Defining Stroke
Strokes or cerebrovascular accidents occur due to a sudden loss of blood flow or sudden bleeding in part of the brain. These two definitions subdivide strokes into ischemic and hemorrhagic events. This classification is vital as it drives the initial treatment of stroke. While the appropriate treatment for ischemia is reperfusion using recombinant tissue plasminogen activator (rtPA), this treatment is completely contraindicated in hemorrhagic strokes, as it can worsen a hemorrhagic stroke and cause death. The vast majority of strokes are ischemic (87%), while less are hemorrhagic (13%), which are further subdivided into cerebral (10%) and subarachnoid (3%). There is a higher number of male stroke patients compared to females in those 55-64 years (1.25: 1), 65-74 years (1.5:1), 75-84 years (1.07:1). This reverses in those 85 years and over with a male to female ratio of 0.76:1. African Americans and Hispanic Americans are more likely to have a new stroke compared to European-Americans.
Related Video: What is Involved in General Stroke Care?
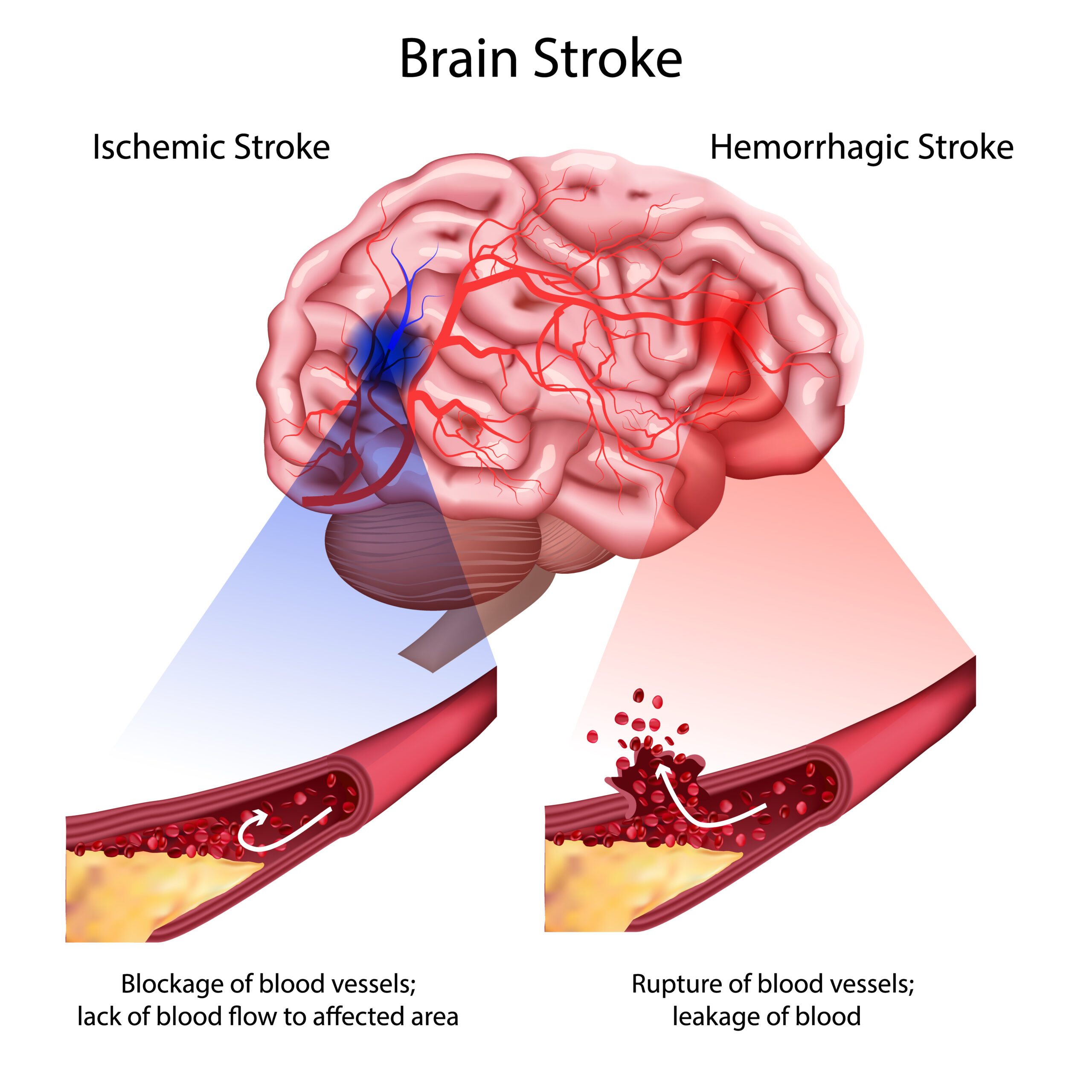
Ischemic and Hemorrhagic Stroke
Stroke: Ischemic
In ischemia, the blood supply is decreased or completely lost due to a blockage in the arterial blood flow. It typically is slower in onset than a hemorrhagic stroke. There are certain categorizations of ischemic stroke:
- Thrombotic: this is secondary to a clot that acutely obstructs the arterial lumen. It usually occurs with a background of chronic narrowing of the lumen, endothelial dysfunction, or both conditions. It is quite similar to ACS, except it occurs in the brain.
- Embolic: this is secondary to a material (usually an unstable clot) passing through the arterial lumen and causing an acute obstruction. The source can be cardiac, such as in the case of atrial fibrillation, acute MI, valvular disease, or endocarditis.
- Hypoperfusion: this refers to low blood flow states or temporary loss of blood flow that recovers. This type of stroke can occur following recovery from cardiac arrest.
