Adult Opioid Overdose for Healthcare Providers
Short Description
This algorithm outlines the steps to guide the provider to efficiently assess and manage a patient with cardiac arrest due to an opioid overdose.
Algorithm at a Glance
- The provider identifies when an individual may have an opioid overdose.
- In cardiac arrest, the provider begins high-quality CPR while waiting for a defibrillator/AED and naloxone.
- Naloxone is administered as soon as it is available and then every 4 minutes as needed.
- CPR is continued, and the patient is monitored continuously.
Goals for the Management of Adult Patients with Opioid Overdose
The provider will be able to:
- Recognize an opioid-associated life-threatening emergency
- Provide appropriate treatment for an opioid-associated emergency
Opioid-Associated Emergency Algorithm for HCP
Box 1: The Patient is Assessed and EMS Activated
If outside of the hospital, the provider calls for help and sends someone for an AED and naloxone. The provider observes the patient’s respiratory status.
Box 2: Is the Patient Breathing Normally?
If the patient is breathing normally, the rescuer proceeds to Box 3. If the patient is NOT breathing normally (gasping or no breathing), they proceed to Box 5.
Box 3: Supporting the Patient
The provider maintains an open airway and prepares for transport to the emergency department. Naloxone administration should be considered if available.
Box 4: Continuous Monitoring
The provider continues to assess the patient’s breathing and level of consciousness until EMS arrives for transport.
Box 5: Does the Patient Have a Pulse?
If the patient is not breathing, the provider checks for a pulse for < 10 seconds. If there is a pulse, they proceed to Box 6. If no pulse is felt, they proceed to Box 7.
Box 6: Supporting the Patient
The provider maintains an open airway and provides rescue breathing as needed. Naloxone should be administered as soon as possible and the patient prepared for transport to the ED.
Box 7: High-Quality CPR
If only one rescuer is available, the provider performs high-quality CPR for 2 minutes before calling for help and retrieving an AED and naloxone. The provider considers the administration of naloxone if available. The team follows the Cardiac Arrest algorithm and uses the AED or defibrillator when available.
