Management of Shock After ROSC
Management of Shock After ROSC
Short Description
The pediatric patient in cardiac arrest may be affected by shock after the return of spontaneous circulation. This algorithm outlines the steps to guide the provider to efficiently assess and manage a child in shock after ROSC.
Related Video – ROSC Achieved – Now What?
Algorithm at a Glance
- Optimize oxygenation and ventilation
- Treat persistent shock
- Evaluate Hs and Ts as a contributing factor
- Treat hypotension
Goals for Management
The clinician will be able to:
- Identify shock following ROSC after cardiac arrest in the child
- Understand and treat shock quickly to prevent the child’s deterioration
The Management of Shock After ROSC Algorithm
This algorithm outlines the steps for assessing and managing children presenting with shock after the return of spontaneous circulation.
Shock Management After ROSC Pediatric Algorithm
Related Video – Understanding Management of Shock After ROSC Pediatric Algorithm
Box 1: Optimize Oxygenation and Ventilation
The team titrates oxygen to maintain an oxyhemoglobin saturation of 94–99%. The clinician begins to wean the supplemental oxygen if the saturation is 100%. If necessary, the clinician considers an advanced airway and uses waveform capnography if available. Respiratory status is continually monitored to limit exposure to hypercapnia or hypocapnia.

Clinicians continually monitor respiratory status after return of spontaneous circulation.
Box 2: Assess For and Treat Persistent Shock
The clinician considers fluid boluses of 10–20 mL/kg of an isotonic crystalloid. The team uses caution and lowers the amount of fluid if poor cardiac function is suspected.
The provider considers the need for inotropic or vasopressor support for shock that does not respond to fluids.
Related Video – One Quick Question: What is the 421 Formula?
Related Video – Types of Shock
Normal saline (0.9% sodium chloride) is an example of an isotonic crystalloid.
Box 3: Consider the Hs and Ts as Contributing Factors
During the process, the clinician continuously evaluates the Hs and Ts as possible contributing factors and corrects them if possible.
Related Video – Introduction to the Hs and Ts
Shock can be due to metabolic abnormalities, hypovolemia, or cardiac tamponade. The provider considers these as possible contributing factors of shock.
- If the clinician determines the shock is hypotensive, they proceed to Box 4.
- If the clinician determines the shock is normotensive, they proceed to Box 5.
Box 4: Hypotensive Shock
If hypotensive shock is apparent, even after IV bolus fluid therapies, the provider gives IV epinephrine (0.03–0.2 mcg/kg/minute) or norepinephrine (0.03–0.5 mcg/kg/min).
Box 5: Normotensive Shock
If the child has persistent shock with a normal blood pressure after IV bolus therapy, the clinician treats the child with low-dose epinephrine or milrinone. Milrinone can produce severe hypotension, so it is administered in a critical care unit by experienced personnel.
Box 6: Other Care
Cardiac arrest takes its toll on multiple organ systems, and after successful resuscitation, the clinician addresses these effects.
The treatment includes:
- Treatment of agitation and seizures
- Treatment of hypoglycemia
- Obtaining ABGs, electrolytes, and calcium
- Initiation of targeted temperature management if the child is comatose
- Aggressive treatment of fever
- Expert consultation and transfer as necessary
Maintenance Fluid After ROSC
Fluid therapy is the administration of an isotonic crystalloid solution given as an IV bolus at a volume of 10–20 mL/kg. Excessive fluid administration can worsen heart failure. A smaller dose (5–10 mL/kg) may be given over 10–20 minutes when there is a concern for adequate cardiac function. Evidence of heart failure includes hepatomegaly, pulmonary edema, jugular vein distention, and an enlarged heart on X-ray.
Although fluid therapy to treat shock is composed of a mainly isotonic crystalloid solution such as 0.9% NaCl or lactated Ringer solution, specific components, such as dextrose solution for hypoglycemia or potassium chloride for hypokalemia, may be added to correct metabolic deficiencies.
The 4-2-1 method estimates the hourly maintenance fluid requirements for children and simplifies the calculation of the proper volume for fluid therapy.
The 4-2-1 Method for Calculating Hourly Fluid Maintenance Requirements
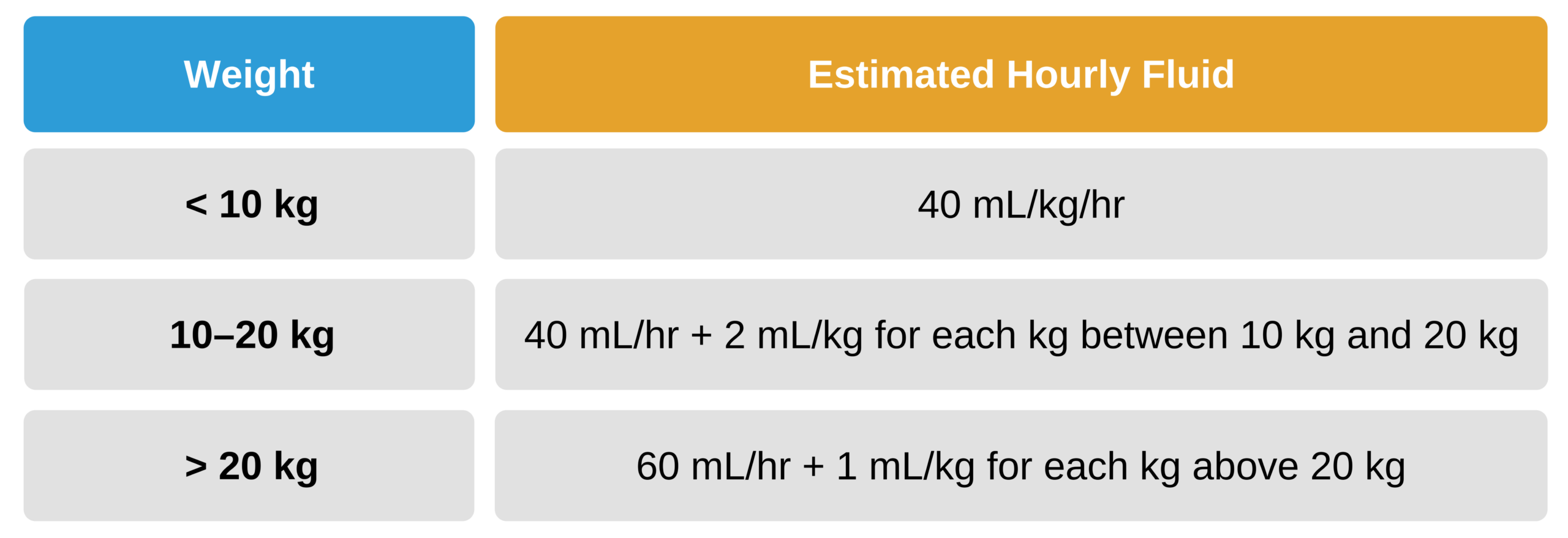
The 4-2-1 method for calculating hourly fluid maintenance requirements.
The infusion rate should be adjusted based on the child’s clinical condition. The patient’s pulse, blood pressure, systemic perfusion, urine output, and level of hydration should be monitored during the infusion.