ACLS Case: Cardiac Arrest
Treating patients with cardiac arrest rhythms requires competency in BLS, ACLS, and post-cardiac arrest care. It is important to note that the fundamental principles for a successful resuscitation are high-quality CPR and rapid defibrillation of shockable rhythms. Appropriate reasons for brief pauses in high-quality CPR include rhythm checks, defibrillation, pulse checks, or placing an advanced airway.
There are four cardiac arrest rhythms: ventricular fibrillation (VF), pulseless ventricular tachycardia (pVT), pulseless electrical activity (PEA), and asystole.
VF occurs when the ventricles depolarize and repolarize in a completely disorganized fashion, causing all pumping efforts and ventricular function to fail.
In pVT, there is an organized electrical activity of the myocardium that is ventricular in origin, as evidenced on ECG by wide QRS complexes, and this does not generate significant blood flow.
In PEA, the electrical activity of the heart may form a normal ECG tracing. However, the cardiac muscle does not generate an adequate response, causing its mechanical function to fail.
Key Takeaway
The rhythms associated with cardiac arrest are:
- VF
- pVT
- PEA
- Asystole
Hypoxia is one of the leading causes of PEA. It can also result from significant blood loss, in which the ejection of blood is inadequate to generate a pulse.
Related Video: ECG Rhythm Review – Asystole
Related Video: What is PEA?
Healthcare staff trained in ACLS must also be able to diagnose and treat the reversible causes of cardiac arrest. The Hs and Ts is a mnemonic used as a guide to identifying the possible causes of cardiac arrest.
Related Video: Introduction to the Hs and Ts
Post-cardiac arrest care begins once the patient achieves the return of spontaneous circulation (ROSC). The prompt initiation of post-cardiac arrest care avoids re-arrest. It can also increase the chance of long-term survival and help to restore neurologic health.
Related Video: ROSC Achieved – Now What?
ACLS responders must understand the algorithms associated with cardiac arrest. The first algorithm below is in the traditional linear format with the shockable rhythms (VF and pVT) on the left side and asystole and PEA on the right side. The second algorithm is a circular arrest algorithm. Both are based on five cycles of compressions and ventilations or 2 minutes of continuous CPR.
Adult Cardiac Arrest
Short Description
This algorithm outlines the steps to guide the team to efficiently assess the patient and manage cardiac arrest.
Algorithm at a Glance
- The rescuer immediately recognizes cardiac arrest and begins high-quality CPR.
- The team determines if the cardiac arrest rhythm is shockable (VF or pVT) or nonshockable (PEA and asystole).
- If the rhythm is shockable, the team administers a shock as soon as a defibrillator is available.
- If the rhythm is not shockable, the team administers epinephrine as early as possible and every 3–5 minutes after that.
- High-quality CPR continues if the patient is in cardiac arrest.
- For VF or pVT, the team considers antiarrhythmics if defibrillation is not successful.
Goals for Management
The responder must succeed in the following goals to successfully manage cardiac arrest:
- Recognize the rhythms of cardiac arrest: ventricular fibrillation, ventricular tachycardia, PEA, and asystole
- Recognize the Hs and Ts as possible causes of cardiac arrest
- Appropriately intervene in cardiac arrest depending on the cardiac arrest rhythm
The Adult Cardiac Arrest Algorithm
This algorithm was created to present the steps for assessing and managing patients presenting with cardiac arrest symptoms.
Adult Cardiac Arrest Algorithm
Key Takeaway
ECG Characteristics of Shockable Cardiac Arrest Rhythms
- VF – appears as voltage fluctuations on the ECG strip; amplitude is characterized as coarse (early VF) or fine (late VF).
- pVT – the patient does not exhibit a pulse; pVT appears as a fast and typically regular rhythm with wide QRS complexes on ECG and no P waves.
ECG Characteristics of Nonshockable Cardiac Arrest Rhythms
- Asystole – complete absence of electrical activity depicted by a flat line on the ECG.
- PEA – exhibits an organized rhythm, but there is no palpable pulse.
Box 0: Ensuring Scene Safety
Particularly for OHCA, it is critical that the rescuer first ensure the scene is safe for both the patient and the team.
Box 1: Identifying Cardiac Arrest and Initiating CPR
Ideally, the team performs rhythm-based management of cardiac arrest. If there is no pulse, the rescuers initiate high-quality CPR. If oxygen and a monitor/defibrillator are available, the team attaches those as CPR continues.
Related Video: One Quick Question: What to Expect During Your First Code?
