Respiratory System
Maintaining the child’s airway, providing oxygenation, and supporting ventilation are the most critical interventions during the immediate post-arrest period. Continuous monitoring of oxygen saturation and end-tidal CO2 gives the provider an idea of the patient’s oxygenation and ventilation status.
Key Takeaway
Post-cardiac arrest, the most important interventions are:
Airway
Oxygen
Ventilation
Respiratory Assessment
During post-cardiac arrest care, the provider may opt to perform endotracheal intubation and initiate mechanical ventilation. Cuffed endotracheal tubes are preferred when possible. Intubation and mechanical intubation support airway, oxygenation, and ventilation needs while the patient is undergoing other ancillary tests. Waveform capnography and chest X-ray ensure the endotracheal tube is in the correct position.
Continuous assessment and adjustments to interventions and therapy are necessary. Monitoring of oxygen saturation, heart rate, and ECG rhythm via a cardiac monitor is ideal. If the patient is intubated, end-tidal CO2 should be monitored with waveform capnography.
Repeated examination of the child’s respiratory condition involves observing for bilateral and equal chest rise, auscultating for breath sounds, and watching for signs of respiratory distress or failure such as tachypnea, increased work of breathing, agitation, and altered mental status.
ABG analysis assists in evaluating ventilation. PaCO2 values from the ABG can be compared with the end-tidal CO2. A chest X-ray can help in diagnosing other respiratory problems such as pneumothorax or aspiration pneumonia.
Goals of Respiratory Management in the Post-Cardiac Arrest Period
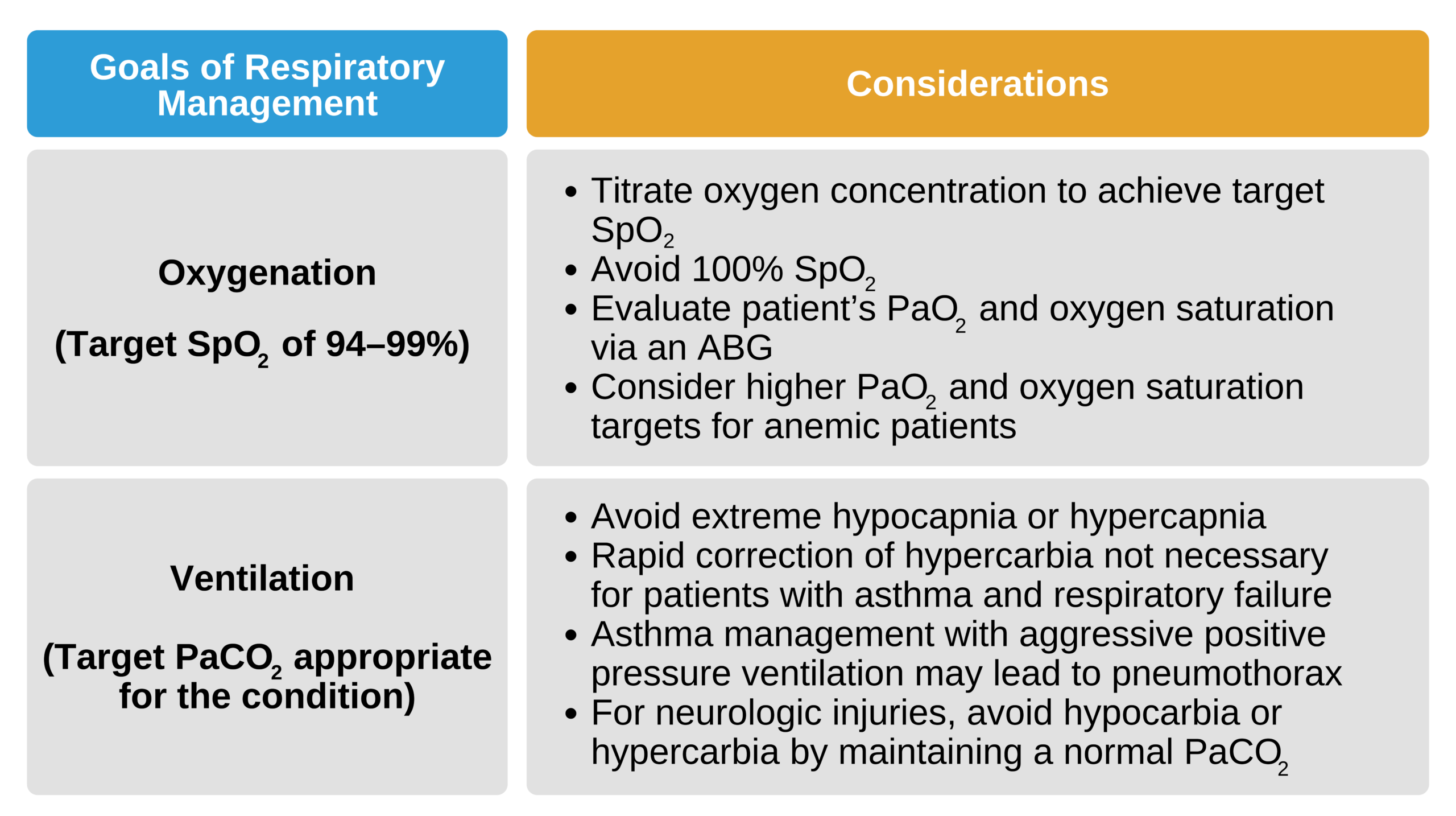
Goals of respiratory management in the post-cardiac arrest period.

Intubated Critically Ill Child
Respiratory Management
In the immediate post-arrest period, supplemental oxygen via a nonrebreather mask should be provided if the child is not intubated. The post-arrest SpO2 goal is 94–99%. When a child is receiving 100% oxygen supplementation, but the SpO2 remains < 90%, an advanced airway with mechanical ventilation and positive end-expiratory pressure should be considered.
