Chest Pain in Toxin Exposure
Patient abusing cocaine may complain of chest pain. While the pain is usually self-limiting without evidence of ischemic changes on EKG, some patients may experience ischemia due to adrenergic associated spasms of the coronary artery. Even more rarely, cocaine users may experience acute MI. The etiology is due to the increased beta-adrenergic associated increase in cardiac oxygen demand and alpha-adrenergic associated vasoconstriction of coronary vessels. The treatment will be directed at patient symptoms as well as drug-associated toxicities, including vasoconstriction, ischemia, and arrhythmias.
Nitroglycerin and benzodiazepines
These medications are used for toxin associated ACS. Research indicates that nitroglycerin can reverse the vasoconstriction associated with cocaine use.
Phentolamine
This alpha-blocking medication is a potent vasodilator and can reverse the vasoconstriction associated with cocaine use. It is considered second-line treatment.
Caution
Be aware that beta-blockade can further cause deterioration in coronary blood flow or can cause hypertension in cocaine users. Consequently, pure Beta-blockers are not recommended for use in cocaine overdose.
Fibrinolytic therapy
ST elevation MI (STEMI) can occur with cocaine overdose. While the coronary artery spasm may be the inciting cause, thrombus can develop, similar to other cases of STEMI. Fibrinolytics may be a useful therapy if there is no associated uncontrolled hypertension. There is reported aortic dissection associated with cocaine abuse. In these cases, fibrinolytics would be contraindicated. In these patients, a detailed physical examination, history, and imaging with a chest x-ray (and if possible echocardiogram) are completed if there is a concern for aortic dissection. Neurologic deficits should prompt evaluation for bleeding within the brain or carotid artery dissections.
PCI is usually preferred to manage toxin associated ACS, especially in the case of comorbid atherosclerosis. Cardiac catheterization will direct treatment with PCI, or if indicated, antiplatelet therapy such as abciximab if there is a significant clot burden.
Toxin associated Tachycardia
Tachycardia commonly occurs with toxin ingestion. When these are asymptomatic, no treatment is needed. Occasionally, however, tachycardia may be severe enough to cause hemodynamic changes or even acute MI or arrhythmias that cause cardiac failure. Typically, adenosine or synchronize cardioversion will not be effective in these scenarios. Do not use verapamil or diltiazem when there is associated hypotension as they will worsen blood pressure.
Benzodiazepines
These medications are useful in treating toxin associated tachycardia as they opposed the excess adrenergic state associated with tachycardia. Additionally, benzodiazepines are effective at opposing cocaine’s effects on the brain and heart. It is important to monitor the consciousness level and ventilatory effects as these are affected by this class of medications.
Physostigmine
This is an antidote to anticholinergics, and it opposes toxin associated tachycardia with hemodynamic effects and the associated anticholinergic effect. Of course, excess doses may work too well, causing the opposite effect with cholinergic excess and associated seizure, bradycardia, or asystole. It should not be used when anticholinergic excess is due to tricyclic antidepressants. It is good sense to consult with a toxicologist as needed.
Propranolol
Beta-blockade with propranolol and other nonselective Beta-blockers can help manage toxin associated tachycardia. However, do not use this for cocaine, ephedrine, or amphetamine overdose as they can worsen coronary blood flow or cause hypertension in cocaine users.
Toxin associated Hypertension
Typically, hypertension associated with toxins is short-lasting. The typical treatment is benzodiazepines, which opposes catecholamine excess. A significant hypertensive crisis can occur with cocaine use.
Benzodiazepines
These are the first medications used to manage a hypertensive crisis in sympathomimetic toxin overdose, including cocaine and amphetamine abuse.
Nitroprusside
If benzodiazepines are ineffective, nitroprusside, a quick-acting anti-hypertensive, can be used.
Alpha and Beta-blockade
Combining alpha and beta-blockade can help in these situations. Combinations include phentolamine and labetalol. However, there is new research suggesting that beta-blockade should not be used in cocaine-associated hypertensive crises.