Box 2: Identifying Shockable Rhythms
If the rhythm is shockable (VF or pVT), the team proceeds to Box 3. If the rhythm is not shockable (asystole or PEA), they proceed to Box 9.
Related Video: ECG Rhythm Review – Ventricular Fibrillation Video
Related Video: ECG Tracing Review – Polymorphic Ventricular Tachycardia (Torsades de Pointes)
Related Video: ECG Rhythm Review – Asystole
Box 3: Administering Shock
When using a manual defibrillator, the first rescuer performs chest compressions while the defibrillator is charging. Once charged, the rescuer stops chest compressions, and the second team member instructs everyone to clear the patient. Once everyone is clear of the patient, the second rescuer delivers a shock at the dosage recommended by the defibrillator manufacturer.
Studies show that biphasic manual defibrillators are preferred over monophasic defibrillators for the treatment of atrial and ventricular arrhythmias.
Biphasic waveform defibrillators set to deliver 200 J or less for the first shock were shown to be efficacious.29
The first dose of shock delivery depends on the manufacturer’s recommended energy dose. If the rescuer does not know the manufacturer’s recommended dose, they should consider the maximal dose for the first and all shocks following.
If VF recurs after a successful shock was delivered, the team should deliver subsequent shocks with the same dose.
When using a monophasic defibrillator, 360 J should be used for the first shock and for recurrent episodes.
Key Takeaway
Energy Dose for Shock
1. First shock – refer to manufacturer’s recommendation or highest dose available (if the recommended shock dose is unknown)
2. Subsequent shocks – refer to manufacturer’s recommendations or escalating energies (higher for second and subsequent shocks)
