Ventilating the Preterm Newborn
The preterm baby has noncompliant lungs from lack of surfactant. Consequently, the preterm newborn’s lung is prone to volutrauma, which may cause a tension pneumothorax during ventilation. A preterm infant with a heart rate of ≥ 100 bpm and spontaneous breathing does not require assisted ventilation. PPV is needed when the baby exhibits labored respiration with bradycardia or low oxygen saturation.
CPAP is an alternative to PPV if the preterm baby has spontaneous breathing and a heart rate of ≥ 100 bpm but has labored breathing and low oxygen saturation levels. Studies show that the early use of CPAP reduces the need for intubation and mechanical ventilation.13
Key Takeaway
CPAP is recommended for a preterm infant with heart rate > 100 bpm but with labored breathing and low oxygen saturation.

Preterm infant receiving CPAP.
When administering PPV to infants via an ET tube or resuscitation face mask, the PPV inflation pressure must be maintained as low as possible to gently inflate the lungs and maintain the baby’s heart rate > 100 bpm. An initial pressure of 20–25 cm H2O is recommended. Face mask ventilation with PPV should be limited to an inspiration pressure of 30 cm H2O.
Key Takeaway
PPV pressure should start at 20–25 cm H2O and should NOT exceed 30 cm H2O.
Chest rise is not a reliable indicator in premature infants, especially those that are extremely premature. Visible chest rise in these babies may actually indicate overventilation and place them at risk for a pneumothorax.
The team should rely on heart rate as the most reliable indicator of adequate ventilation. Auscultation of breaths is also helpful in evaluating effective ventilation.
When PPV via an ET tube fails to improve the preterm infant’s status, the team should suspect an airway obstruction. Leakage is the most common problem impeding effective PPV with a mask.