Cocaine
Cocaine can cause significant consequences when abused. Cocaine works by increasing epinephrine, norepinephrine, dopamine, and serotonin release and decreased their reuptake. This leads to sympathomimetic syndrome with hypertension, tachycardia, and excess energy. Associated consequences include seizure, acute MI, and death.
The majority of the ill effects are cardiac-related. Beta adrenergic stimulation increases heart rate and contractility, and alpha-adrenergic stimulation decreases blood flow to the coronary arteries, and occasionally spasm of the same arteries. There is also associated platelet adhesion increasing the risk of thrombus. Cocaine also can cause fevers and seizures, which further worsen the effect on the heart. Additionally, cocaine is associated with accelerated atherosclerosis and hypertrophy of the left ventricle. Any patient using cocaine with cardiac or neurologic signs of toxicity must be closely monitored with a low threshold for continuous cardiac monitoring if there are signs of arrhythmia.

Cocaine has deleterious effects on the cardiovascular system.
Supraventricular Tachycardia (SVT)
Cocaine can cause paroxysmal SVT, atrial flutter, and fibrillation. These usually resolve rapidly and do not require treatment unless there is hemodynamic instability. If SVTs persist, treat with benzodiazepines.
Ventricular Tachycardia.
Cocaine-associated stable V-Tach (with pulses) includes ectopy, unsustained V-Tach, and stable monomorphic or polymorphic V-Tach.
Benzodiazepines
These are usually short-lasting and may resolve with observation. If this does not occur, the arrhythmias can be managed with benzodiazepines.
Antiarrhythmics
With overdose, cocaine act similarly to a class Ic antiarrhythmic medication and causes wide QRS tachycardias by blocking sodium channels. It is reasonable to treat patients with hypertonic sodium bicarbonate as research suggests this is beneficial in the class Ic antiarrhythmics such as tricyclic antidepressants and flecainide. Typical management is sodium bicarbonate 1-2 mEq/kg bloused and repeated until resolution of wide QRS.
1-1.5 mg/kg of lidocaine may also be used in patients with ventricular arrhythmias failing benzodiazepine management. Since both cocaine and lidocaine block the sodium channel, lidocaine can competitively inhibit cocaine effects. There is no good evidence indicating a benefit or detriment to lidocaine use.
Defibrillation
Defibrillation should be made available in case the V-Tach becomes unstable or pulseless.

Hospital Defibrillator
Ventricular Fibrillation
Cocaine-associated cardiac arrest should follow the same treatment algorithms as cardiac arrest from other etiologies. Antidotes specific to the toxicities can be given if the patient achieves ROSC.
Cocaine-associated Pulmonary Edema and Hypertension
Pulmonary Edema
Cocaine affects pulmonary function, cardiac ischemia, and subarachnoid hemorrhage, which can all contribute to pulmonary edema. The management is with positive pressure ventilations and continuous positive end-expiratory pressures via a mask or advanced airway.
Hypertension
Cocaine overdose can cause hypertensive emergencies via the alpha-adrenergic vasoconstriction. Standard treatment is with benzodiazepines. If needed, nitroprusside or nitroglycerin can be used. Nitroglycerine is more beneficial if there is associated chest pain. Do not give selective beta-blockade in this setting. (Class Iib, Evidence level C). Even medications with combined alpha and beta-blockade (i.e., labetalol) are not as effective as nitroglycerin. However, selective alpha-blockers such as phentolamine can be given.
Key Takeaway
Propranolol and other non-selective Beta-blockers should not be used in toxin associated hypertension as this leaves unopposed alpha-adrenergic stimulation to worsen coronary perfusion and cardiac output.
Chest Pain in Cocaine
Rarely, a cocaine user may experience acute MI. Typically, these patients will have underlying risks for ACS. Cocaine increases acute MI risk by 24 in the 60 minutes following use, although risk persists longer than this. Patients should be treated using oxygen, nitrates, aspirin, and benzodiazepines. Do not give Beta-blockers as this will lead to unopposed alpha-adrenergic stimulation and the risk of associated coronary artery spasm. Magnesium can be helpful to minimize coronary artery spasm and associated ischemia in patients. Morphine can be used to manage chest pain.
