Adult Survival Chain
The survival chain refers to the integrated systems of care needed to treat a cardiac arrest patient. There are two chains depending on the location of the arrest (in the community or in the hospital).
Regardless of location, the survival chain culminates in the hospital, often in a high-level department such as an ICU, where post-cardiac arrest care emphasizes high-level monitoring and focused management of the patient’s temperature.
The key to the success of a survival chain is the knowledge that cardiac arrest can happen anywhere in the community or within the hospital. Consequently, the responder should be quick to recognize and treat the situation wherever it occurs.
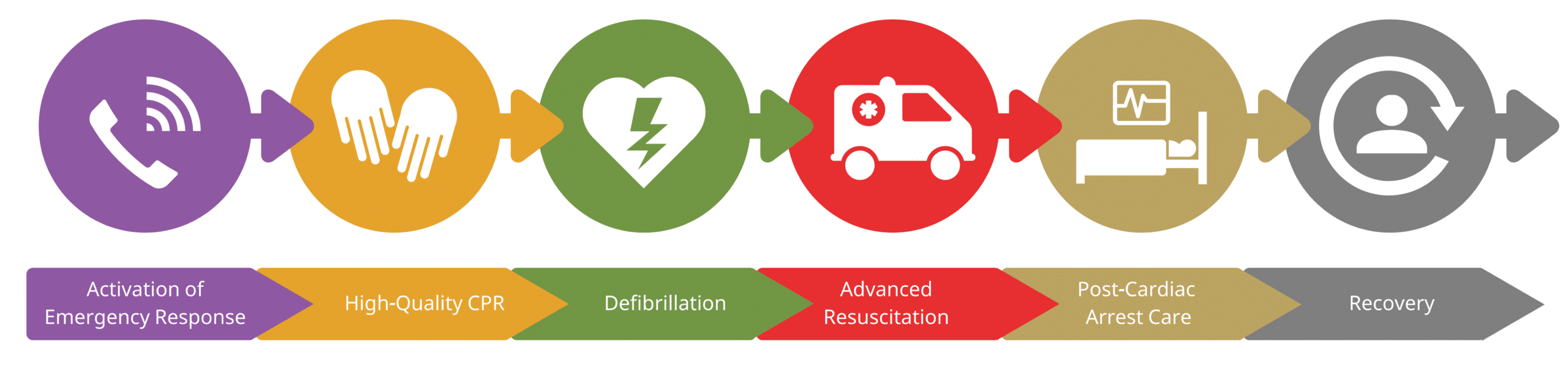
Out-of-Hospital Cardiac Arrest (OHCA)
1st Link: Recognizing Arrest and Activating EMS: Phone Icon
As soon as cardiac arrest is evident, the responder activates emergency medical services (EMS). The steps include:
- The responder must recognize collapse and activate EMS.
- The EMS dispatcher responds and recognizes a potential cardiac arrest, initiating the appropriate emergency response (BLS or ACLS).
- EMS responders arrive and take over care of the patient.
The key to this is early recognition of the event and early initiation of CPR. This can be accomplished by a layperson or by a readily available CPR-trained individual.
Key Takeaway
Early recognition of cardiac arrest results in early CPR and improved outcomes.
It is key that responders do not delay CPR because the cardiac arrest is not recognized. Mechanisms for early recognition and emergency response initiation must occur promptly.
Responders need to notify EMS quickly for success. Calling 911 is an easy first step that reduces the wait time for an effective treatment for cardiac arrest patients. Dispatchers must be well trained and able to help the layperson determine if a patient is likely to have a cardiac arrest.
Importance: ACLS training programs prepare millions of responders to care for potential cardiac arrest patients and save lives.

Calling 9-1-1 is one of the first steps to activate emergency medical services (EMS).
2nd Link: High-Quality CPR: Hands Icon
High-quality CPR with excellent chest compressions is the key to saving lives. This is important in the community as well as hospitals where non-clinical employees should also be aware of high-quality CPR techniques.
CPR is based on cycles of 30 chest compressions and 2 breaths with a basic airway, followed by continuous compressions and a breath every 6 seconds with an advanced airway. A critical component is limiting unnecessary interruptions in compressions and ensuring pauses are limited to 10 seconds or less.
