Emergent and Life-threatening Asthma
Pathophysiology
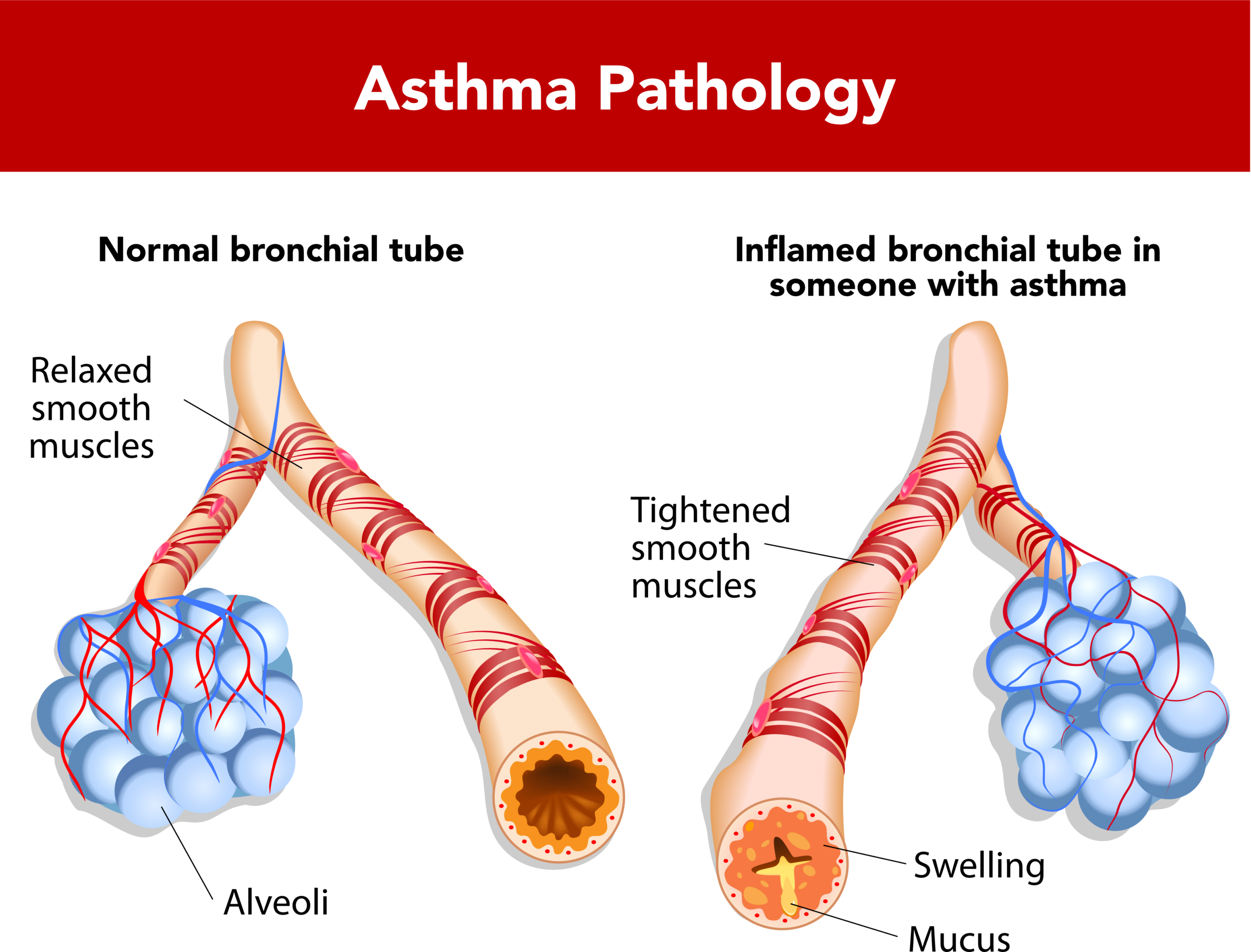
Asthma occurs due to three major pathophysiologic conditions:
- Inflammation of the airway
- Bronchoconstriction
- Impaction of mucus
Severe asthma can lead to respiratory arrest, leading to cardiac arrest and death. In these cases, it is usually caused by acute bronchospasms that lead to airway plugging with mucus. Associated findings at autopsy include airway muscle hypertrophy, airway edema, plasma protein exudate, and inflammatory mediators. As one of the mainstays of treatment is inhaled beta2 agonists that relax the bronchial smooth muscle, it is thought that bronchospasms play a major role in the disease.