Managing STEMI associated with Cocaine
About ½ of acute MI associated with cocaine overdose is due to coronary spasms. Unfortunately, the difference between coronary spams and thrombus is not easily identified used ST changes on EKG. Consequently, some providers may further evaluate with an echocardiogram or quick assay of cardiac biomarkers. Also, cardiac catheterization can be diagnostic in this situation.
Cocaine-associated ACS versus other etiologies
More contemporary high-quality and multicenter research regarding cocaine-induced ACS exists; however, much of the guidelines and consensus is based on smaller studies, related research using non-cocaine-induced ACS and expert opinion. There are certain differences between cocaine-associated ACS and other etiologies of ACS
- Benzodiazepines are first-line treatment for cocaine-associated ACS (but not for other etiologies of ACS).
- Beta-blockers are contraindicated in cocaine-associated ACS (but not for other etiologies of ACS). Research indicates that Beta-blockers can worsen neurologic toxicity as well as vasospasm of the coronary arteries. Additionally, it does not reverse hypertension or tachycardia. Additionally, mixed alpha and Beta-blockers do not show significant benefit and are not recommended either.
- Percutaneous coronary interventions may be preferred for cocaine-associated ACS to distinguish coronary spasm from a thrombus (but not for other etiologies of ACS).
The goals for cocaine-associated ACS are similar to other etiologies to maximize cardiac recovery by improving perfusion and delivery of oxygen. Benzodiazepines achieve this goal in many cocaine-associated ACS cases and also protect the brain and calm the patient. Nitroglycerine is used to minimize vasoconstriction and improve chest pain. Antithrombotic and antiplatelet medications can help decrease coagulopathy in cocaine overdose.
Refractory Cocaine-associated ACS
Other therapies for these patients include phentolamine, calcium channel blockers, and reperfusion strategies when symptoms are refractory.
Phentolamine is an alpha-adrenergic antagonist that blocks cocaine effects and reduces coronary vasoconstriction. A side effect is hypotension.
Calcium channel blockers are controversial in managing cocaine abuse. Some studies have shown benefit with verapamil use at improving vasoconstriction and survival and reducing seizures and arrhythmias. Other studies have shown no benefit in survival and even adverse events.
Toxin Associated Bradycardia
When bradycardia occurs with toxin ingestion, it can become refractory to standard treatment options. Toxins can cause cellular toxicity, which requires specific antidote treatment. An example is bradycardia associated beta-blocker toxicity that is managed with supratherapeutic insulin, IV calcium, or glucagon. Additionally, in association with digoxin overdose, digoxin specific antibodies (FaB) are instrumental in stopping the toxic effects.
Atropine
Atropine is useful in the case of cholinesterase inhibitor toxicity. Such toxic medications in this class include carbamate, organophosphates, and nerve agents. Treat the adult patient with a 2 to 4 mg dose. The dose may need to be increased further for successful treatment.
Pacing
In mild or moderate toxin associated bradycardia, transcutaneous pacing can be therapeutic. However, it is not recommended to use transvenous pacing prophylactically as the catheter tip can elicit ventricular arrhythmias in the irritable cardiac muscles. Transvenous therapy can be used if transcutaneous treatment is not successful.
Beta-agonists
If toxin associated bradycardia is not well managed by atropine or pacing, then beta-agonist therapy can be indicated. Typically, treatment is with dopamine or epinephrine infusion. Also, norepinephrine may be effective. It is not uncommon to use supratherapeutic doses to overcome beta-blockade or calcium channel toxicity.
Do not use isoproterenol as a first-line therapy in toxin associated bradycardia as the associated vasodilation can worsen hypotension and produces ventricular arrhythmia. The medication may be tried at supratherapeutic doses for beta-blocker associated refractory bradycardia.
Digoxin specific antibodies (FaB)
Management of digoxin or cardiac glycoside toxicity is targeted at the significant ventricular arrhythmia as well as atrioventricular (AV) heart block associated with it. Heart block can occur with the use of some herbal medicines, digoxin, and other cardiac glycosides.