Simple changes in head and neck position can improve PPV quality. An ETCO2 detector can be an excellent visual indicator of PPV delivery.
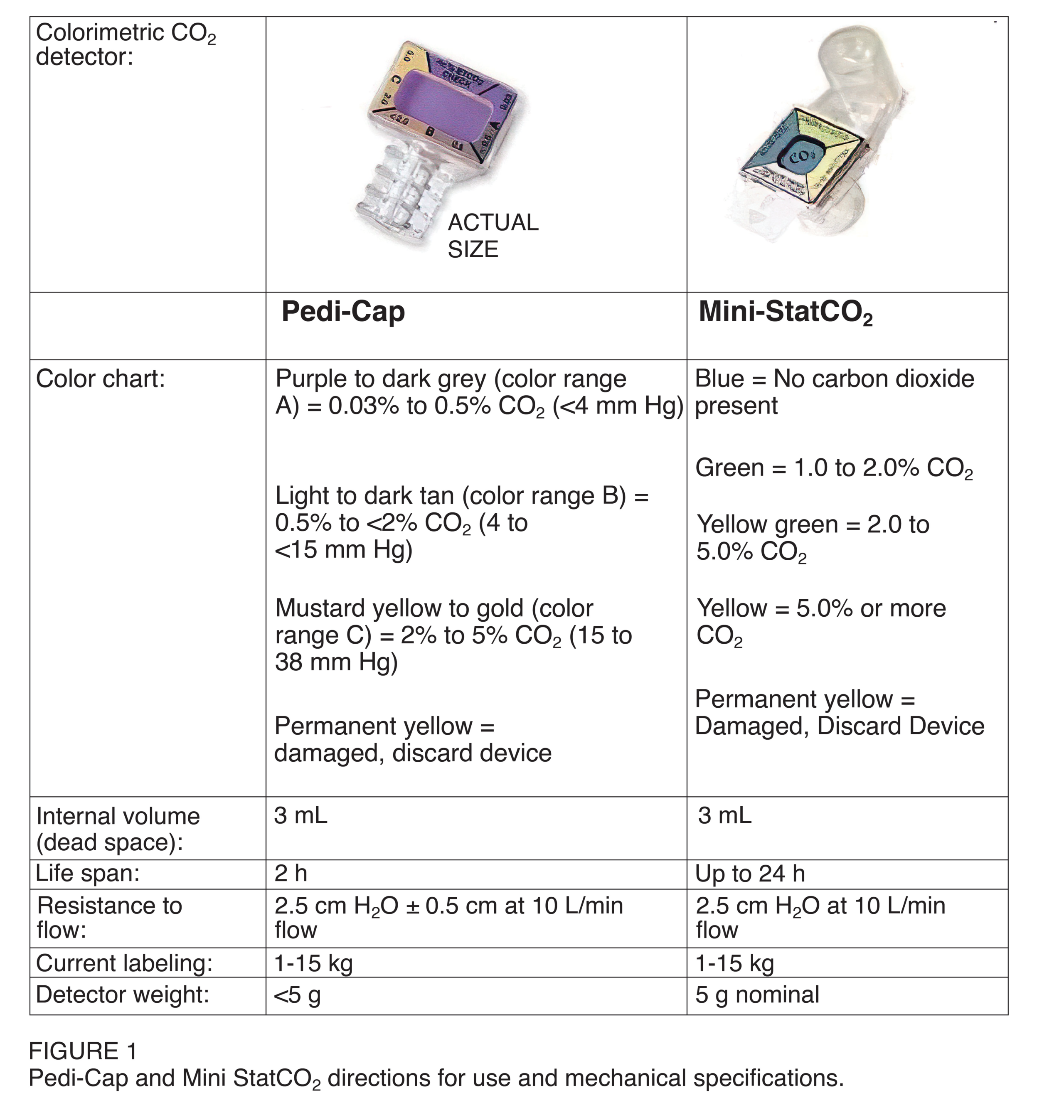
Calorimetric CO2 detectors.14
When administering PPV after endotracheal intubation, the PPV device must provide a PEEP of at least 5 cm H2O. PEEP helps keeps the alveoli from collapsing during expiration and makes it easier to inflate them safely on inspiration. A T-piece resuscitator or a flow-inflating bag is usually the best choice for preterm infant resuscitations. It is challenging to provide consistent PEEP via a face mask with a self-inflating bag. If needed, a self-inflating bag with a PEEP valve can be used to provide PEEP during PPV.
Key Takeaway
INSURE is a mnemonic for early surfactant therapy for preterm infants who do not improve with CPAP:
INtubate-SURfactant-Extubate.
If the preterm infant has severe respiratory distress syndrome and requires intubation, surfactant replacement therapy can be administered through the ET tube. Antenatal steroids, early CPAP, and intubation followed by prophylactic surfactant lower the risk of severe respiratory distress in the preterm baby born < 30 weeks gestation.
If the preterm newborn fails to improve after receiving CPAP, intubation and surfactant administration are reasonable next steps. One treatment protocol called INSURE (INtubate-SURfactant-Extubate) involves intubating, administering surfactant, and then immediately extubating the infant and resuming CPAP. If the preterm baby is < 26 weeks gestation, the team may choose to administer prophylactic surfactant immediately rather than attempt CPAP alone.
Titrating Oxygen Concentration
Reperfusion injury poses a risk to preterm babies. The mechanisms that protect their cells from oxygen-associated injuries are underdeveloped. Therefore, oxygen concentration must be carefully adjusted to ensure that the baby achieves the targeted preductal oxygen saturation.
