Maternal-Fetal Physiologic Changes
Uterine-placental Perfusion
The 40% increase in cardiac output helps sustain the 1/3 of outflow to the uterus and placenta. The placenta has low resistance, so the perfusion pressure is needed to maintain blood flow to this area. If the mother becomes hypotensive and perfusion pressure is compromised, there will be an immediate loss of flow to the placenta and the fetus. Reversing hypotension is key to both mother and fetus survival.
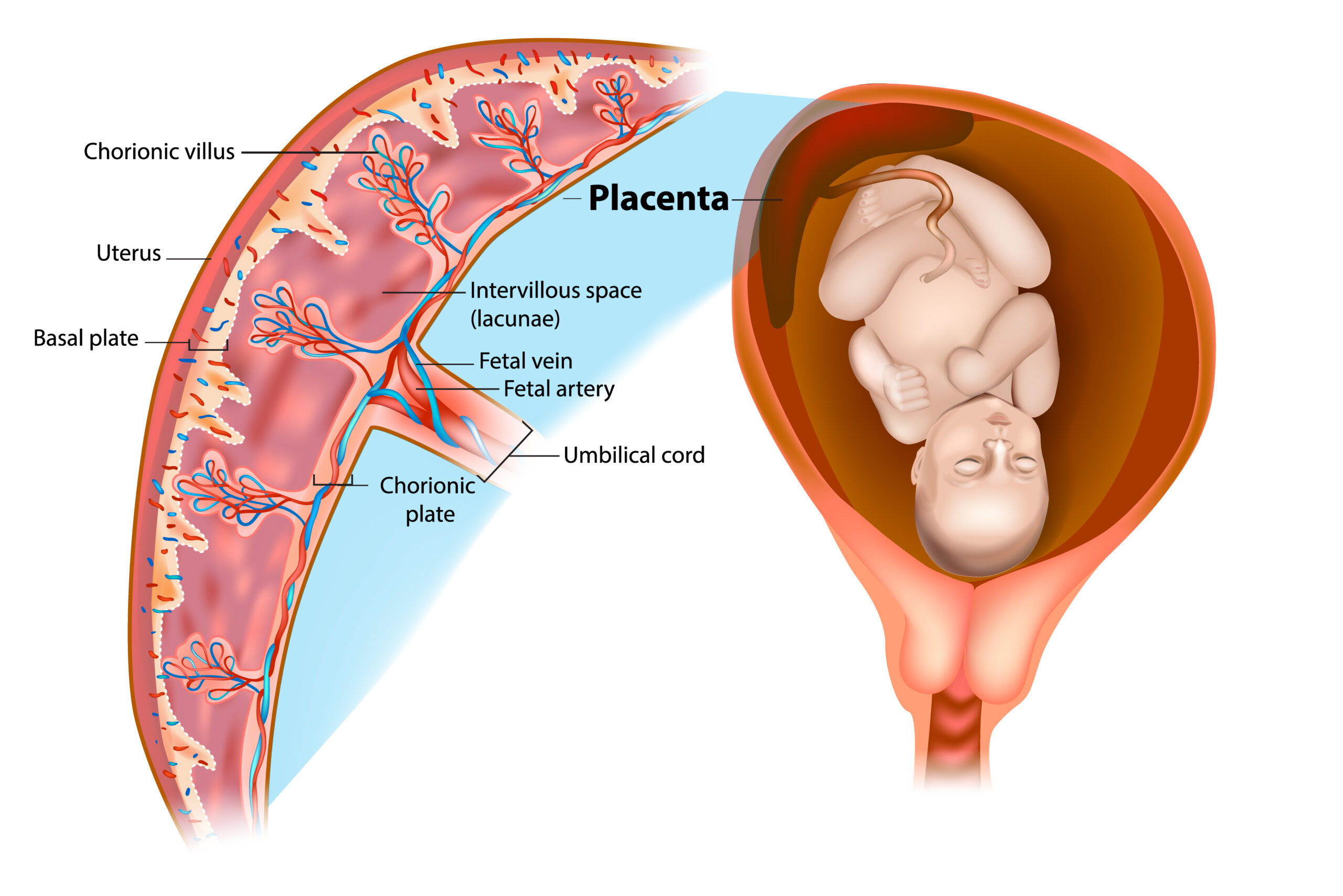
Placental Blood Circulation
The Uterus
The increasing size of the uterus begins to have a vascular effect around 20 weeks gestation. The uterus compresses both the IVC and the aorta, reducing venous return and systemic outflow, respectively. This can be noticeable when the pregnant woman lays supine. In cardiac arrest, the uterus can make resuscitation attempts more difficult. The IVC obstruction requires all IV medications to be given via supradiaphragmatic veins. If severe, IV administration may not be effective without the delivery of the fetus.