Toxicity associated with Beta and Calcium Channel Blockade
Both beta and calcium channel blockade can decrease heart rate (chronotropic) and contractions (inotropic). Additionally, calcium channel blockade may also vary in the amount of vasodilation. Some signs or symptoms of toxicity from these medications include:
- Hypotension
- Negative inotropy
- Decreased consciousness (from lethargy to coma)
- Hypoglycemia/hyperkalemia (Beta-blockers)
- Hyperglycemia (calcium channel blockers)
- Rapid deterioration to shock
- Seizures
- Cardiac arrest secondary to PEA or AV block

One of the signs of toxicity associated with beta and calcium-channel blockade is hypotension.
Additionally, beta-blockade can cause arrhythmias such as VF, AV blockade, torsades de pointes, and asystole.
The negative effects of regular releasing preparations usually occur by 2-4 hours after ingestion. If the patient remains asymptomatic after 4-6 hours, it is unlikely that they will develop significant symptoms. However, if the patient took a long-acting preparation, it may take as long as 18 hours for symptoms to occur.
No good data suggests a specific preferred antidote for these toxic medications. Follow standard management of cardiac arrest if it occurs. Treatment recommendations include:
- Provide oxygen and monitor respirations and airway (especially if diminished consciousness)
- Obtain continuous cardiac monitoring to rule out arrhythmia
- Obtain IV access with two large catheters
- If hypotension occurs, provide 500-1000mL of IV normal saline. Monitor for cardiac dysfunction and pulmonary edema
- Obtain glucose levels
- Consider providing activated charcoal if toxin ingestion was less than one hour ago, and there are mild symptoms only. Consider orogastric lavage instead if the symptoms are significant. Ensure airway protection. If the patient used long-lasting preparations and x-ray shows retained medications (and the patient has bowel activity), consider bowel irrigation.
- Do not use ipecac syrup as its onset is delayed (i.e., it may not work before toxic effects), and it may worsen bradycardia via emesis associated vagal tone.
Managing Calcium Channel Blockade toxicity
Ensure IV access to manage hypotension and cardiac dysfunction
Shock and Hypotension
Start with a 500-1000ml fluid challenge. Ensure no cardiac dysfunction or pulmonary edema. If pt is still symptomatic:
- IV 2 mcg/min infusion of epinephrine (increasing as high as 100mcg/min). Alternative is norepinephrine
- IV 8-16 mg/kg calcium chloride if symptoms persist
- IV 1-3 g calcium with improvement (but not resolution) with calcium chloride
Bradycardia
If bradycardia does not respond to usual treatment, immediately begin transcutaneous pacing (and move to transvenous pacing when available)
Other treatments
If patients’ symptoms still not respond, other treatments include:
- Combined insulin and glucose infusion
- Glucagon: IV 1-5 mg has been shown to manage cardiac toxicity
- Circulatory assist device: i.e., IABP and extracorporeal membrane oxygenation (ECMO) can be used in toxicity refractory to all therapies
- Calcium salts: this can help in severe cases when other therapies are ineffective.
Managing Beta-blockade toxicity
Ensure IV access to manage hypotension and cardiac dysfunction
Shock and Hypotension
Start with a 500-1000ml fluid challenge. Ensure no cardiac dysfunction or pulmonary edema. If the patient is still symptomatic:
- Vasopressors: IV 0.1-0.5mcg/kg/min infusion of epinephrine or another vasopressor that has significant alpha-adrenergic activity.
- Glucagon: IV 1-5 mg if not responding to vasopressors and increase up to 3mg/h. if there is significant cardiac instability, begin with 3-10 mg bolus over 3-5 minutes and then continue the infusion at 3-5 mg/h. (Class Iib, Evidence level C)
- Isoproterenol can be given with other vasopressors, although its additional benefit is not proven. This is a second-line treatment.
- IV 8-16 mg/kg calcium chloride if symptoms persist. Provide this treatment before signs of organ damage.