Research confirms early CPR is necessary to save lives. In OHCA, bystander CPR almost doubles the survival rate. Untrained laypersons should deliver hands-only CPR, which is almost as effective as traditional CPR with breaths in adults. Traditional CPR is more effective for those with respiratory arrest as the cause (especially important in children).

Community Member Performing CPR
For OHCA, 23% have VF or pulseless VT, while in the hospital, this rate is 17.6%. Consequently, many of these patients do best with immediate CPR and defibrillation within 5 minutes of arrest.
Key Takeaway
Community providers must be trained in CPR and how to use the AED to decrease out-of-hospital deaths.
In OHCA, as EMS personnel may not arrive on the scene within 5 minutes, more laypersons must be trained on providing effective CPR and AED use to reach these time goals. EMS dispatchers should question the caller to determine if the patient is likely to be in cardiac arrest. They can then give instructions for untrained laypersons to provide hands-only CPR and help them with AED use.
Related Video: One Quick Question: Should You Choose CPR or Defibrillation?
3rd Link: Defibrillation: Heart Icon
Early defibrillation is key for patients with a shockable rhythm, such as acute VF or pVT. The goal is to provide defibrillation with 3 to 5 minutes of arrest, as this improves survival rates.
Key Takeaway
The goal is to provide defibrillation within 3 to 5 minutes of arrest in patients with a shockable rhythm.
Prompt CPR and defibrillation received within this period can increase survival rates to between 41% and 74%. Quick defibrillation improves survival in patients with shockable rhythms. For every minute that passes without the use of an AED for defibrillation, the survival rate decreases by up to 10% (although interval CPR mitigates this rate of decline). Since AEDs have been placed in public spaces such as airports, casinos, and airplanes, sudden cardiac death rates have decreased.
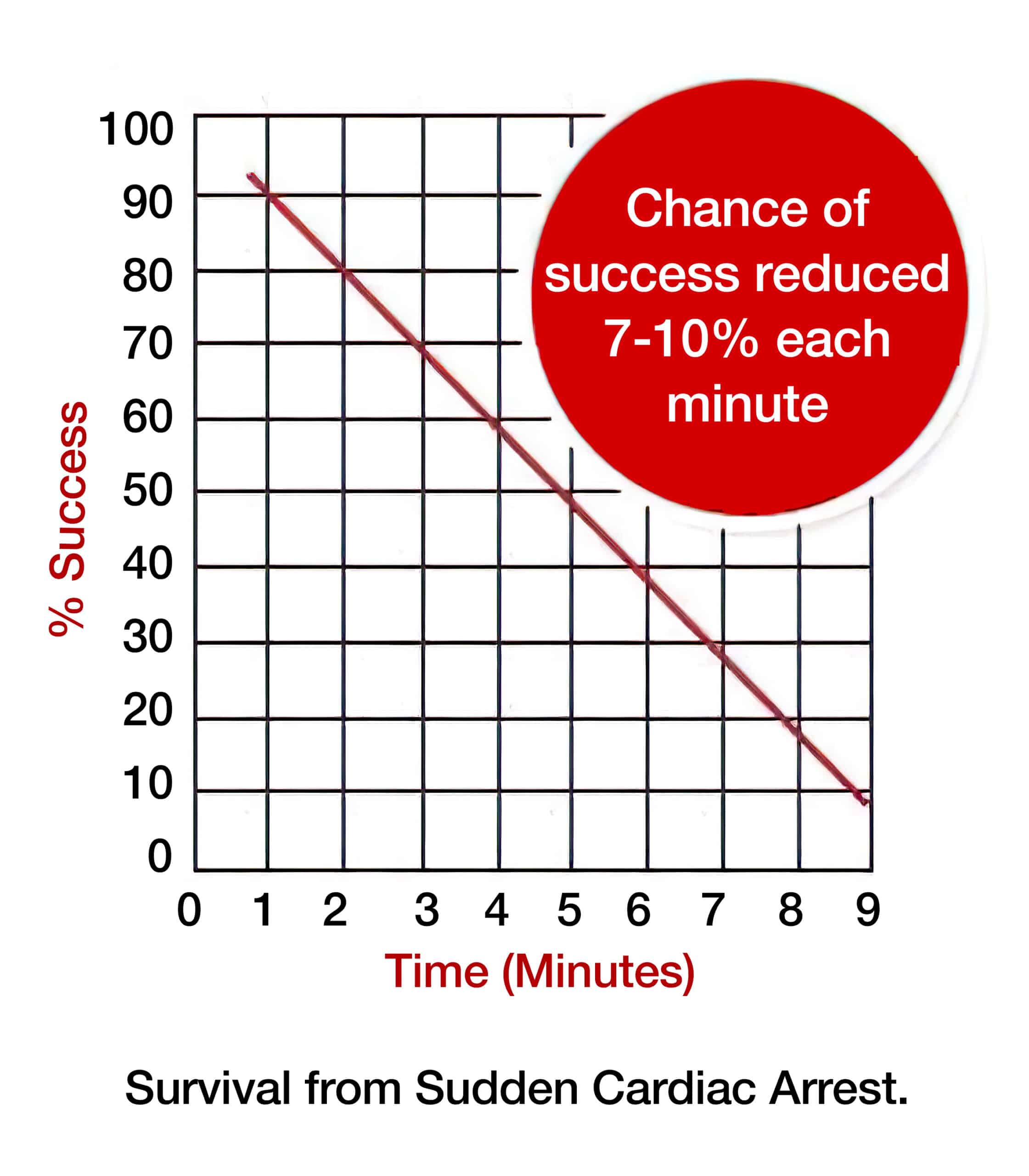
Time to Defibrillation and Survival
All major health organizations that monitor resuscitation efforts (the AHA, European Resuscitation Council, and the International Liaison Committee on Resuscitation) recommend early defibrillation. All EMS vehicles are equipped with and have responders who can use AEDs.