Maternal Physiology
The physiologic changes in pregnancy make the mother less likely to tolerate hypoxia or acidosis. Physiologic anemia reduces the oxygen-carrying capacity due to lowered hemoglobin (even despite normal PaO2 or SpO2). As the uterus enlarges, the elevated diaphragm reduces both functional residual capacity (FRC) and volume (FRV), making the patient more susceptible to desaturation if hypoxia occurs. Additionally, supine positioning, decreasing FRC further opposes an attempt at ventilation and oxygenation.
Pregnancy-related respiratory alkalosis also makes the patient more susceptible to acidosis. Laryngeal edema makes intubation difficult, and increased blood flow to the area may increase the risk of bleeding and subsequent obstruction. The progesterone associated relaxation of the esophageal sphincter increases the risk for aspiration. Consequently, even in a stable patient, intubation can be complicated. Unsuccessful intubation is likely higher in pregnancy due to these complications. Pregnant women are always considered to have difficult airways.
Fetal Physiology
Fetal hemoglobin binds oxygen more effectively than adult hemoglobin, leading to a relatively higher SpO2 at the same PaO2. As a result, the fetus may have an advantage early on during maternal arrest. Additionally, cardiac output is greater per kilogram compared to cardiac output following birth. While there is no current research on the effect on the fetus from maternal CPR, old research suggests that fetuses of primates can survive 7 minutes following asphyxiation without neurologic damage. It is recommended that delivery occurs within 5 minutes following arrest to reduce risk to both fetus and mother. However, the research behind this is poor and recent research suggests the time before a neurologic compromise is actually closer to 15 minutes. The fetus at older gestational age will likely do better than the younger fetus.
Improving Cardiovascular function of the Mother
Moving the Uterus
Chest compressions are limited with the uterus compressing the IVC and the aorta, which limits flow to both the heart and the brain. Recent research indicates that positioning can aid in this regard. MRI evaluation of stroke volume reveals that when shifting the 20 weeks gestation, pregnant patients to a left lateral tilt will increase stroke volume by almost 30%. At 32 weeks gestation, the increase is 35%, while the increase in cardiac output is 24%.
Manual displacement
The uterus can be manually displaced to relieve IVC compression. In the patient undergoing cesarean section, manually displacing the uterus to the left compared to a 15 degree left tilt decreases hypotension and the need for ephedrine. This manual displacement may allow supine positioning for effective CPR while reducing relieving IVC compression.
To accomplish manual displacement
- Stand to the left of the patient at the level of the uterine fundus
- Reach with both hands across the patient and pull the uterus to the left and up.