Asthmatic Changes
Related Video: Asthma Exacerbation Pathophysiology
Both bronchospasm and obstruction of the airway with mucus leads to airway hyperinflation as well as increased resistance. The consequence is an increase in the work associated with breathing. In mechanically ventilated patients auto- positive end expiration pressure (auto-PEEP) may develop. The inspiration tidal volume is larger than the expiration tidal volume leading to an always increasing lung volume. The excess lung volume causes increased thoracic pressure (or auto-PEEP), reduced venous return, and subsequent hemodynamic instability due to reduced cardiac output. Severe asthma emergencies can be life-threatening, especially if certain complications are evident, including pneumomediastinum, pneumothorax, pneumonia, cardiac dysfunction, pulmonary edema, and lobar atelectasis.
Diagnosing life-threatening Asthma
This disease is more common in:
- African-American males;
- Urban and low socioeconomic status
- Patients with baseline severe or steroid-dependent asthma;
- Patients with recent asthma-related complication (i.e., hospitalization, intubation);
- Patients diagnosed before 5 years old;
- Patients delaying care due to minimizing, self-treatment, or lack of awareness regarding severity.
Related Video: Patient History – Asthma Exacerbation
Patients are more likely to present at night and either nearing arrest or after hours of failed therapy.
Related Video: What is an Asthma Exacerbation Physical Exam?
Triggers for Asthma
Several triggers can be identified both to guide treatment as well as to minimized future exposure or seek early treatment if encountered in the future.
- Environmental triggers including extreme heat or cold, increased humidity, smoke/cigarette exposure
- Upper respiratory infection
- Allergies (pollen, mold, dust)
- Exercises
- Comorbid conditions (i.e., acid reflux, COPD)
- Medications (Beta-blockers, NSAIDs, aspirin)
No triggers may be found, and some patients have significant exacerbations despite documented compliance with their treatments.
Disease Severity
Patients are not necessarily accurate in determining the severity of their disease. There is not a good correlation with the patient’s subjective severity and objective scores. Some patients additionally may have a muted response to high CO2 and low oxygen and be unaware of the severity of the disease.
Additionally, wheezing may not be a good indicator of the severity of airway disease as very severe disease may be associated with a lack of air movement and lack of wheezing. A “silent” asthmatic is particularly concerning, and the onset of wheezing may actually indicate improvement.
Upright posture and accessory muscle use suggest a risk of respiratory failure. Confused mental state, drowsiness or exhaustion indicate imminent arrest. Scoring asthma severity based on objective findings (symptoms, signs, and laboratory evaluation) is more reliable at diagnosing severity. The use of a peak flow meter is a useful tool to assess asthma severity in adults who can cooperate and should be a routine assessment in asthma patients.

A peak flow meter assesses how well a person’s asthma is controlled.
Differential
Other conditions must be differentiated from asthma that can lead to shortness of breath and wheezing:
- Primary cardiac illness (i.e., heart failure, myocarditis)
- Emphysema
- Upper airway obstructions
- Pneumonia
- Anaphylaxis causing bronchospasms
- Pulmonary edema
- Pulmonary emboli
- Chronic and obstructive pulmonary disease (COPD)
Systemic signs such as urticaria make anaphylaxis more likely. At the same time, medications, including Beta-blockers, opiates, and cocaine, may mimic the bronchospasm of asthma. Additionally, abruptly stopping corticosteroids can lead to severe asthma.
Oxygen Saturation levels can mislead
- SaO2 may not accurately reflect worsening alveolar hypoventilation, especially if O2 is being supplemented.
- SaO2 can drop during beta-agonist treatment as this causes airway and vascular dilation that can lead to intrapulmonary shunts