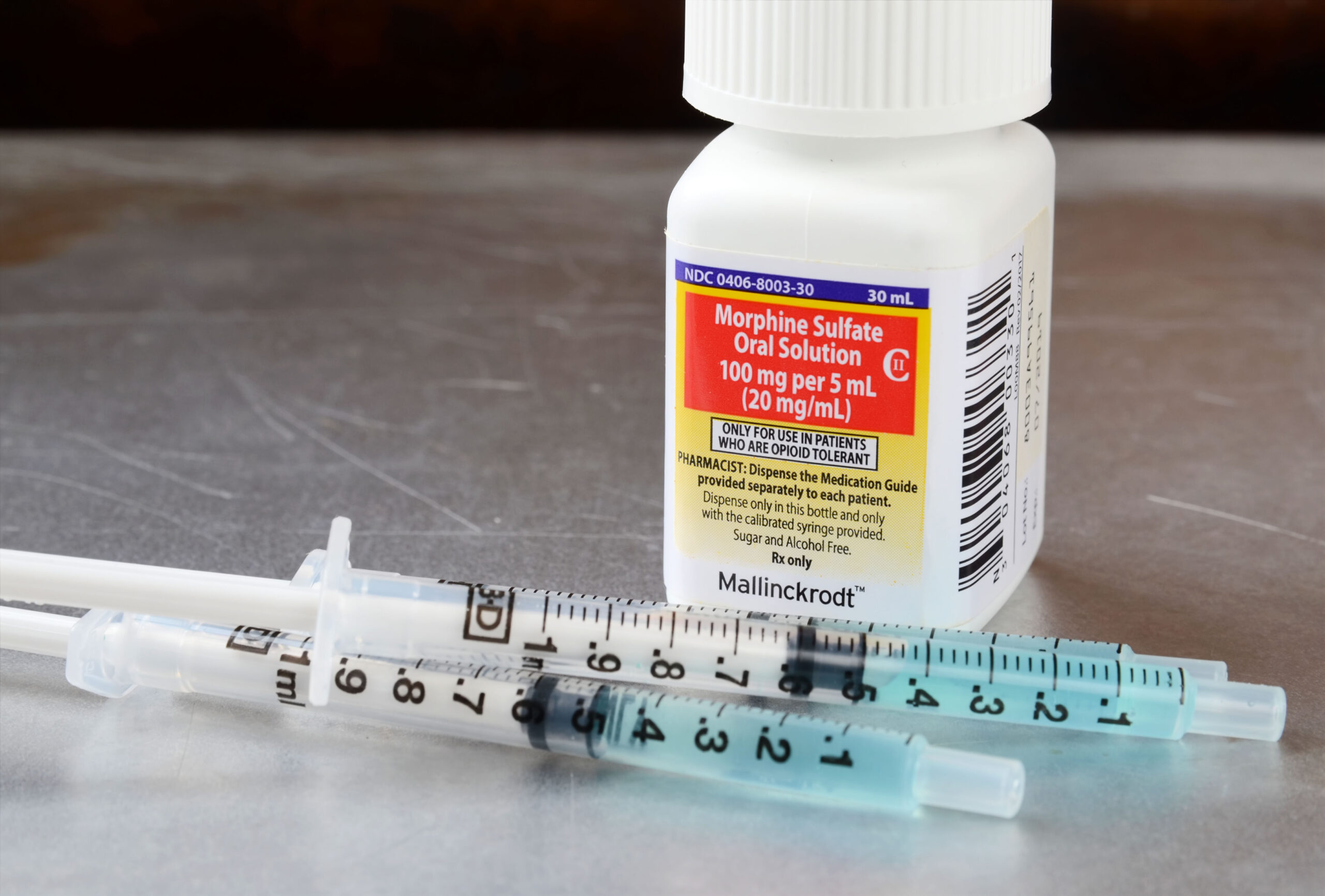
Morphine is an opiate.
Opiates affect both neurologic and respiratory function and eventually can cause both respiratory and cardiac-related arrests. Often patients will use multiple drugs or have comorbid medical or mental health conditions. Some forms of opiates- propoxyphene and methadone- may lead to torsade de pointes, and others may be cardiotoxic as well. While it is difficult to be absolutely certain that a patient is suffering from acute opiate toxicity, if clinical suspicion is high, the use of naloxone, an effective antagonist of the opiate receptor, is warranted. Naloxone opposes opiates in the central nervous and gastrointestinal systems and rapidly block neurological and respiratory toxicity. It can be given using IV, intramuscular (IM), subcutaneous, nebulized, or intranasal and endotracheal routes.
Typical signs and symptoms of opiate toxicity include depression of the nervous and respiratory systems, and miosis (pinpoint pupils). Patients may overdose intentionally, due to recreational use or accidentally via prescription or iatrogenic administration. It is vital to monitor patients closely as decompensation can occur quickly. Patients are most susceptible to respiratory compromise due to loss of reflexes protecting the airway and significant depression of respiration.
Reversing Opiate toxicity
Apart from depression of the respiratory system and respiratory arrest, opiates can lead to pulmonary edema. Naloxone is the immediate treatment of choice to reverse toxicity. It can be given in stable patients who do not have advanced airway and no significant cardiovascular impairment. While the ideal dose is not well known, some suggestions include:
- IM or IV starting dose between 0.04-0.4 mg can be successful without causing significant withdrawal symptoms. IM or IV doses can be increased to 2mg if the patient’s response is suboptimal. Repeat doses between 3-5 minutes as needed.
- For IN use, the typical dose is 2 mg with 1 mg in each nostril. Repeat doses between 3-5 minutes as needed.
- Typical nebulized doses are 2 mg in 3ml of normal saline.