Responders must provide early CPR to augment the benefits of AED use. Unfortunately, delays beyond 3 to 5 minutes continue to occur secondary to some hospitals’ reluctance to purchase AEDs for use within the hospital.
4th Step: Excellent Advanced Care: Ambulance Icon
Excellent care for the cardiac arrest patient requires an integration of BLS and ACLS. Outside of the hospital, EMS responders must be well trained in BLS, but at least one, and preferentially two, EMS responders should be able to provide ACLS. The participation of two or more ACLS providers is associated with at least a 20% increased survival rate in patients with VF.
In the hospital setting, ACLS must also be integrated into code situations, allowing a seamless transition from ongoing CPR to advanced techniques.
5th Link: Post-Arrest Treatment: Bed Icon
Following the acute management of cardiac arrest, integrating multiple areas of care, such as cardiovascular, metabolic, and neurologic care, is instrumental in increasing survival rates following ROSC.
The primary goals of post-arrest treatment are:
- Maintaining cardiovascular perfusion
- Appropriate transport of the OHCA patient to a facility that can maintain an appropriate level of care or the IHCA patient to an intensive care unit
- Defining and managing the cause of cardiac arrest while preventing recurrence
The secondary goals of post-arrest treatment are to:
- Maintain body temperature that optimizes neurologic function and survival
- Manage existing ACS
- Manage mechanical ventilation and reduce organ injury
- Maintain organ function and take steps to decrease organ injury
- Determine recovery prognosis
- Transition to the appropriate rehabilitation service.
6th Link: Recovery
The final link includes rehabilitation assessment and treatment before hospital discharge. This recovery link involves assessing the needs and providing rehabilitation services for both the patient and their family.
These efforts involve assessment of:
- Cardiopulmonary status
- Neurologic status
- Return to work
- Post-traumatic stress
- Fatigue
Cardiac Arrest in the Hospital
For cardiac arrest patients within the hospital, excellent surveillance is required for prevention. It includes tools such as rapid response and the identification of early warning signs. This is most important on the general medicine floors. For those patients who progress to cardiac arrest, multiple responders from different services must come together rapidly to provide resuscitation and appropriate management.
