Epinephrine
Epinephrine is a sympathomimetic drug that increases heart rate and the contractile strength by activating the alpha- and beta-adrenergic systems. It also causes systemic vasoconstriction. These modes of action effectively divert blood flow into the myocardium.
Related Video – Epinephrine ACLS Drugs
Indications
Epinephrine is indicated if the baby’s HR remains < 60 bpm after 60 seconds of high-quality chest compressions using 100% oxygen concentration. Epinephrine should not be given if the team has not established effective PPV and or provided high-quality chest compressions during the first 60 seconds of CPR.
Key Takeaway
Epinephrine should ONLY be given to the infant with a persistent heart rate < 60 bpm AFTER 60 seconds of coordinated high-quality chest compressions and effective PPV.
Epinephrine Dosage
Epinephrine is given in a concentration of 1:10,000 or 0.1 mg/mL at a dose of 0.02 mg/kg intravenously (equal to 0.2 mL/kg). The dose range is 0.01–0.03 mg/kg. When administering epinephrine via the endotracheal route, its dosing is 0.1 mg/kg (equal to 1 mL/kg).
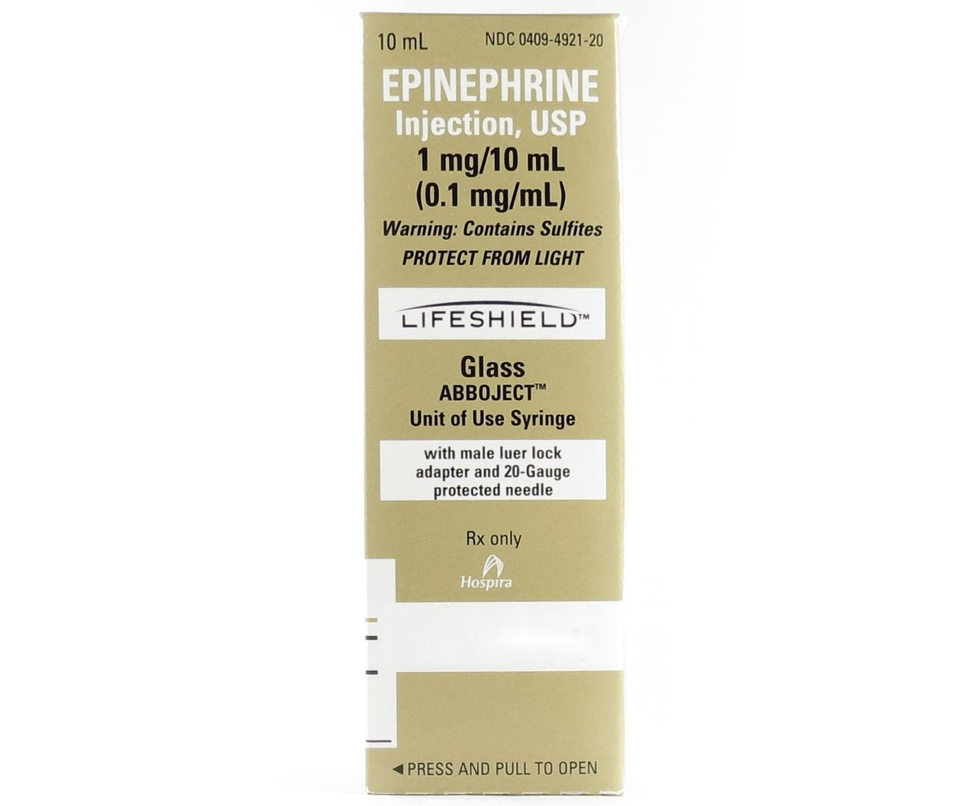
Epinephrine injection.
Epinephrine Route of Administration
Intravenous access is the preferred method for administering epinephrine; intraosseous (IO) administration is the second-best method, leaving endotracheal tube administration as the route of last resort. Epinephrine reaches the central circulation faster and with more reliable absorption through the umbilical vein and IO sites.
Umbilical catheterization is recommended over peripheral venous catheterization because of its more extensive access route and success rates. Also, the peripheral vessels are likely to collapse during arrest, which can cause extravasation of epinephrine, significantly delaying its absorption.
Although the endotracheal route is less effective, some providers may elect to give epinephrine via this route while performing umbilical catheterization.
Administering Epinephrine
A 3-way stopcock is used to deliver the correct dose of epinephrine to the newborn. The 3-way stopcock is connected to the umbilical or IO catheter and flushed with normal saline to push out all the air from the catheter and the ports of the stopcock.

3-way stopcock.
After placing the stopcock and flushing the catheter with normal saline, the clinician administering epinephrine:
- Inserts the epinephrine IV syringe on the parallel port and places a 1 mL syringe on the 90-degree flushing port
- Turns the stopcock to block the passage of fluid to the patient
- Draws the desired calculated volume into the 1 mL syringe
- Turns the stopcock to block the passage of fluid to the epinephrine syringe
- Injects the medication from the 1 mL syringe to the patient; the 1 mL syringe can be removed and replaced with a syringe containing normal saline.
- Flushes the epinephrine to the patient with 3 mL normal saline
- Replaces the normal saline syringe with the 1 mL syringe and draws out the desired volume in preparation for the next possible dose of epinephrine
Assessing the Effectiveness of Epinephrine
The baby’s heart rate is reassessed 1 minute after giving epinephrine. Chest compressions and PPV are halted briefly so the ECG monitor can record an accurate heart rate. If the heart rate is 60 bpm or higher, the team stops chest compressions and continues PPV, titrating oxygen concentration to the predicted preductal oxygen saturation.
If the heart rate still fails to reach 60 bpm, repeat doses of epinephrine can be given every 3–5 minutes. Subsequent doses can be increased. The team also considers other possible contributory problems such as low blood volume or pneumothorax. The team thinks through the MR.SOPA mnemonic to be certain they are delivering effective PPV and verify that they are delivering high-quality chest compressions.