Using the Algorithm for Cardiac Arrest for Shockable Rhythms (VF and pVT)
ACLS is based on high-quality CPR, beginning with chest compressions and early defibrillation. When a cardiac arrest is witnessed, bystanders should begin CPR immediately and defibrillate as soon as possible to increase survival. On the other hand, ACLS therapies such as intubation or IV medications have not been shown to increase survival. Here, we will discuss the algorithm for managing cardiac arrest for shockable rhythms.
Following assessment and intervention using BLS (activation of EMS, high-quality CPR, manual defibrillation, and shock delivery), the ACLS provider can begin using the initial and secondary evaluations.
Responders continue high-quality chest compressions while evaluating to determine the underlying cause of arrest and response to treatments are simultaneously undertaken. An appointed team leader will coordinate assessment and evaluation using the algorithm for cardiac arrest for shockable rhythms. The team leader should also assign roles according to responders’ skillsets and experience.
Key Takeaway
- Immediately following defibrillation, restart chest compressions.
- Complete 2 minutes of 5 cycles of CPR before evaluating the pulse or rhythm.
- Assess the patient.
- ROSC can be signaled by a sudden increased ETCO2 level > 40 mm Hg.
- Do not interrupt chest compressions for > 10 seconds.
During the first few minutes of CPR, all interventions are organized to keep interruptions to chest compressions to a minimum. The perfusion pressure of the coronary arteries (CPP) is calculated by subtracting the diastolic pressure during right atrial relaxation from the diastolic pressure of aortic relaxation. CPP is associated with blood flow to the cardiac muscle and the return of spontaneous circulation (ROSC). Studies have shown that CPP should be at least 15 mm Hg to ensure high-quality CPR.
When providing shocks in the algorithm, the dose depends on the defibrillator type. For monophasic defibrillation, 360 J of energy is used for the first and subsequent shocks, if needed. For biphasic defibrillators, the manufacturer’s recommendations should be followed and usually range between 120 J and 200 J. This should be displayed on the device. If it is not, the maximal energy available on the device should be used for all delivered shocks. If the first shock stops the arrhythmia, but it recurs later during CPR, responders should use the same energy for the next shock.
Key Takeaway
Biphasic Defibrillators
Use a dose between 120 J and 200 J (according to manufacturer’s recommendations) to treat VF.
Subsequent shocks should be at the same energy level or at increasing energy levels.
Monophasic Defibrillators
Use a dose of 360 J for the first and any subsequent shocks.
If VF is recurrent, use the same energy level as used prior for subsequent shocks.
Chest compressions should be restarted immediately following delivery of the shock.
Responders:
- Never delay compressions at this time to check for a pulse or cardiac rhythm
- Obtain IV or IO access simultaneously while another team member provides compressions.
The responder providing shocks should always clear the patient and ensure that no one is touching the patient. This notification should be given in a loud and authoritative voice before shock delivery. Rhythm checks can then be done after 2 minutes or 5 cycles of CPR.
If the new rhythm is not shockable and appears organized (i.e., with narrow and regular QRS complexes), responders try to palpate the pulse.
- If there is an organized rhythm and a palpated pulse, they proceed to post-arrest care.
- If there is a nonshockable rhythm and no pulse, they move to the asystole and PEA arm of the algorithm (boxes 9–11).
- If there is a shockable rhythm, the team delivers another shock and again immediately restarts CPR, beginning with chest compressions right after shock delivery.
When there is a persistent shockable rhythm (VF or pVT), shock delivery is followed by 2 minutes or 5 cycles of CPR. If the patient has IV or IO access, vasopressor medications should be delivered.
Epinephrine Injection
Epinephrine: 1 mg IV or IO is given after the second shock and repeated every 3–5 minutes.
Additional team members need to prepare these medications in advance to minimize delays in care.
The benefit of epinephrine during CPR is that it is an alpha-adrenergic agonist that causes vasoconstriction. This effect improves blood flow to the heart and brain, which leads to an increase in both the mean arterial and aortic diastolic pressures.
However, research has not shown that epinephrine improves survival or long-term neurologic function. Therefore, giving high doses or increasing doses of epinephrine above 1 mg is not recommended.
Related Video: Epinephrine – Cardiac Arrest
Medication delivery should flow with CPR and should not delay chest compressions.
The team can give anti-arrhythmic medications before or following shock delivery. When shockable rhythms are unresponsive to defibrillation and vasopressors, the responder should consider giving amiodarone or lidocaine. However, there is no conclusive evidence that anti-arrhythmic medications increase survival to discharge from the hospital.
Responders must always check for the underlying and treatable cause of cardiac arrest.
Return of Spontaneous Circulation
Once achieving ROSC, patients should be managed with appropriate post-arrest care. During this phase, patients must be evaluated and treated for hypoxemia, hypotension, and acute cardiac syndrome. This is also the time to initiate medical hypothermia in patients who remain comatose.
Related Video: ROSC Achieved – Now What?
Managing VF
Health care responders must recognize VF quickly. In this disorganized rhythm, the ventricle has a wide variation in the polarity at different locations. Consequently, there is no unified depolarization of the ventricle, no effective contraction of the ventricle, and no useful cardiac output. Treatment begins with CPR followed by quick defibrillation.