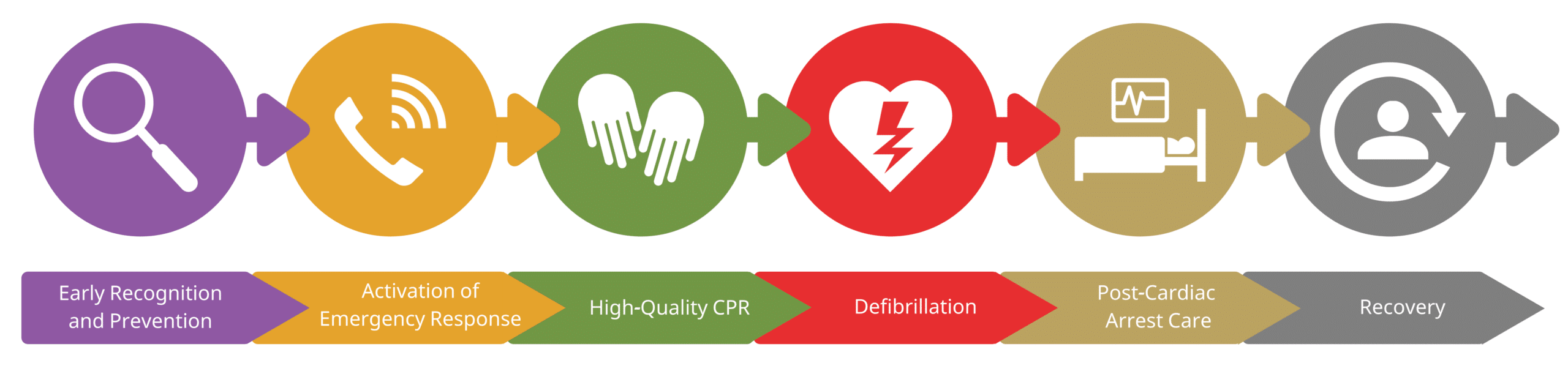
In-Hospital Cardiac Arrest Adult Chain of Survival
In-Hospital Cardiac Arrest (IHCA)
1st Link: Recognizing Arrest: Magnifying Glass Icon
As soon as cardiac arrest is evident, responders call for help.
The steps include:
- The responder must recognize collapse
- In IHCA, families can be trained to recognize signs of cardiovascular distress before a cardiac arrest occurs.
- Rapid response team members arrive and begin administering care.
The key to this is early recognition of the event and early onset of CPR. This can be accomplished by a readily available CPR-trained individual.
Key Takeaway
Early recognition of cardiac arrest results in early CPR and improved outcomes.
2nd Link: Activating Resuscitation Team: Phone Icon
Patients in cardiac arrest do best with immediate CPR and defibrillation within 5 minutes of arrest. The code or rapid response team responds and recognizes potential cardiac arrest, initiating the appropriate response (BLS or ACLS).
3rd Link: High-quality CPR: Hands Icon
High-quality CPR with excellent chest compressions is the key to saving lives. CPR is based on cycles of 30 excellent chest compressions and 2 breaths with a basic airway, followed by continuous compressions and a breath every 6 seconds with an advanced airway. A key component is limiting unnecessary interruptions in compressions and ensuring that pauses are limited to 10 seconds or less. This intervention can be provided by anyone who recognizes the cardiac arrest.
4th Link: Defibrillation: Heart Icon
Early defibrillation is key for patients who have a shockable rhythm: ventricular fibrillation or pulseless ventricular tachycardia. The goal is to provide defibrillation within 3 to 5 minutes of arrest, as this improves survival rates. For every minute that passes without defibrillation, the survival rate decreases by up to 10%. This intervention is typically provided by the in-hospital code team.
Key Takeaway
The goal is to provide defibrillation within 3 to 5 minutes of arrest in patients with a shockable rhythm.
5th Link: Post-Arrest Treatment: Bed Icon
Following the acute management of cardiac arrest, integrating multiple areas of care such as cardiovascular, metabolic, and neurologic care is instrumental in increasing the survival rate following ROSC.
The primary goals of post-arrest treatment are to:
- Maintain cardiovascular perfusion
- Appropriate transport of the cardiac arrest patient to the intensive care unit
- Identify and manage the cause of cardiac arrest while preventing recurrence
The secondary goals of post-arrest treatment are to:
- Maintain body temperature that optimizes neurologic function and survival
- Manage existing ACS
- Manage mechanical ventilation and reduce organ injury
- Maintain organ function and take steps to decrease organ injury
- Determine the patient’s recovery prognosis
- Transition to the appropriate rehabilitation service
6th Link: Recovery
The final link includes rehabilitation assessment and treatment before hospital discharge. This recovery link involves assessing the needs and providing rehabilitation services for both the patient and their family.
These efforts involve assessment of:
- Cardiopulmonary status
- Neurologic status
- Return to work
- Post-traumatic stress
- Fatigue