Note: For monophasic defibrillators, the initial shock dose is a standard 360 J and for subsequent shocks.
Box 4: Continuing High-Quality CPR
The team minimizes CPR interruptions by immediately performing chest compressions after a shock. At this point in the algorithm, it is important to obtain IV or IO (intraosseous) access in anticipation of drug delivery.

Auto-compression devices are tested on a manikin

Clinicians should pay attention to ETCO2 monitoring.
Box 5: Rhythm Check and Shock Administration
After 2 minutes of high-quality CPR, the team rechecks the patient’s rhythm. If there is continued VF or pVT, they prepare to administer another shock. The rhythm check should be as brief as possible and CPR resumed immediately afterward.
Box 6: Epinephrine and Consideration for Advanced Airway
Once the team delivers the shock, they resume high-quality CPR immediately. At this point, two shocks have been delivered, and vascular access is available. High-quality CPR is ongoing.
It is now time to utilize drug therapy to restore a perfusing rhythm. The first-line medication for the treatment of VF or pVT is epinephrine.
A cardiac arrest patient may receive epinephrine when feasible after the placement of vascular access. Studies of IHCA patients show an increased chance for ROSC if epinephrine is given within 1 to 3 minutes of cardiac arrest as opposed to after 3 minutes.30
For OHCA patients, studies show increased rates of ROSC if epinephrine is given 9 minutes or less from the onset of cardiac arrest compared with patients given epinephrine later.31
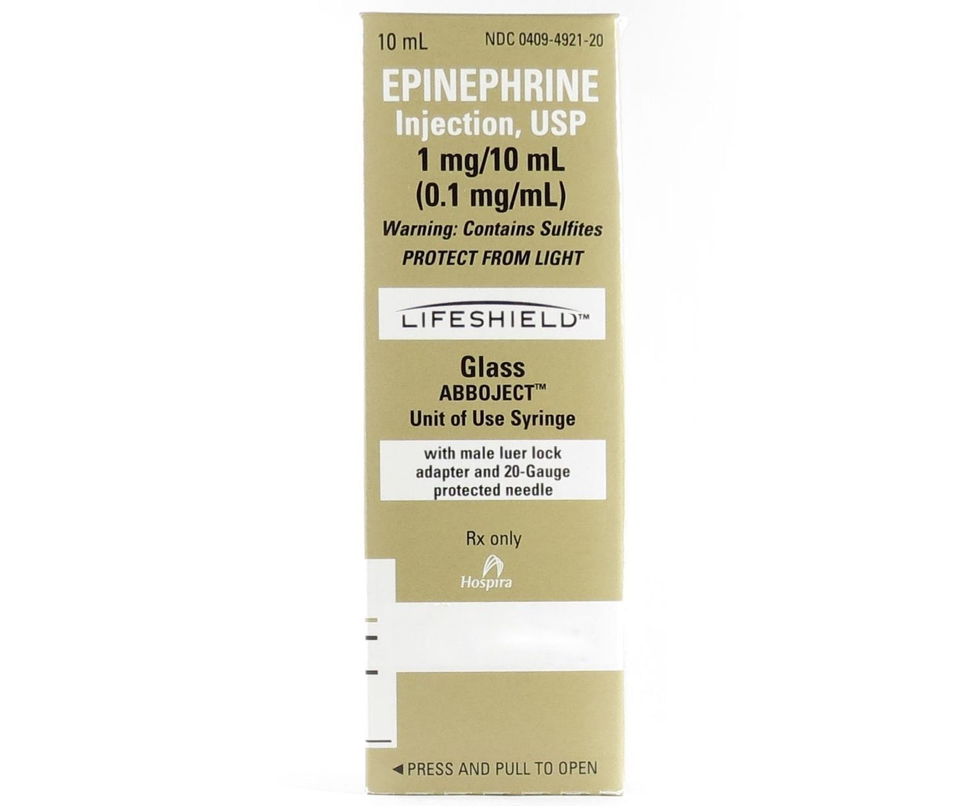
Epinephrine 1:10,000 Box Package Revision
Related Video: Epinephrine – ACLS Drugs
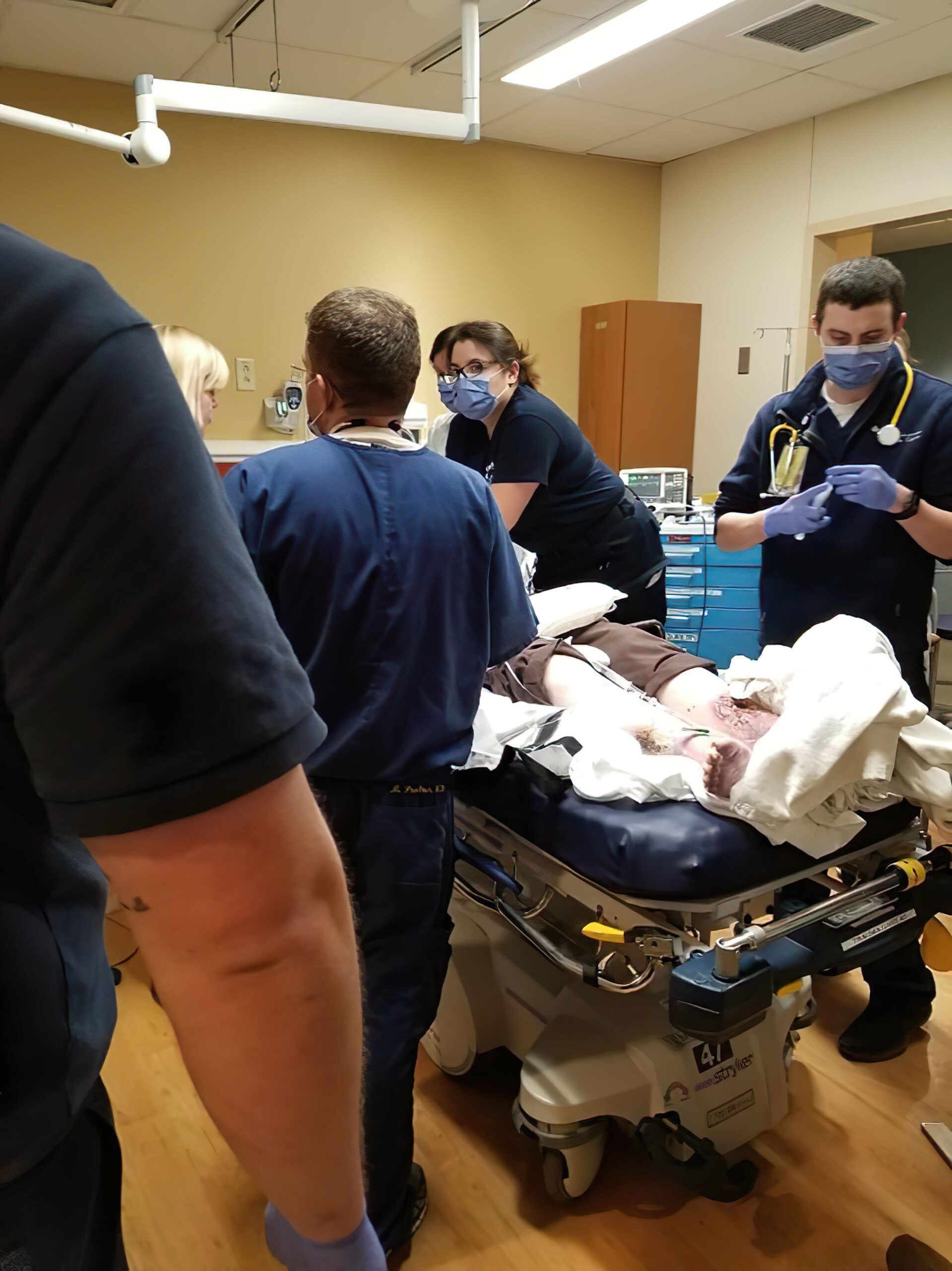
Rescuer on far right is preparing medication.
