Monitoring during Oxygenation and Ventilation
Respirations provided by responders must achieve good oxygenation as well as ventilation.
- Oxygenation allows the arterial blood to maintain adequate oxygen levels.
- It is monitored by pulse oximetry.
- Ventilation promotes the removal of CO2 from the venous blood.
- It is monitored by capnography or capnometry.
Oximetry Principles
When monitoring oxygenation, responders must understand the principles of oxygenating tissues rather than simply memorizing normal oximetry values.
Physics of Oximetry
Oximetry uses the fact that the way light is transmitted through the fluid it is dissolved in, which in this case is blood, indicates its concentration. Consequently, the light transmitted in oxygenated and non-oxygenated blood is different. Specifically, oxygenated hemoglobin will absorb infrared light, while deoxygenated hemoglobin absorbs mostly red light. Oximetry transmits both infrared and red light through a tissue bed (e.g., the finger or ear), allowing the photodetector on the other side to capture the light that is not absorbed. In this way, the oximeter detects the relative percentage of oxygenated and deoxygenated hemoglobin in the tissue. If the patient does not have any abnormal hemoglobin (e.g., methemoglobin) and there is a 70% or greater oxygen saturation, there will be at most a 3% difference between the pulse oximeter reading and arterial blood gas measurements. Therefore, its accuracy in most situations makes pulse oximetry a useful tool in hospital and emergency department settings. It is also useful in identifying ROSC when a normal plethysmograph waveform is detected.

Pulse Oximeter Attached to Finger
Oxygen Delivery in Hemoglobin and Tissue
Obtaining arterial blood gases is impractical during acute cardiac arrest. And, because of decreased blood flow, pulse oximetry is not sensitive enough to detect oxygen in the peripheral tissues during a cardiac arrest.
Instead, pulse oximetry is useful in patients who have not arrested but still need continuous monitoring of oxygen saturation levels. Optimal oxygen saturation depends on three things:
- Enough available oxygen saturating the hemoglobin
- Enough hemoglobin to transport oxygen molecules
- Enough cardiac output to transport hemoglobin that is saturated with oxygen to the periphery
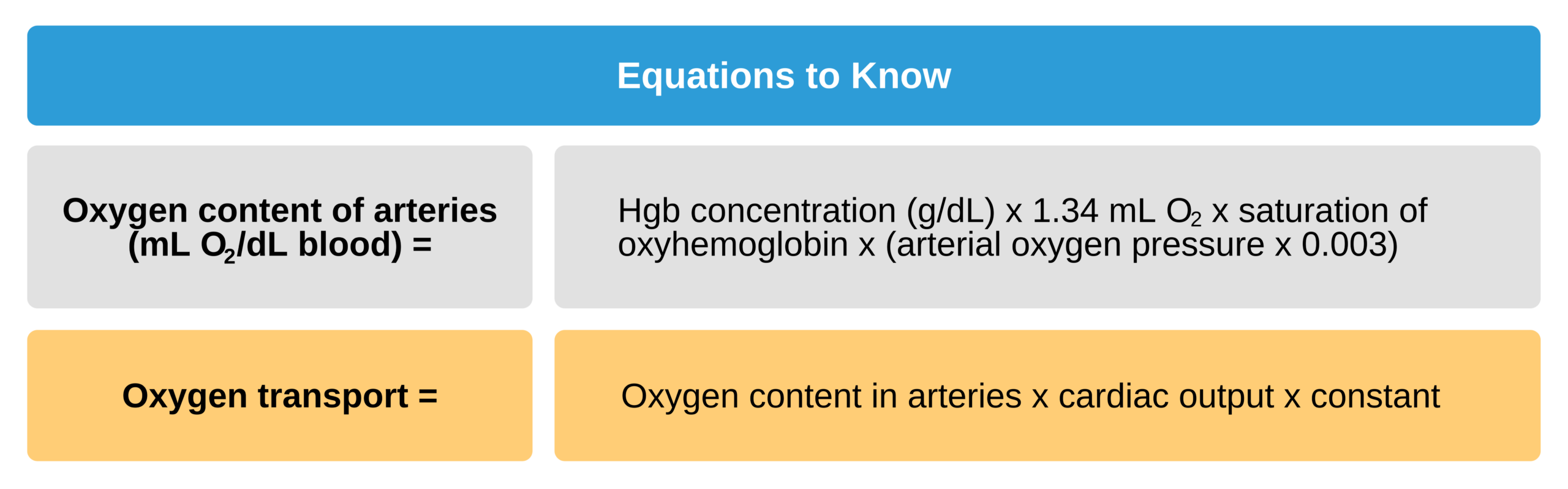
The total oxygen content in arterial blood is determined by the concentration of hemoglobin as well as the oxygen saturation. Unfortunately, pulse oximetry does not approximate oxygen delivery because it does not take into account the oxygen content (specifically the amount bound to hemoglobin and dissolved oxygen) or the cardiac output.
The average oxygen content of the arterial blood supply is between 18 and 20 mL/dL. In addition to measuring oxygen content, it is vital to determine if oxygen can be effectively transported to the tissues that need it. Cells in peripheral tissues should be able to take up and use oxygen for metabolism.
Limitations of Pulse Oximetry
When monitoring pulse oximetry, the clinician must keep in mind the patient’s cardiac output and oxygen transport and ensure adequate perfusion and hemoglobin concentration. If either of these values is low, oxygen transport will be suboptimal regardless of the pulse oximetry reading.
Hemoglobin Abnormalities (e.g., poisoning from carbon monoxide)
Abnormal types of hemoglobin, such as carboxyhemoglobin from carbon monoxide or methemoglobin from cyanide, do not absorb light in the same way as regular hemoglobin. Therefore, pulse oximetry does not recognize these types of hemoglobin.
If a patient has abnormal hemoglobin in their blood, the oxygen saturation will be inaccurately high as it will only evaluate the percent of normal oxygenated hemoglobin rather than the total oxygenated hemoglobin (which would include the abnormal hemoglobin). Therefore, if there is a suspicion of poisoning that involves abnormal hemoglobin, it is best to obtain an arterial blood sample.
Inaccuracies in Pulse Oximetry
Some clinical conditions will cause abnormal pulse oximetry results. Be aware of these complicating factors (the first two being the most commonly seen):
- Poor perfusion of the periphery from hypotension, decreased cardiac output, vasoconstriction, hypothermia, etc.
- Excess motion such as agitation, twitching movements, or patient transport
- Oxygen saturation < 70%
- Significant anemia with hemoglobin < 2 or 3 g/dL
- Dark-skinned individuals, polish on the nails, or infections that obscure the surface of the nails
When using pulse oximeters, remember these important safety precautions:
- Do not use cracked oximeter probes as their lights touching the skin can lead to burns.
- Do not mix and match oximeter probes from one company with the base unit from another company.