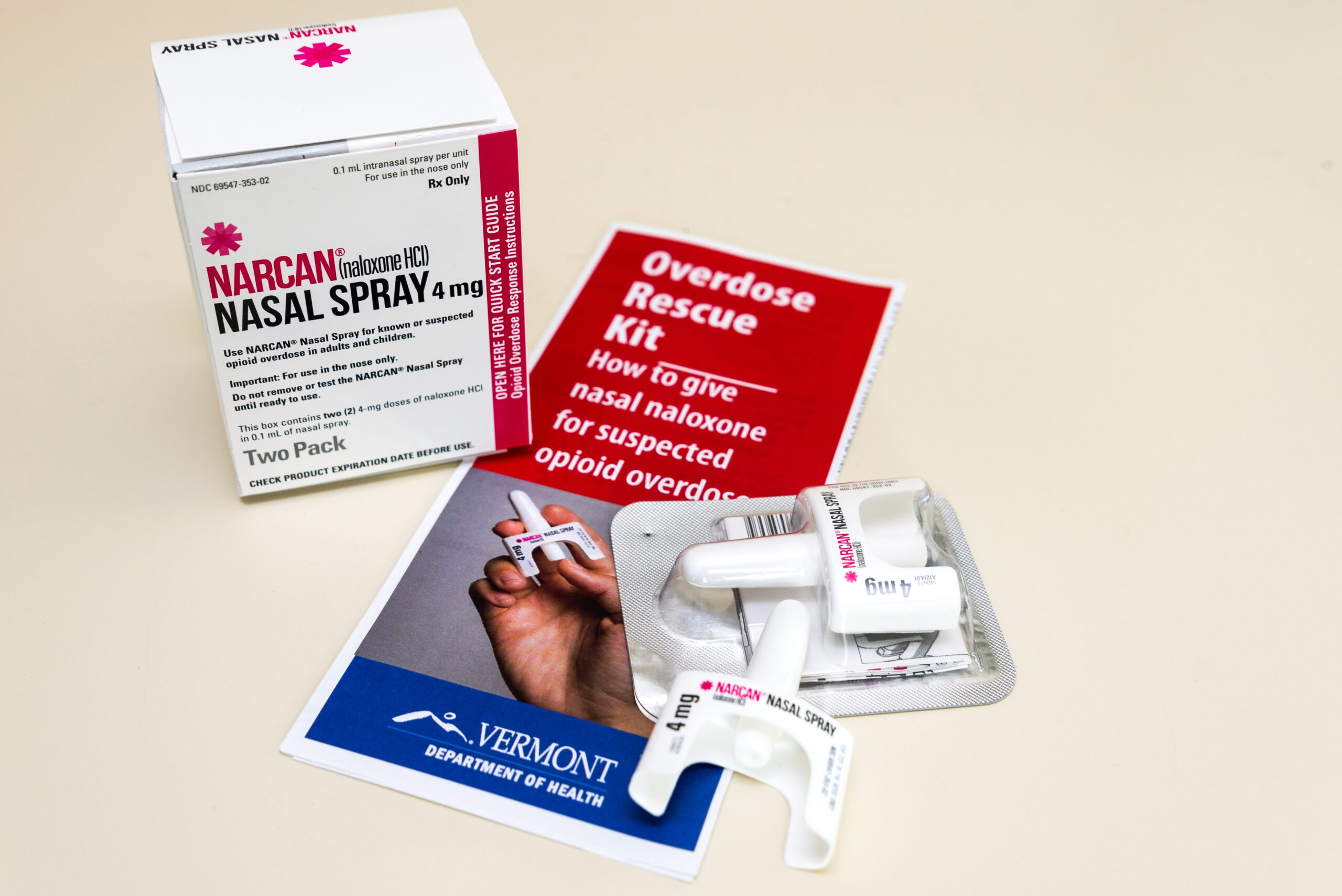
Narcan is administered intranasally.
Related Video: Understanding the Opioid-Associated Emergency Algorithm for Healthcare Providers
Opiate specific treatments include:
- Bag mask ventilation for patients with respiratory depression (but no cardiac arrest) while naloxone is prepared. (Class I, Evidence level A).
- Advanced airway placement if naloxone is ineffective
- Provided naloxone as soon as possible; do not delay for intubation. While naloxone has a short action of duration than some opiates (i.e., heroin), it is associate with under 2% adverse events and is usually effective. Additionally, repeated doses can be given if symptoms recur.
- Increased doses may be required for propoxyphene
- Increased dose up to 6-10 mg may be required for significant opiate toxicity or the use of fentanyl and derivatives.
The goals of treatment are normal respiratory function and adequate ventilation, rather than restoration of complete alertness. Be aware that sudden withdrawal of opiates can cause reactionary arrhythmias, pulmonary edema as well as significant patient agitation.
Related Video: Understanding Opioid Overdose
Public Education on Opiate Toxicity and Naloxone Use
Individuals at high risk for opiate overdose should be educated and even trained regarding signs of toxicity as well as the use of naloxone. This instruction should be geared toward non medically trained individuals using first aid and non-healthcare BLS guidelines. Since in these guidelines, pulse checks are not encouraged, it is reasonable to give an empiric treatment of naloxone alongside first aid care. Family members and bystanders who have naloxone in a known situation of overdose with observed respiratory compromise or unresponsive status can provide the medication while providing resuscitation and activating EMS. These patients should receive follow up care with medical services.