Administering Epinephrine
The recommendations for treating cardiac arrest are for epinephrine intravenously or via the intraosseous route with a preparation of 1:10,000 dilution, 1 mg every 3 to 5 minutes. Studies show that this standard dose is responsible for improved survival and ROSC.32
The addition of vasopressin does not deliver any advantage over using epinephrine alone. Thus, the AHA no longer recommends vasopressin as a treatment in cardiac arrest.33
Key Takeaway
Recommendations no longer suggest vasopressin as a treatment choice in cardiac arrest.
The effects of epinephrine include:
- Vasoconstriction, which causes increased perfusion to the heart and brain
- Increased cardiac output resulting in:
- Increased heart rate
- Increased heart contractility
- Increased conductivity of impulses through the AV node
Related Video: What is Cardiac Output?
Related Video: What is the Cardiac Output Formula?
Considering Advanced Airway
In Box 6, in addition to administering epinephrine, responders are directed to consider the insertion of an advanced airway. This is not always necessary if the patient is being ventilated adequately using a bag-mask.

A bag mask provides manual ventilation to patients.
Ideally, two rescuers are needed to ventilate effectively with a bag-mask. One obtains a tight seal with the mask over the patient’s mouth and nose. The second rescuer delivers each ventilation at the correct time in the CPR sequence (2 breaths are given after 30 compressions) and at sufficient volume to cause the chest to rise but avoiding excessive ventilation. These are essential components of high-quality CPR.
Related Video: Understanding Bag Valve Mask Usage during CPR
Related Video: Tips for Bagging
When it is determined that an advanced airway is needed, there are several essential points the team must remember:
- Inserting an advanced airway can lead to unacceptable delays in the provision of CPR.
- Only those team members with expertise should attempt insertion of an advanced airway.
- Once inserted, proper placement must be determined by both physical confirmation (equal bilateral chest rise, air entry heard in all lung fields, and no air auscultated over the epigastrium) and physiologic monitoring (waveform capnography).
- The advanced airway is then secured in place, with placement frequently checked to detect any complications, such as dislodgement.
- Once an advanced airway is in place, ventilation and compressions no longer need to be synchronous. The compressor provides continuous chest compressions, while the ventilator provides one breath every 6 seconds.
Note: For more information on advanced airways and ventilation during cardiac arrest, see the chapter on adjuncts.
Box 7: Rhythm Check and Shock Administration
Once the initial dose of epinephrine has been given and 2 minutes have passed since the last shock, the team pauses CPR to perform another rhythm check. If the patient’s rhythm is unchanged or refractory (patient remains in VT or pVT), another shock is administered.
Box 8: Administering Antiarrhythmic and Considering Possible Causes
Once the team administers the shock, they should immediately resume CPR for 2 minutes. Amiodarone is given for VF or pVT refractory to defibrillation, CPR, and vasopressor therapy. Lidocaine is an alternative treatment to replace amiodarone. Both drugs are given IV and IO.