Children with cyanotic congenital heart disease should have supplementary oxygen titrated to their baseline SpO2.
Ventilation efforts should target a normal PaCO2 of 35–45 mm Hg. Hyperventilation should be avoided in patients with neurologic dysfunction unless there is strong evidence of impending uncal herniation.
Key Takeaway
Intubation, oxygenation, and ventilation are the most effective interventions for a child in respiratory failure.
In the event of respiratory failure, an advanced airway will likely be required to maintain a airway patency and provide adequate oxygenation and ventilation. Endotracheal intubation should be considered, especially if the child has a depressed mental status. CPAP or noninvasive ventilation may suffice in some patients.
Key Takeaway
An intubated child who continues to deteriorate should be evaluated using the DOPE mnemonic.
If the patient continues to deteriorate despite intubation, the DOPE mnemonic assists the clinician with troubleshooting potential issues with the ET tube:
- Displaced
- Obstructed
- Pneumothorax
- Equipment failure (such as mechanical ventilator)
Related Video: D.O.P.E. for Intubated Patients
Analgesia and sedation minimize the patient’s stress and anxiety levels and lessen the burden of oxygen demand. Recommended analgesics include fentanyl or morphine. Lorazepam or midazolam can be used to control anxiety.
Neuromuscular blockade can assist when inserting the ET tube. The clinician should also consider neuromuscular blockade if the intubated patient requires high peak inspiratory pressures or a high mean airway pressure during mechanical ventilation secondary to reduced lung compliance. It can help with ventilator asynchrony in sedated patients who still have increased airway resistance due to tense muscles of respiration.
Neuromuscular blockade can mask the occurrence of seizures or any signs of agitation elicited by poor oxygenation and ventilation. The child must always be well sedated before administering neuromuscular blockers. The paralyzed patient must be closely monitored for signs of stress that indicate insufficient sedation, such as tachycardia, hypertension, pupil dilation, and tears.