Bradycardia
If bradycardia does not respond to usual treatment, immediately begin transcutaneous pacing (and move to transvenous pacing when available). Other treatment includes:
- Atropine. It is unlikely to be effective but has no major side effects
- Circulatory assist device: i.e., IABP and extracorporeal membrane oxygenation (ECMO) can be used in toxicity refractory to all therapies. Provide this treatment before signs of organ damage.
- Combined insulin and glucose infusion. Monitor potassium levels as this can cause hypokalemia
Managing Digitalis or Cardiac Glycoside toxicity
Patients may develop symptoms following overdose or after long time use of these medications. Initially, signs of toxicity may be non-specific and include neurologic and gastrointestinal complaints. Some symptoms include weakness, visual changes, weakness, nausea and vomiting, as well as abdominal pain. Patients may also develop arrhythmias, particularly bradycardia (including AV block) and ventricular ectopy. Specific arrhythmias such as atrial tachycardia and high-level AV block, multifocal V-Tach, new-onset ventricular bigeminy, non-paroxysmal accelerating junctional tachycardias as well as regularize atrial fibrillation should raise clinical suspicion for toxic effects.
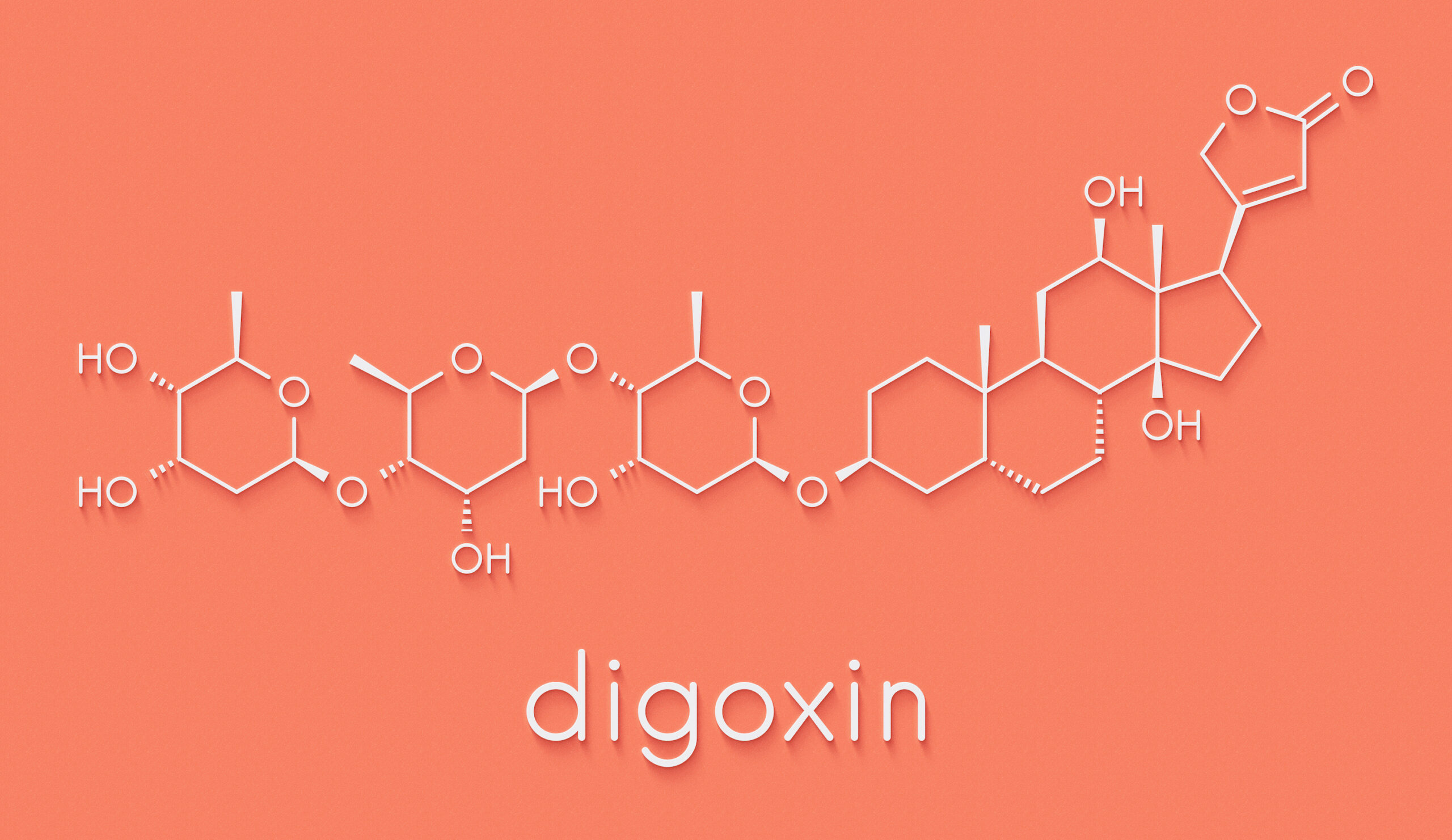
High levels of digoxin may cause heart toxicity.