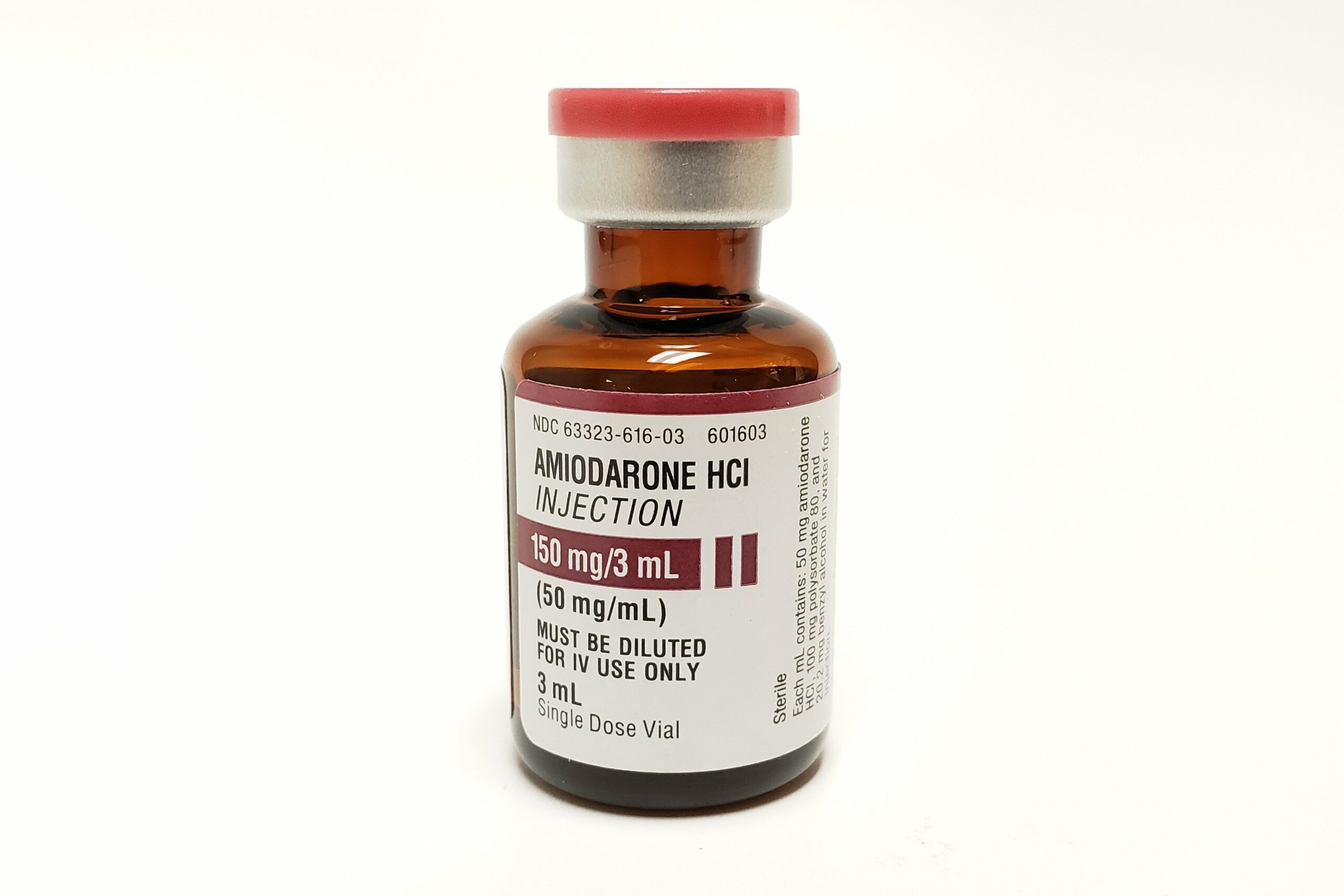
Amiodarone is administered for VF or pVT after defibrillation, CPR, and vasopressor therapy.
Antiarrhythmic Drugs During and Immediately After Cardiac Arrest
Amiodarone is administered for VF or pVT refractory to defibrillation, CPR, and vasopressor therapy. Lidocaine is an alternative treatment for amiodarone. Both drugs may be given intravenously and via the intraosseous route.
Related Video: Amiodarone – ACLS Drugs
Related Video: Lidocaine – ACLS Drugs
Key Takeaway
Preparation of Antiarrhythmic Drugs in Cardiac Arrest
- Amiodarone – First dose 300 mg IV/IO push, then 150 mg IV/IO push for subsequent doses
- Lidocaine – First dose 1.0 to 1.5 mg/kg as IV/IO push, then 0.5–0.75 mg/kg IV push for a maximum of 3 doses or a total of 3 mg/kg
Reversible Conditions
The team leader continues to seek and identify possible reversible causes of arrest, including:
- Hypoxia
- Hypovolemia
- Hydrogen ion excess
- Hypo- or hyperkalemia
- Hypothermia
- Tension pneumothorax
- Tamponade, cardiac
- Toxins
- Thrombosis, coronary
- Thrombosis, pulmonary
Related Video: ACLS – Introduction to the Hs and Ts
Box 9: Is Rhythm Asystole or PEA?