- (if unable to stand at the patient’s left, push the uterus up and to the left with one hand)
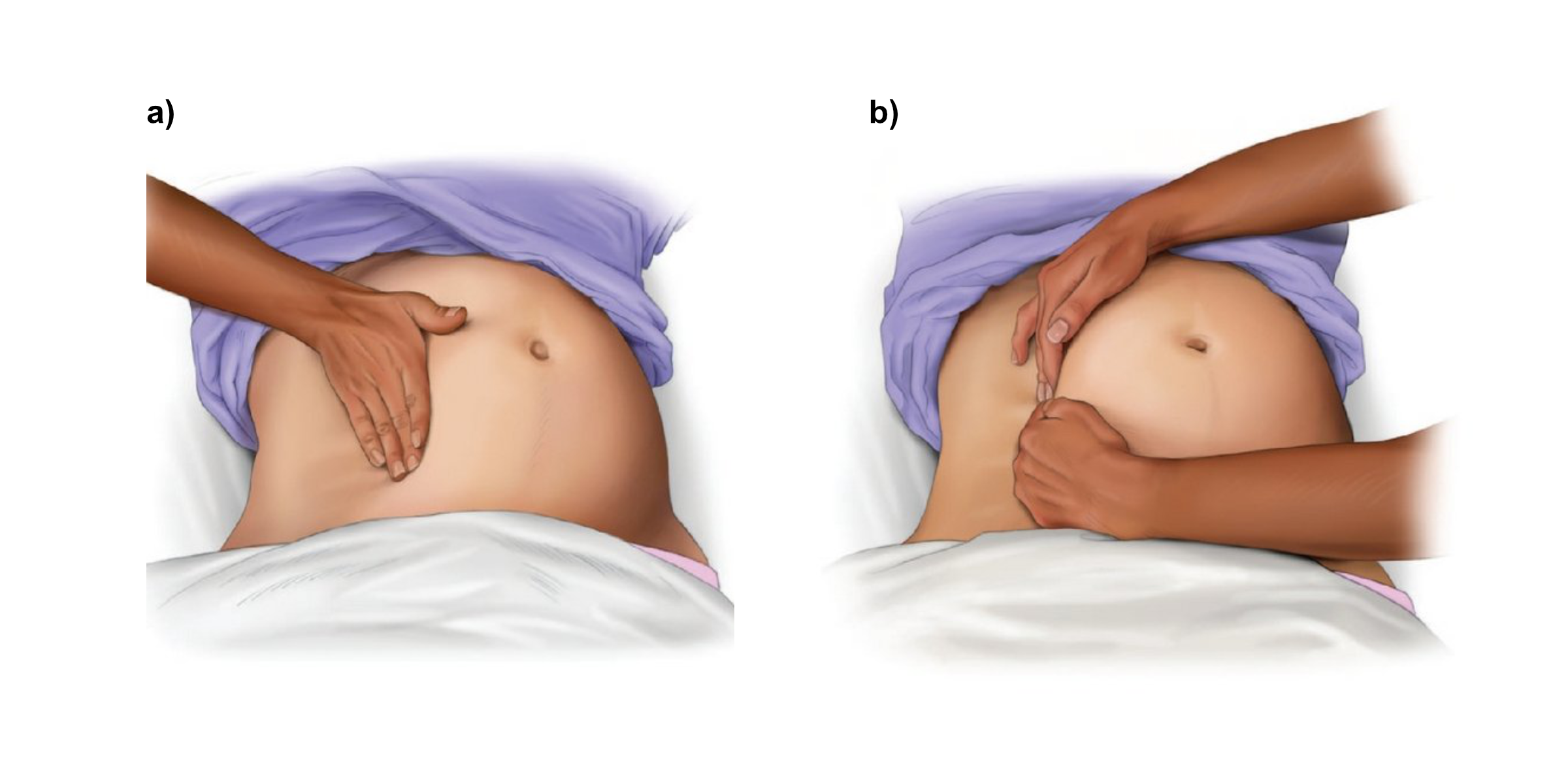
Manual Displacement of the Uterus
Left lateral Tilt Compressions
One option for reducing venous compression in the pregnant woman is to use left lateral tilt positioning. However, this is not ideal for chest compressions due to the angle and associated decrease in the compression force. There is no good research looking at this method of providing compression. Due to the ability to maintain supine position when manual displacing the uterus to the left- and the easier provision of other resuscitation care- this is preferred to the left lateral tilt positioning.