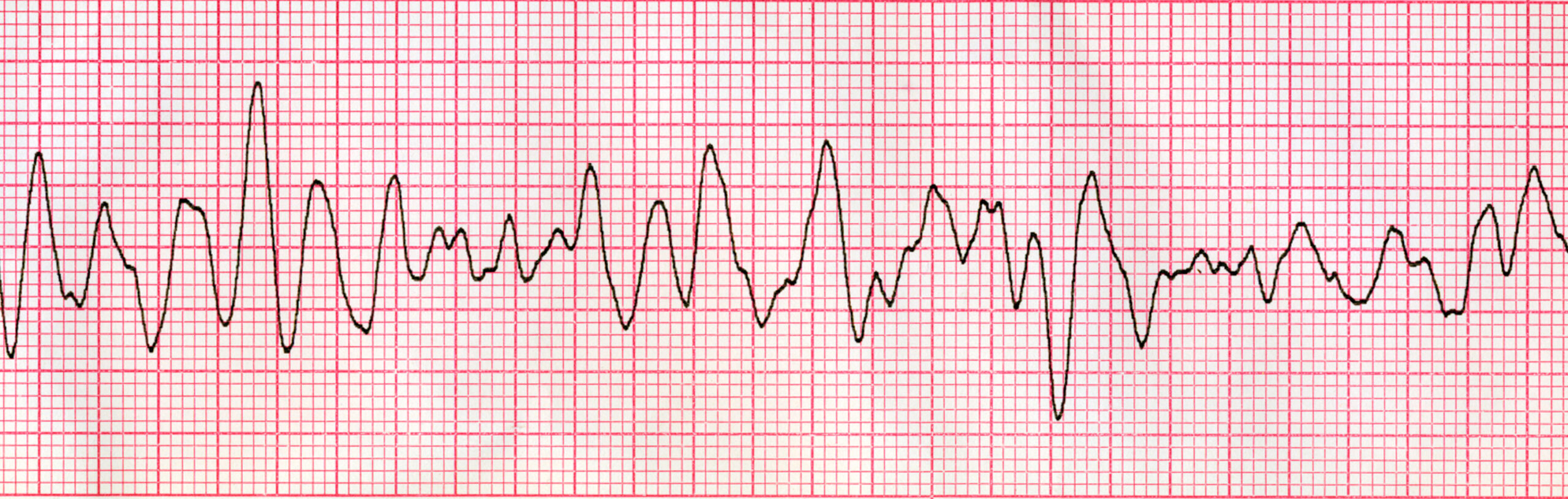
Ventricular Fibrillation
Variations in VF
Loss of blood flow to the cardiac muscle as an underlying cause of cardiac arrest often manifests as VF. There are two main types of VF in this situation: coarse VF and fine VF.
Coarse VF is the initial presentation of VF and generally lasts for about 3–5 minutes. This type of VF displays a high amplitude and utilizes a significant amount of ATP. These findings indicate there are still energy reserves in the heart, and coarse VF is more likely to have successful defibrillation leading to an organized perfusing rhythm.
On the other hand, fine VF usually occurs later and indicates that energy resources are nearly exhausted. This fine variation may resemble asystole and frequently occurs following a significant delay in CPR. Such patients have a decreased chance of achieving ROSC.
At this time, it is not known if the VF quality can guide treatment. There may be some benefits in guiding responders to provide prolonged CPR or administer other therapies before defibrillation if the defibrillator recognizes an increased risk of post defibrillation asystole.
Refractory VF
The first shock may not treat VF and provide a perfusing cardiac rhythm. In this case, VF can persist, recur, or be refractory to shocks.
- Persistent VF: VF continues after defibrillation.
- Recurrent VF: VF is abolished but then recurs more than 5 seconds later.
- Refractory VF: VF continues after defibrillation, medications, and airway management.
These different responses may help categorize finding the underlying cause of the cardiac arrest and guide treatments.
Underlying Causes of Cardiac Arrest
There is a range of causes for cardiac arrest. Responders should be aware of the Hs and the Ts, which provide a good framework for evaluating the cause of arrest. This list is more commonly a cause for arrest due to asystole or PEA.
Related Video: One Quick Question: What are Hs and Ts?
Managing Medications and Airway
The primary goal of resuscitation are high-quality CPR and quick defibrillation. Drug delivery is a secondary goal. Consequently, obtaining intravenous or intraosseous access to provide medications should be emphasized only after the primary goals of CPR and defibrillation have been achieved and are ongoing. Unlike CPR and defibrillation, there are no guidelines for time to IV or IO access during resuscitation. However, there is evidence of a benefit to obtaining access expeditiously.
Responders must be aware that advanced airways come with risks as well as benefits. Placement of an advanced airway can lead to a delay of chest compressions, and consequently, the team leader must make the best decision possible as to the need for an advanced airway. If basic airways such as bag-masks provide adequate ventilation, it may be beneficial to delay the placement of an advanced airway until the team stabilizes the patient. Additionally, the responder placing the advanced airway must be skilled in this task as there are certain adverse events associated with their placement.