Asystole and PEA are the two cardiac arrest rhythms that are not shockable. As soon as one of these rhythms is identified, the team administers epinephrine.
Box 10: CPR Resumes for 2 minutes
The team administers epinephrine every 3–5 minutes.
At this point, the team leader considers an advanced airway and waveform capnography. After 2 minutes of high-quality CPR, the team stops briefly for a rhythm check.
Box 11: High-Quality CPR Continues If the Rhythm Is Not Shockable
The team leader assesses for treatable causes of cardiac arrest. If the rhythm is shockable at any time, the team proceeds to Box 5 or 7.
Box 12: ROSC?
If there are no signs of ROSC, the team returns to Box 10 or 11. If there are signs of ROSC, they proceed to the Post-Cardiac Arrest Care algorithm.
Prognostication During CPR: End-Tidal CO2
The end-tidal carbon dioxide (ETCO2) level is used as a prognostication tool in considering when to end resuscitative efforts in intubated patients. Failure to attain an ETCO2 > 10 mm Hg via waveform capnography after 20 minutes of CPR portends a poor prognosis. The team should not use ETCO2 for prognostication in the nonintubated patient.
During cardiac arrest, ETCO2 levels reflect cardiac output generated by chest compressions. Hence, lower values indicate poor chest compression quality or low cardiac output. Low ETCO2 values may also indicate bronchospasm, kinking of the ET tube, or mucus plugging of the ET tube.34
Extracorporeal CPR
ECPR is a clinical intervention that utilizes venoatrial extracorporeal membrane oxygenation during cardiac arrest. It is not a recommended treatment for cardiac arrest, but the clinician should consider ECPR in hospital settings where the procedure can be performed immediately. ECPR may also be considered for select patients in cardiac arrest when the suspected etiology may be reversible.
Interventions Not Recommended During Cardiac Arrest
Key Takeaway
Medications NOT recommended in cardiac arrest: </span
- Atropine
- Sodium bicarbonate
- Calcium
- Fibrinolytics
Atropine
Studies report no therapeutic benefit of atropine for routine use in cardiac arrest patients with PEA or asystole.35
Sodium Bicarbonate
The AHA no longer recommends sodium bicarbonate for patients in cardiac arrest. High-quality CPR provides ventilation and perfusion to the surrounding tissues to restore the acid-base balance.
During cardiac arrest, tissue acidosis ensues because of anaerobic metabolism. Thus, the administration of sodium bicarbonate aims to return the physiologic pH.
However, studies have shown that sodium bicarbonate does not improve survival rates. Additionally, it causes adverse effects when used during CPR, such as compromising cerebral perfusion pressure by reducing systemic vascular resistance.36
Related Video: Understanding and Interpreting ABGs Part 3: Acid-Base Introduction
Calcium
Current recommendations do not include routine use of calcium in IHCA and OHCA. Studies fail to show treatment with calcium to be associated with ROSC or improved survival.37
Fibrinolysis
Fibrinolytic therapy is not routinely used in cardiac arrest. Current recommendations include fibrinolytic therapy for patients with acute coronary syndrome or pulmonary embolism. Some studies show promising results when treating patients with cardiac arrest unresponsive to standard therapy38 or with suspected pulmonary embolism as the cause.39 However, clinical trials have consistently failed to show good outcomes with the routine use of fibrinolytic therapy during CPR40 and increased bleeding risk.41
Cardiac Arrest Circular Care
Short Description
This algorithm presents the Cardiac Arrest Algorithm in a circular format to reinforce that cardiac arrest care does not end until ROSC occurs and Post-Cardiac Arrest Care begins.
Algorithm at a Glance
- The circular cardiac arrest care algorithm provides a simple way to understand cardiac arrest care as a continuous process.
- The team understands that cardiac arrest care involves high-quality CPR, medications, defibrillation, and airway management.
- The team ensures that post-cardiac arrest care begins at the time of ROSC.
Goals for Cardiac Arrest Circular Care
The team will recognize that cardiac arrest care is an iterative process that includes:
- Continuous CPR
- Continuous monitoring
- Defibrillation as early as possible
- Drug therapy
- Airway management
- Post-Cardiac Arrest Care
Related Video: ACLS – Cardiac Arrest Circular Algorithm
The Adult Cardiac Arrest Circular Algorithm
This algorithm was created to present the care for a patient in cardiac arrest as a circular algorithm to emphasize the need for ongoing assessment and management.