Cardiac Effects
Digitalis causes inhibition of the cardiac nodes as well as stimulation of fibers of the atrium and ventricle. Significant toxicity can lead to
- Bradycardia and subsequent heart failure
- Ventricular arrhythmia
- Hyperkalemia secondary to digitalis effect on the sodium and potassium specific adenosine triphosphate (ATP) pump.
Managing Digitalis toxicity
Management is based on whether toxicity is acute or long-term.
Long-term toxicity
Most patients with long-term use who develop toxicity will have associated electrolyte abnormalities (hypomagnesemia and hypokalemia), renal dysfunction, dehydration, and decreased muscle mass. Cardiotoxicity can be treated via:
- Replacement of potassium
- Replacement of magnesium
- Replacement of volume
This triad of management will usually treat toxicity associated arrhythmias. If there is refractory toxicity, consider management with digoxin specific antibodies (Fab).
Acute toxicity
In acute settings, the use of activated charcoal if ingestion was under one hour ago is reasonable. Do not use ipecac syrup in hospitalized patients as more reliable therapies are possible.
Use digoxin specific antibodies (Fab) if there is severe and life-threatening digitoxin toxicity. (Class I, Evidence level B). Note that patients are at higher risk for pacemaker associated ventricular arrhythmias, so transvenous pacers may be contraindicated. Consult cardiology as needed. Note as well that digoxin toxicity may be associated with malignant ventricular arrhythmia following defibrillation for cardioversion. Always use the lowest effective cardioversion dose possible. Patients will usually have elevated intracellular calcium and so should not be given calcium salts.
Bradycardia
Atropine
Treat with IV 0.5mg of atropine. Its effects are by blocking the vagal stimulation of digitalis.
Digoxin specific antibodies (Fab)
This treatment is highly effective for severe toxicity from digitalis. The antibodies bind to digoxin, which produces a non-active compound that is excreted by the kidneys. Its effects are within a few minutes, and the full effect is usually in less than 30 minutes. Candidates for this treatment include patients with:
- Cardiac arrest
- Refractory life-threatening arrhythmias
- Significant hyperkalemia (above 5 mEq/L) in acute toxicity
- Digoxin levels over 10 ng/mL following 6 hours from ingestion or digoxin levels over 15 ng/ml in all cases
- Over 10 mg ingestion in adults (0.1 mg/kg or 4 mg in pediatric patients)
- Serum digoxin post-distribution levels over 5 ng/mL
A vial of the digoxin specific antibody is used to treat about 0.5mg of digoxin. To treat appropriately:
- Provide 2 vials for each milligram of digoxin
- If the ingested amount is not known or for cases of chronic use, determine the vial number to give by multiply serum digoxin (ng/mL) by weight (kg) divided by 100.
- If the serum digoxin level is not known and the patient has life-threatening symptoms, give 10-20 vials. If the patient is only symptomatic (not life-threatening), begin with 6 vials.
- Associated hyperkalemia is an ominous finding; administer digoxin specific antibodies if potassium level is over 5 mEq/L in digoxin toxicity.
