths
ACS may lead to a catastrophic event, including cardiogenic shock or life-threatening arrhythmia. When this occurs, the patient may go into cardiac arrest. This is a major underlying cause of out-of-hospital cardiac arrest.
In the setting of an arrhythmia co-occurring with ACS, ventricular fibrillation is most likely. Patients should be managed with CPR and early defibrillation. However, outcomes tend to be worse in patients with underlying ACS.
Mechanism of Action of ACS
As mentioned above, the underlying etiology of ACS is atherosclerosis of the coronary arteries. This is a gradual process that, over time, leads to plaques that block the lumen of the arteries. Most of the plaque is subluminal or within the arterial wall. Importantly, a significant amount of plaque is required for ACS. The majority of symptomatic patients have at least a 70% blockage of the arteries (based on angiography studies).
Consequently, many plaques do not occlude the arteries and are asymptomatic. When the plaque ruptures, it causes hemodynamic changes that lead to symptoms. It also can be difficult to predict which plaque will cause problems based on angiography or stress tests. However, evaluation of the plaque based on the amount of lipid present, the covering separating it from the lumen, and the extent of associated inflammation can be useful for determining its stability and subsequent risk for rupture.
- Stable plaque: these plaques have lower lipid levels with a thick, stable cap separating it from the lumen. Consequently, they are less likely to rupture but instead progressively encroach on the lumen, leading to decreased blood flow, which may manifest as exertional chest pain.
- Vulnerable plaque: these plaques are rich in lipid and have a high level of acute inflammation. As a result, they are at high risk of rupture. They are less likely to infringe on the lumen or cause a reduction in blood flow, so they usually will not lead to exertional angina or a positive stress test. Research is still needed to better identify and diagnose these plaques on imaging studies such as cardiac MRI and CT.
Inflammation is common in plaques, especially at the junction with high arterial blood flow. High levels of inflammation lead to unstable plaques that are at high risk of rupture.
Stable Versus Vulnerable Plaque
There are several goals for managing STEMI:
- minimize the size of infarction
- treat or prevent cardiac arrhythmias
- treat or prevent heart failure
- treat serious complications, including rupture of the myocardium and valvular dysfunction
Patients with complete blockage of the arteries overlying the heart surface (epicardial coronaries) will have ST elevation and progressive cell death from the subendocardium to the epicardium. While in a few patients, the obstruction might resolve spontaneously, the majority of patients will need fibrinolytics or other reperfusion therapies to reverse or at least limit the damage.
Success is dependent on the time between the occurrence of the obstruction and the intervention that restores blood flow, and thus the timing is critical. Most myocytes will die within the first few hours after loss of blood flow, and reperfusion will be needed within this time frame to improve survival as well as preserve cardiac function. Typically, by 2 hours following obstruction, 50% of the myocardium will have infarcted, with 90% or more by 6 hours. Of course, this will depend on which coronary artery has obstructed, the degree of obstruction, and any collateral blood supply to the area.
Initial Treatment of STEMI
Outside of the hospital
About 50% of patients who have acute MI outside of the hospital expire before admission. These deaths are likely attributable to life-threatening arrhythmias, such as VF or pulseless VT, as well as sudden deaths due to catastrophic events.
In order to improve these outcomes, there must be community programs that help bystanders to identify and manage ACS within the community setting, including the performance of prompt, high-quality CPR and defibrillation.
Factors that must be addressed to ensure rapid and efficient care in the community include:
- delay in patient recognition of symptoms
- delay in rapid defibrillation
- lack of access to AED or 12-lead ECG
- delay in EMS communication with receiving hospital
- poor triage of the appropriate receiving hospital
Negative outcomes of delay
Delays in the diagnosis and treatment of patients with STEMI lead to worse outcomes. Fibrinolytics and mechanical reperfusion must be administered expeditiously to be effective. Everyone, from patients to caregivers and EMS and healthcare responders must be aware that time is of the essence.
There are three major areas that can lead to delays in the delivery of care for patients with STEMI in the community:
- Delay in patient recognition of symptoms is a critical reason for delaying patient care and likely accounts for up to 70% of delay in care. Patients with known heart disease should take nitroglycerin with chest pain and activate EMS if their symptoms are not better within 5 minutes.
- Transport of the patient via EMS causes fewer delays. Additionally, EMS can speed up their services by communicating early with the receiving hospital. Most patients will present to the ED using a private automobile, which adds to the time delay.
- Once at the ED, the time to beginning treatment makes up about 1/4 to 1/3 of the delay in care.
Efforts to educate the public, integrate care, and allow the administration of fibrinolytics outside of the hospital have helped to decrease delays in care. Additionally, quick triage of patients with direct delivery to the cath laboratory has also been a way to save precious moments and ensure better outcomes.

Nitroglycerin treats chest pain.
Improving patient recognition
Although chest pain is a common finding in patients with ACS, many patients will delay the activation of EMS due to denial or minimizing symptoms. Women, older individuals, and patients with diabetes and hypertension are more likely to have atypical presentations, which may cause further delays. For these patients and other resource-limited populations such as patients on Medicaid or without insurance, racial minorities, and those with disabilities, the average delay in care can be 2 hours or more.
Research shows that the use of ambulance services can reduce delays in care. Additionally, the time, location, and availability of caregivers or family members can also affect time delays.
Ways to minimize delays
Educating patients with known heart disease or those at risk for coronary artery disease is a key step in helping to minimize delays in care. Additionally, health providers should enlist the aid of caregivers or family members to encourage them to access care quickly if they identify suggestive symptoms. On the other hand, education aimed at the general public does not consistently lead to a reduction in care delays.