Adult Cardiac Arrest Circular Algorithm
Step 1: Initiating CPR
When a cardiac arrest is suspected, the team begins high-quality CPR, administers oxygen, and attaches a monitor/defibrillator.

CPR procedure in the hospital.
Step 2: Interpreting the Rhythm
If VF or pVT, the team defibrillates immediately. If PEA or asystole, the team continues CPR and administers epinephrine early in the process and every 3 to 5 minutes throughout the resuscitation.
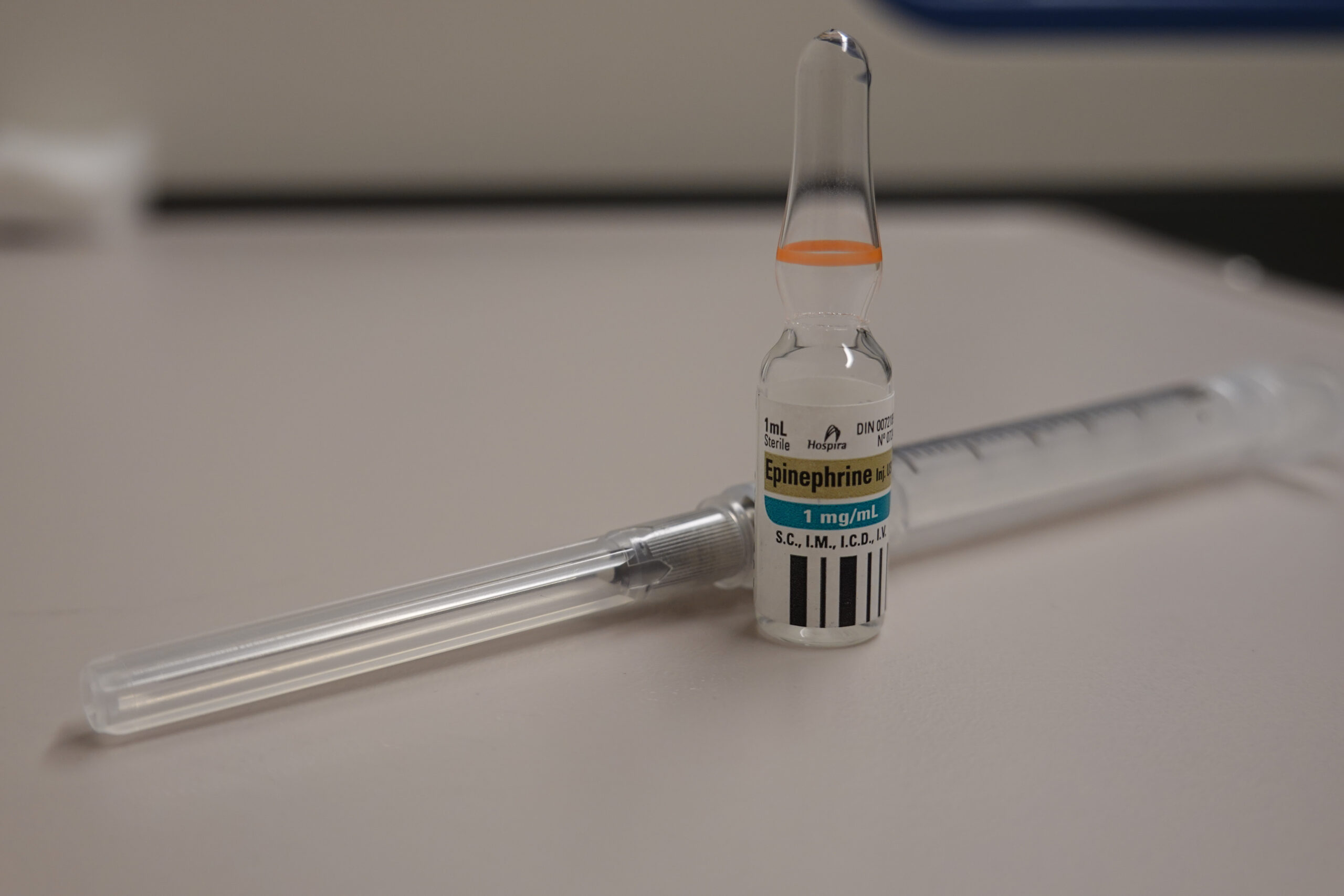
Epinephrine is administered every 3 to 5 minutes.
Related Video: Epinephrine – Cardiac Arrest
Step 3: Step 2 Is Repeated After 2 Minutes
The team leader considers an advanced airway and assesses for and treats a reversible cause. The team considers the Hs and Ts to evaluate reversible causes.