Key Takeaway
Digitalis associated unstable V-Tach Synchronized cardioversion
10 -20 vials of digoxin specific antibodies
Magnesium sulfate
Lidocaine
Use defibrillation if there is rapid deterioration
If the patient is more stable, use synchronized cardioversion.
Ventricular Arrhythmia
In cases of ventricular ectopy, management with magnesium, potassium, and intravascular fluids is usually sufficient.
Digoxin specific antibodies (Fab)
Use this treatment in combination with anti-arrhythmic when digitalis associated stable V-Tach is present.
Lidocaine
Use this anti-arrhythmic for persistent ventricular arrhythmia (following electrolyte and fluid management). Provide 1-1.5mg/kg, which is rarely associated with toxicity. Continue with 1-4 mg/min infusion until digoxin specific antibodies (Fab) have treated the condition. Monitor for signs of heart or kidney failure that can be associated with toxic effects of lidocaine.
Magnesium
This is a first-line treatment for digitalis associated ventricular arrhythmia. Start with 1-2 g of magnesium sulfate. It can also be used if lidocaine is ineffective. Infuse 1-2g over an hour, followed by 0.5-1 g each hour for persistence. Low magnesium augments digoxin uptake into cardiac cells and decreases the activity of the sodium and potassium ATP pump.
Consequently, hypomagnesemia and hypokalemia can make normal levels of digoxin cardiotoxic. Ensure monitoring of electrolyte levels, blood pressure, cardiac rhythm, respiration, and reflexes. Be aware that magnesium should not be used in patients with AV block or bradycardia and should be cautiously used in those with kidney failure.
Ventricular Fibrillation
No research is available to indicate that specific antidotes should be used for cardiac arrest in digoxin. Follow the typical treatment of cardiac arrest and use antidotes in the post-arrest period if cardiotoxicity remains.
Toxin Associated Conduction Impairment
Sodium channel antagonist medications (i.e., procainamide, flecainide) and tricyclic antidepressants can prolong conduction abnormalities.
Alkalization and Hypertonic Saline.
These therapies help to limit V-Tach due to sodium channel antagonists, tricyclic antidepressants as well as cocaine. The use of hypertonic sodium bicarbonate provides both treatments on one. In cases of calcium channel or beta-blockade associated conduction impairment, treatment with chronotropic treatments including epinephrine, supratherapeutic glucagon, or pacing may be needed.
In patients with toxin associated toxicity, alkalization should aim to achieve a pH between 7.45-7.55.
- Encourage respiratory alkalosis as an initial treatment
- 1-2 mEq/kg bolus of sodium bicarbonate to achieve goal pH
- Infuse alkaline solution using 3 ampules sodium bicarbonate and 30 mEq potassium chloride in D5W
Anesthetic Toxicities
IV administration of anesthetic, including lidocaine, mepivacaine, and bupivacaine, can cause seizures and cardiac arrest. Research suggests that IV rapid lipid infusion can reverse the toxic effect via redistribution of the anesthetic and improving metabolic pathways that neutralize the toxic effect. Consequently, IV lipid emulsions can be administered alongside therapy for cardiac arrest in these patients, especially in patients who have bupivacaine associated cardiac arrest. (Class Iib, Evidence level C-EO). Following ROSC, continued treatment with IV infusion of 0.25ml/kg of lipid emulsion for up to 60 minutes can be helpful. Additional boluses can also be given for refractory symptoms up to 10ml/kg in the first hour of treatment. This treatment may be more successful in this patient population than vasopressors. There is some support for adding lipid emulsions to the protocol for anesthetic-associated cardiac arrest; however, consultation with toxicologists or anesthesiologist is advised.
Tricyclic Antidepressant Toxicity
Tricyclic antidepressant overdose is extremely cardiotoxic and is the major cause of overdose associated death in hospitalized patients. Their toxicity is fourfold:
- Increase catecholamine release while inhibiting reuptake
- Systemic anticholinergic effects
- Inhibit cardiac potassium channels and neurologic and cardiac voltage-dependent (fast) sodium channels.
- Alpha blocking properties

Tricyclic antidepressants carry a risk of overdose.