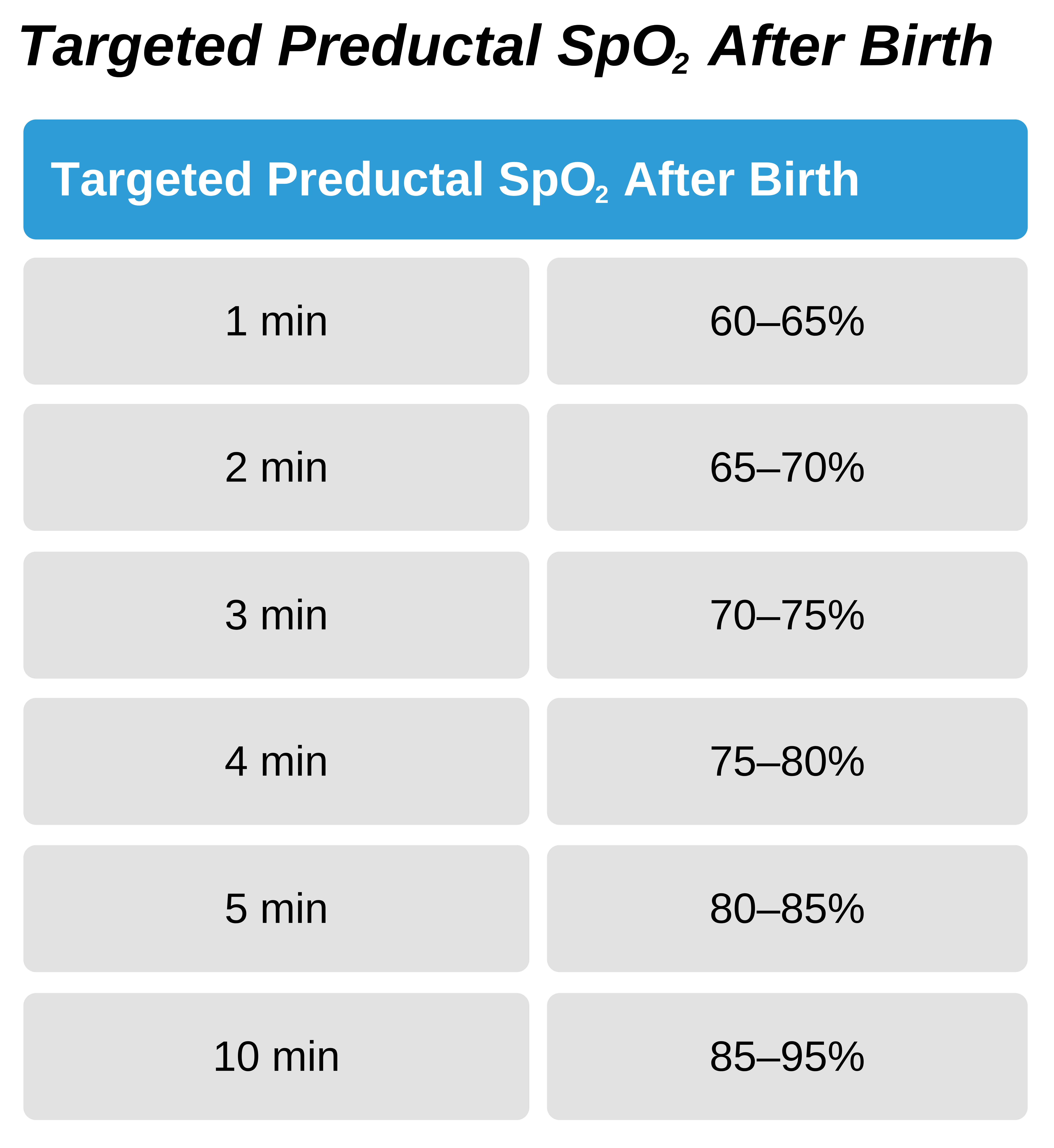
A pulse oximeter and an oxygen blender are necessary to titrate the oxygen concentration for the preterm infant. The oxygen blender should initially be set to a low concentration of 21–30%. In most cases, this percentage of oxygen should adequately increase the baby’s oxygen saturation. If the baby is not reaching the expected SpO2 levels after supplying oxygen, then the oxygen concentration on the blender can be increased.
If the infant develops bradycardia and requires chest compressions, the baby should be intubated and immediately given 100% oxygen.
13 Jain N, James J. Impact of early CPAP on the respiratory care of preterm babies – an audit. J Neonatol. 2017;31(1–2):1–5. https://journals.sagepub.com/doi/abs/10.1177/0973217920170101?journalCode=nnta
14 Garey DM, Ward R, Rich W, Heldt G, Leone T, Finer NN. Tidal volume threshold for colorimetric carbon dioxide detectors available for use in neonates. Pediatrics. 2008;121(6):e1524–1527.