Related Video: Introduction to the Hs and Ts
Step 4: The Cycle Is Continued Until ROSC
Upon return of spontaneous circulation (ROSC), the team proceeds to the Post-Cardiac Arrest Care algorithm.
Terminating Resuscitation Efforts
As important as it is to know how to resuscitate a patient, it is equally important to know when to terminate resuscitation efforts. Unfortunately, the answer to this question is not always clear-cut.
Before terminating resuscitation efforts, the clinician must consider the physical, psychological, social, and ethical aspects of this decision. Some principles that can help guide this determination include:
- Medical futility, or the belief that prolonged resuscitation will not change the outcome. That is, even with resuscitation efforts, the patient is likely to die. This concept is most applicable when dealing with a prehospital arrest in which there was no witness, no prehospital ROSC occurred, or when EMS identified an initial unshockable rhythm. Any of these conditions predict a > 99% chance of inferior outcome or medical futility.42
- Autonomy, or the patient’s right to refuse treatment. “Does the patient have a do not resuscitate (DNR) order, or is the family aware of the patient’s DNR status?”
- Beneficence, or doing what is in the best interest of the patient. “If we attempt prolonged resuscitation for this 95-year-old, is the outcome likely to be something they would have wished for?”
- Benefit versus burden. “If we continue medical treatment, will the benefits for the patient be higher than the burden?”
Ultimately, within the specific institution, there must be guidelines in place to direct EMS and in-hospital personnel about decisions to terminate treatment. The hospital Ethics Committee is often a valuable resource when making these sorts of decisions.
29 Morrison LJ, Henry RM, Ku V, Nolan JP, Morley P, Deakin CD. Single-shock defibrillation success in adult cardiac arrest: a systematic review. Resuscitation. 2013;84(11):1480–1486.
30 Donnino MW, Salciccioli JD, Howell MD, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. BMJ. 2014;348:g3028.
31 Goto Y, Maeda T, Goto YN. Effects of prehospital epinephrine during out-of-hospital cardiac arrest with initial non-shockable rhythm: an observational cohort study. Crit Care. 2013;17(5):R188.
32 Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation. 2011;82(9):1138–1143.
33 Panchal AR, Berg KM, Hirsch KG, et al. 2019 American Heart Association focused update on advanced cardiovascular life support: use of advanced airways, vasopressors, and extracorporeal cardiopulmonary resuscitation during cardiac arrest: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2019;140(24):e881–e894.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000732
34 Kodali BS, Urman RD. Capnography during cardiopulmonary resuscitation: current evidence and future directions. J Emerg Trauma Shock. 2014;7(4):332–340.
35 Neumar RW, Otto CW, Link MS, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 suppl 3):S729–S767.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.110.970988
36 Velissaris D, Karamouzos V, Pierrakos C, Koniari I, Apostolopoulou C, Karanikolas M. Use of sodium bicarbonate in cardiac arrest: current guidelines and literature review. J Clin Med Res. 2016;8(4):277–283.
37 Kette F, Ghuman J, Parr M. Calcium administration during cardiac arrest: a systematic review. Eur J Emerg Med. 2013;20(2):72–78.
38 Hamera JA, Bryant NB, Shievitz MS, Berger DA. Systemic thrombolysis for refractory cardiac arrest due to presumed myocardial infarction. Am J Emerg Med. 2021;40:226.e3–226.e5.
https://www.sciencedirect.com/science/article/abs/pii/S0735675720306471?via%3Dihub
39 Javaudin F, Lascarrou JB, Le Bastard Q, et al. Thrombolysis during resuscitation for out-of-hospital cardiac arrest caused by pulmonary embolism increases 30-day survival: findings from the French national cardiac arrest registry. Chest. 2019;156(6):1167–1175.
40 Bottiger BW, Arntz HR, Chamberlain DA, et al. Thrombolysis during resuscitation for out-of-hospital cardiac arrest. N Engl J Med. 2008;359(25):2651–2662.
41 Wang Y, Wang M, Ni Y, Liang B, Liang Z. Can systemic thrombolysis improve prognosis of cardiac arrest patients during cardiopulmonary resuscitation? A systematic review and meta-analysis. J Emerg Med. 2019;57(4):478–487.
42 Morrison LJ, Verbeek PR, Vermeulen MJ, et al. Derivation and evaluation of a termination of resuscitation clinical prediction rule for advanced life support providers. Resuscitation. 2007;74(2):266–275.