- Transient ischemia attack (TIA): this is a temporary loss of blood flow that leads to specific neurologic signs that resolve. There is no lasting neurologic deficit and most resolve in under one hour.
- Reversible ischemia neurologic deficit (RIND): this is similar to TIA, but specifically indicates a resolution of symptoms by 24 hours after onset. If symptoms persist more than 24 hours, the patient has had a stroke. Importantly, up to 60% of patients with TIA/RIND will have signs indicating infarction on advanced assessment.
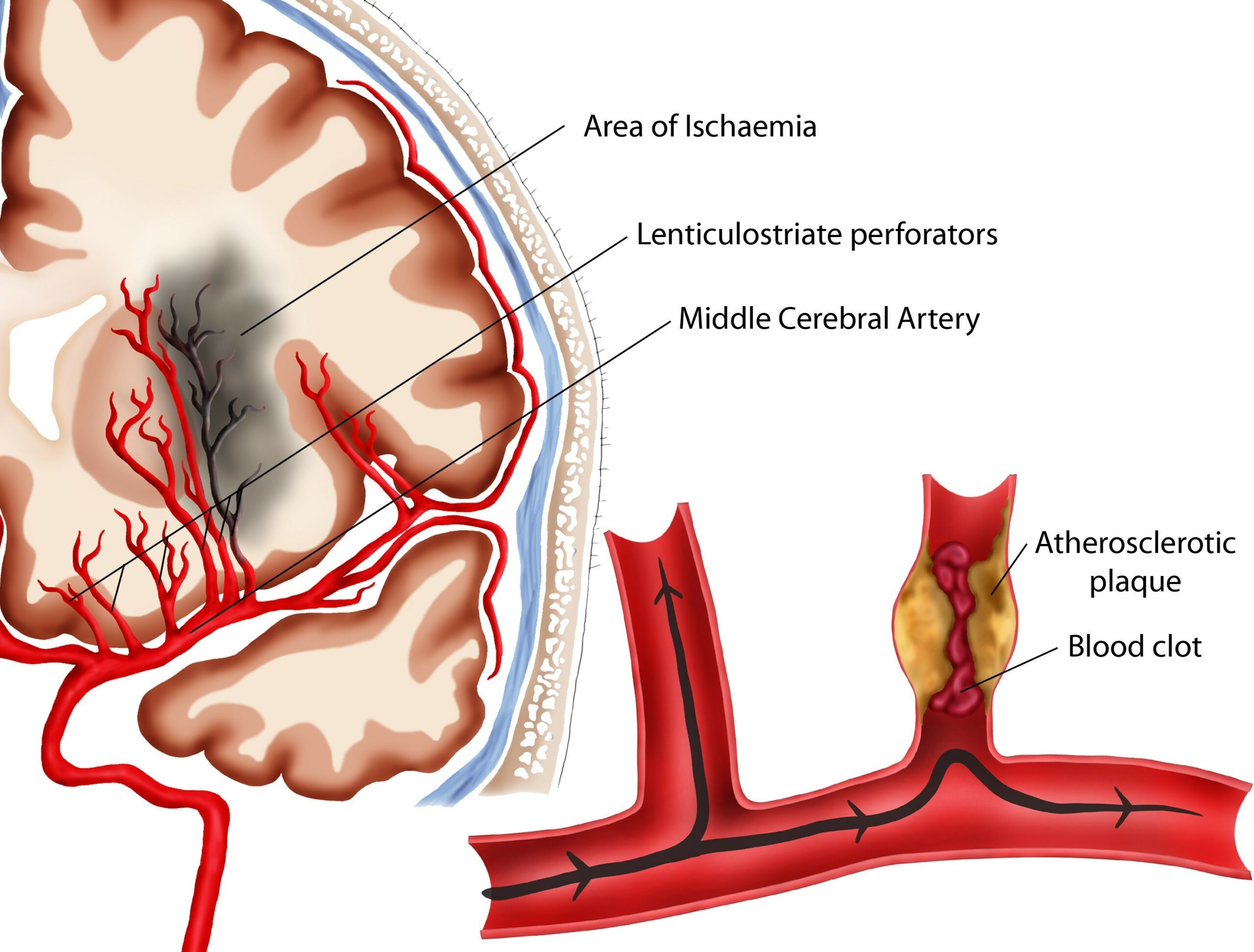
Middle Cerebral Arterial Occlusion by Thrombus
Ischemic strokes can also be classified based on the location of obstruction:
- Anterior stoke (carotid artery): obstruction occurs in the outflow of the carotid artery. The cerebral hemisphere is usually affected. This is more common, occurring in 80% of patients.
- Posterior stroke (vertebrobasilar artery): obstruction of the outflow of the vertebral and basil arteries. The brain stem and cerebellum are usually affected.
Strokes: hemorrhagic
In hemorrhage, an acute bleed causes the stroke. Typically, this is following rupture of a blood vessel with bleeding affecting the local brain tissue. The brain is affected by trauma, mass effect with increased intracranial pressures, reactionary vascular spasms, released chemical mediators, and downstream loss of blood flow. The two categories are:
- Intracerebral (10%): this occurs in brain tissue, usually due to damage to the small intracerebral arteries. A major risk factor is chronic hypertension. Additionally, amyloid angiopathy is a major risk in elderly patients.
- Subarachnoid (3%): this occurs in the subarachnoid space, from damage to the cerebral blood vessels. If the damage is in cerebral arteries, there is a sudden and rapid increase in pressure leading to severe symptoms. Commonly these cases are secondary to an aneurysm. Arteriovenous malformation causes a minority (about 5%).