Recognizing ischemic chest pain
Chest pain from ischemic cardiac lesions is often under the sternum and described as pressure, crushing, and restrictive. Other symptoms concerning for ACS chest pain include:
- pressure, pain, or tightness at the center of the chest lasing several minutes
- radiation to the neck, shoulder, arm, jaw, or back
- associated dizziness, diaphoresis, nausea, or emesis
- sudden dyspnea (may not have associated chest pain)
Research indicates that up to 54% of individuals with typical ACS chest pain had ACS. Of course, a significant number of patients had GERD (43%). Of note, in patients with no heart disease history, complaints of chest pain that is stabbing, pleuritic, worse with palpation, or positional is almost certainly not ACS.

Chest pain is a symptom of ACS but may be confused with GERD symptoms.
Preliminary EMS Management of STEMI
Emergency medical services (EMS) should be familiar with the presentation and management of ACS. These responders will need to perform preliminary management, diagnose, and transport patients to the most appropriate healthcare facility.
Their management includes:
- Determining which patients likely have ACS
- Assessing and managing the ABCs
- assessing vital signs and heart rhythm
- providing CPR and early defibrillation if needed
- Promptly performing a 12-lead ECG and communicating findings with the receiving facility
- Evaluating for any abnormal rhythms, especially VF or VT that requires defibrillation
- Obtaining patient history, keeping the fibrinolytic checklist in mind to determine acceptable candidates for therapy
- Obtaining vascular access and measuring oxygen saturation
- Being prepared to provide transcutaneous pacing if needed for associated ACS bradyarrhythmia
- Providing primary ACS care, including the administration of:
- oxygen for O2 saturations under 90% or those in cardiac arrest
- aspirin (if no allergy/contraindication)
- nitroglycerin (sublingual or spray) at 3- to 5-minute intervals (if no contraindications)
- morphine as needed for chest pain refractory to nitroglycerin (morphine may increase mortality in patients with NSTE-ACS)
Key Takeaway
Morphine may increase mortality in patients with NSTE-ACS.
Related Video: Morphine – ACLS Drugs
Morphine
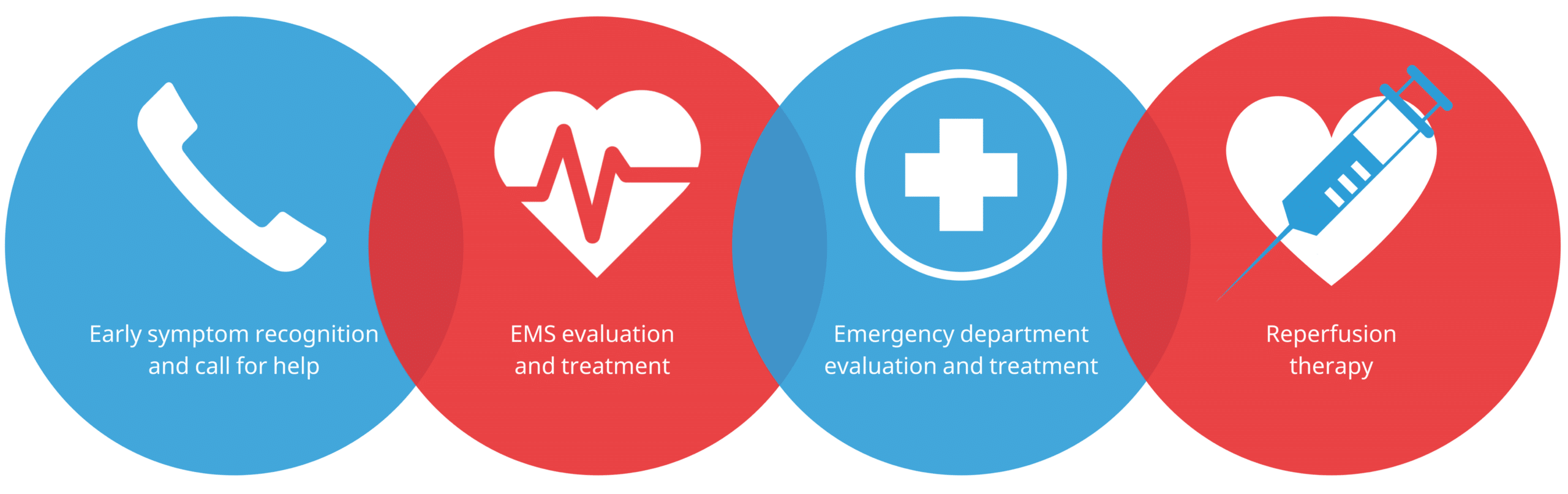
Survival Chain in ACS
ECG outside of the hospital
Obtaining an ECG and communicating the results with the receiving hospital is key to minimizing delays in care. Studies indicate that this can decrease delays by 10–60 minutes and is associated with improved survival. Thus, it is recommended that EMS providers obtain an ECG on the field.
It is also important that EMS staff are trained in interpreting the ECG findings of ACS. Even if EMS is unable to interpret the ECG, they can transmit the findings electronically to minimize delays. This allows the receiving hospital to prepare for fibrinolytics or the cath laboratory to prepare for intervention before the arrival of patients with STEMI.
It is likely beneficial for EMS staff who can interpret ECGs to activate these services, even if a physician is unable to confirm the findings. Additionally, when STEMI is identified, EMS staff should evaluate for any major contraindications to reperfusion. The fibrinolytic checklist is helpful in this regard.