Signs of toxicity include
- Altered mental status ranging among irritability, delirium, confusion, hallucinations, and seizures
- Sinus tachycardia (with right QRS axis) and wide QRS tachycardias. ECG findings include positive terminal QRS in the lead aVR. Supraventricular tachycardia, hypertension, and prolonged QT interval
- Signs of anticholinergic action: mydriasis, delirium, gastric slowing, urinary retention
Acute changes on EKG, including wide QRS/ventricular arrhythmias, AV block, as well as seizures, coma, acidosis, and hypotension, require urgent management. The most significant toxicities include “3 C’s and 1 A.”
- Convulsions (seizure)
- Cardiac arrhythmias
- Coma
- Acidosis
Managing Tricyclic Antidepressant Toxicity
Typically, symptom onset will be within 2-4 hours following exposure. There can be rapid progression and immediate control of the airway, oxygen delivery, and obtaining IV access are key. Administer activated charcoal if a large dose was taken. Patients should be monitored closely, but do not attempt to elicit vomiting. Use rapid sequenced intubation before orogastric lavage in patients unable to control their airway.
Sodium Bicarbonate
Patients should be treated with sodium bicarbonate to achieve alkalization. Alkalization
decreases the free tricyclic molecules and eliminates the toxic sodium channel blockade of action potential phase 0. Do not give sodium bicarbonate to those with mild tachycardia or stably prolonged QT interval, instead, provide sodium bicarbonate to patients with
- QRS interval over 100ms
- Ventricular arrhythmia
- Hypotensive not responding to fluid challenge
To achieve alkalosis:
- Induced hyperventilation to the goal of 7.50-7.55 in patients with inadequate respiration or seizure.
- 1-2 mEq sodium bicarbonate for 1-2 minutes
- Infuse alkaline solution using 3 ampules sodium bicarbonate and 30 mEq potassium chloride in D5W
- Monitor pH using arterial and venous pH levels.
- Continue sodium bicarbonate infusion as needed until the patient is stable.
Magnesium
Tricyclic antidepressants can cause arrhythmias due to the toxic effect in phase 2 in the action potential. This initially manifests as a long QT then can progress to torsades de pointe. Magnesium can be used to treat this toxicity.
Start with 1-2 g of magnesium sulfate. Provide as a bolus in patients who are unstable and over 1-5 minutes in more stable patients. The maximum dose is 5-10 g.
Cardiac Arrest
Follow the typical treatment of cardiac arrest and use antidotes in the post-arrest period if cardiotoxicity remains. Some research suggests a benefit of sodium bicarbonate with epinephrine, but the study was biased due to associated physostigmine use. Sodium bicarbonate can be considered in tricyclic antidepressant-associated cardiac arrest
Hypotension and Seizure
Seizures worsen hypoxia, electrolyte abnormalities, and acidosis. Most tricyclic antidepressant seizures can be managed with benzodiazepines.
Key Takeaway
Treating Rapid Decompensation
Administer IV sodium bicarbonate bolus if QRS >100 ms or hypotension occurs even if the pH is unknown.
Treat hypotension with a fluid challenge. Administer sodium bicarbonate if the fluid challenge is unsuccessful, using norepinephrine or dopamine for refractory cases.
Neurologic and Respiratory Effects
Medication can have effects on the neurologic and respiratory system. Often time (and supportive care) is the best treatment for these temporary effects
Seizure
Many medications can lead to seizures. Additionally, withdrawal syndromes can also present with seizures. Health care providers should be aware that seizures can be the harbinger of toxic hemodynamic instability that requires more treatment, such as in the case of anesthetic toxicity that will require rapid treatment of impending cardiac compromise with lipid emulsion therapy.
Opioids
Opioids overdose is a common problem and led to over 28,000 deaths in the US in 2014. Up to half of the deaths involve prescribed opiates. In fact, the risk of death involving opiates (prescription pain medications, heroin, and synthetics apart from methadone) increased by 9%, 26%, and 80% each. It is the most common cause of injury-related death in those between 25-60 years, more than car accidents.