Understanding the Tachycardia with a Pulse Algorithm
Understanding the Tachycardia with a Pulse Algorithm
Initial Steps
When pediatric patients present with a tachyarrhythmia, the provider must first determine if the patient is symptomatic or asymptomatic. The provider should look for signs and symptoms of hypotension, altered sensorium, shock, and life-threatening hemodynamic instability. When present, the provider must support the patient’s ABCs and provide oxygen.
The provider attaches a cardiac monitor or defibrillator. A pulse oximeter is used to determine the oxygen saturation. The team should quickly establish vascular access for medications. While inserting an IV catheter, they should obtain blood samples for laboratory analysis of potassium, glucose, ionized calcium, magnesium, and blood gases.
A 12-lead ECG can help the team accurately diagnose the patient’s condition and guides treatment. The provider must be ready to give medications to treat the specific rhythm disturbance.
Emergency Interventions
The team can attempt some emergency interventions in a pediatric patient who has symptomatic tachyarrhythmia with a pulse. These include vagal maneuvers, cardioversion, and medication therapies.
Vagal maneuvers stimulate the vagus nerve and cause a decrease in heart rate. Vagal stimulation slows down the conduction of impulses through the AV node. Its success depends on the age of the child and their level of cooperation during the maneuver. Placing an ice pack on a child’s face can stimulate the vagus nerve. A small plastic bag can be filled with ice and water and applied over the patient’s eyes for 15 to 20 seconds, being careful not to cover the nose.
When a child is old enough to follow instructions and is willing to cooperate, they can perform the Valsalva maneuver by blowing air from the mouth through a narrow straw or attempting to breath out of the nose while plugging it (as pictured below). Carotid massage is appropriate for older children.

A Valsalva Maneuver
While performing a vagal maneuver, care should be taken to support the child’s ABCs. The patient’s ECG rhythm should be observed before and after the procedure. If the rhythm does not convert after performing these maneuvers and the child remains stable, they may be repeated. If the child is unstable, vagal maneuvers may continue while preparations for medication delivery and cardioversion are underway. Medications and electrical cardioversion are definitive treatments.
Synchronized cardioversion is indicated if the child in SVT or VT with a pulse is symptomatic and hemodynamically unstable. Cardioversion is a painful process, and sedation should be used when time permits, but the procedure should not be delayed.
Key Takeaway
Steps for Synchronized Cardioversion
- Turn on the defibrillator.
- Set lead switch to pad or paddles depending on the equipment used.
- Select the largest adhesive pad or paddles available, ensuring they do not overlap.
- Apply a conductive gel if using paddles on the metal side.
- Sedate the patient as necessary.
- Push the selector switch to synchronized mode.
- Look at the screen for R wave markers, indicating that the defibrillator is in the synchronized mode.
- Select the energy dose based on the patient’s weight.
- Announce “charging defibrillator,” and then push the charging button. Apply the paddles or pads as indicated.
- When the defibrillator is fully charged, announce, “I am going to shock on 3,” and count “1, 2, 3. All clear!”
- After confirming that everyone is clear of the patient, deliver the shock and hold the paddles in place a little longer to ensure the shock is adequately delivered.
- Check the cardiac monitor. If tachycardia is still present, prepare for another shock.
- Reset the sync mode and increase the energy dose.
Synchronized cardioversion times the delivery of the shock with the R wave. Synchrony is important to avoid shocking during vulnerable T waves as there is a chance that SVT and VT will degrade into ventricular fibrillation.
It takes time to synchronize the shock delivery to the R wave, so the provider holds the paddles in place for a longer time to ensure that the shock is delivered appropriately.
When cardioverting SVT or VT with a pulse, use 0.5–1.0 J/kg for the initial dose. If the initial dose fails to convert the patient, then the dose is increased to 2.0 J/kg.
Succeeding shocks can be increased more incrementally by an experienced provider. If the patient’s rhythm is not improving, the provider must reevaluate the patient and verify that the child is not in sinus tachycardia.
If VF develops, the provider must immediately begin high-quality CPR and prepare to deliver an unsynchronized shock as soon as possible.
Related Video – Synchronized Cardioversion for Tachycardia
Medication therapy is an important component of treating tachyarrhythmias in children. The PALS provider must be familiar with medications to treat tachyarrhythmias in the pediatric population:
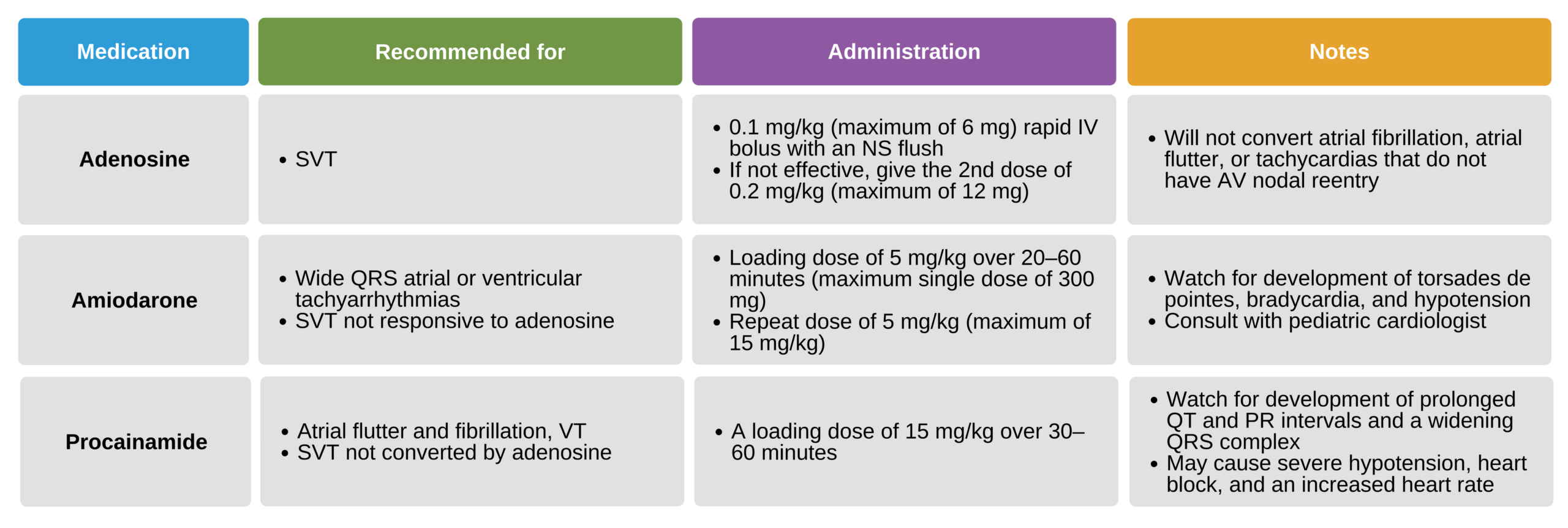
Medications to treat tachyarrhythmias in the pediatric population.