The Acute Coronary Syndrome Algorithm
The Acute Coronary Syndrome Algorithm
This algorithm was created to outline the steps for assessing and managing ACS in patients who present with characteristic symptoms.
Acute Coronary Syndrome Algorithm
Related Whiteboard: Acute Coronary Syndrome – ACS Algorithm
Related Video: Understanding the Acute Coronary Syndrome Algorithm
Box 1: Identifying Chest Discomfort Suggestive of Ischemia
The ACLS responder recognizes signs of ischemia in patients as they present with symptoms. Patients with ACS may report chest discomfort. They may perceive pressure or tightness rather than actual pain.
Other characteristic symptoms include:
- Chest discomfort radiating to the jaw, shoulders, neck, and arms
- Chest discomfort involving the back between the shoulder blades
- Light-headedness, dizziness, fainting, sweating, nausea, or vomiting
- Unexplained dyspnea with or without chest discomfort

One of the characteristic symptoms of ischemia is chest discomfort.
The rescuer should be aware that many groups, including women, patients with diabetes, and older individuals, may not experience the typical signs and symptoms of ischemia.
STEMI Chain of Survival
The STEMI Chain of Survival
The American Heart Association (AHA) describes the ST elevation myocardial infarction (STEMI) chain of survival. This care system considers the stakeholders of ACS management, including the patients, family members, and healthcare personnel.
The links include prompt recognition and reaction to STEMI warning signs, rapid EMS dispatch, prearrival notification, and EMS system transport to the receiving hospital; rapid assessment and diagnosis in the ED or cath lab; and rapid treatment.
Key Takeaway
Initial Prehospital Therapies in ACS
- Oxygen – when dyspneic, hypoxemic, in heart failure
- Aspirin – 162–325 mg tablets chewed; contraindicated in GI bleeding
- Nitrates – contraindicated in inferior wall MI and RV infarction, hypotension with sildenafil
- Opiates – to achieve analgesia and decrease oxygen demand; likely to cause hypotension
- Initial ECG if available

Nitroglycerin is a type of nitrate, one of the initial prehospital therapies in ACS.
Box 2: EMS Care and Prehospital Preparation
EMS personnel monitor the patient’s vital signs and cardiac rhythm to properly assess the patient. They are prepared to initiate CPR and implement defibrillation when necessary. They make sure to support the patient’s airway, breathing, and circulation.
EMS personnel also provide oxygen and administer medications when necessary to stabilize the patient. Supplemental oxygen is titrated to maintain oxygen saturation > 90% to improve arterial oxygen content and support oxygen delivery.
One of the pathological considerations of ACS is thrombus formation. Aspirin therapy is necessary to stabilize patients with ACS. At therapeutic doses of 162–325 mg, aspirin can immediately inhibit thromboxane A2 production. This inhibits the action of platelets, which play a significant role in thrombus formation. Aspirin can also prevent coronary artery reocclusion.
Related Video: Aspirin – ACLS Drugs
Nitroglycerin (NTG) dilates peripheral arteries and veins. This effect reduces the preload of the left and right ventricles, which lessens the burden to the myocardium. NTG also reduces chest discomfort in patients with ACS. A positive response to NTG (i.e., reduction in chest pain) should not be viewed as a diagnostic clue, as other causes of chest pain may also be relieved with the use of nitrates.
NTG must be used with caution in patients with inferior wall and right ventricular MI, and it is contraindicated in patients with hypotension, bradycardia, or tachycardia. The recent use of a phosphodiesterase inhibitor such as sildenafil (Viagra™) potentiates the effects of NTG, which can cause severe hypotension that is refractory to vasopressor treatment and may be fatal.
Catecholamine release may worsen the symptoms of ACS. Opiates such as morphine provide relief from chest pain and anxiety, which may reduce the release of catecholamines. Morphine’s vasodilatory effects reduce left ventricular preload and afterload. Hence, opiates can reduce myocardial oxygen demand and catecholamine release. This also helps to redistribute blood volume in patients with acute pulmonary edema.
Related Video: Morphine – ACLS Drugs
To guide the management of patients with ACS, EMS obtains a 12-lead ECG, which assists in patient triage. EMS will determine whether to prepare the receiving hospital for percutaneous coronary intervention (PCI) or fibrinolytic therapy, either of which reduces morbidity and mortality. This intervention potentially minimizes the extent of myocardial injury.
Should EMS identify STEMI on the 12-lead ECG, the team will promptly notify the receiving hospital. If time permits, the EMS team should also attempt to complete a fibrinolytic checklist before arrival at the hospital.
Box 3: Immediate Emergency Department (ED) Assessment and Treatment
The third link in the STEMI chain of survival is the immediate emergency department (ED) assessment and treatment. Best practice for patients with confirmed STEMI by EMS is to bypass the ED and proceed to the cath lab. For patients with STEMI, the goal is to provide fibrinolytic therapy within at least 30 minutes of ED arrival or perform PCI in a cardiac catheterization lab within at least 90 minutes of first medical contact.
If immediate cath lab is not possible, once the patient arrives at the ED, the team titrates oxygen to maintain an SpO2 > 90%. ED personnel administer aspirin and NTG or morphine for pain.
Once the patient arrives at the ED, the ACS team obtains the 12-lead ECG from EMS, but if this is unavailable, an ECG must be obtained within 10 minutes of arriving at the ED door.
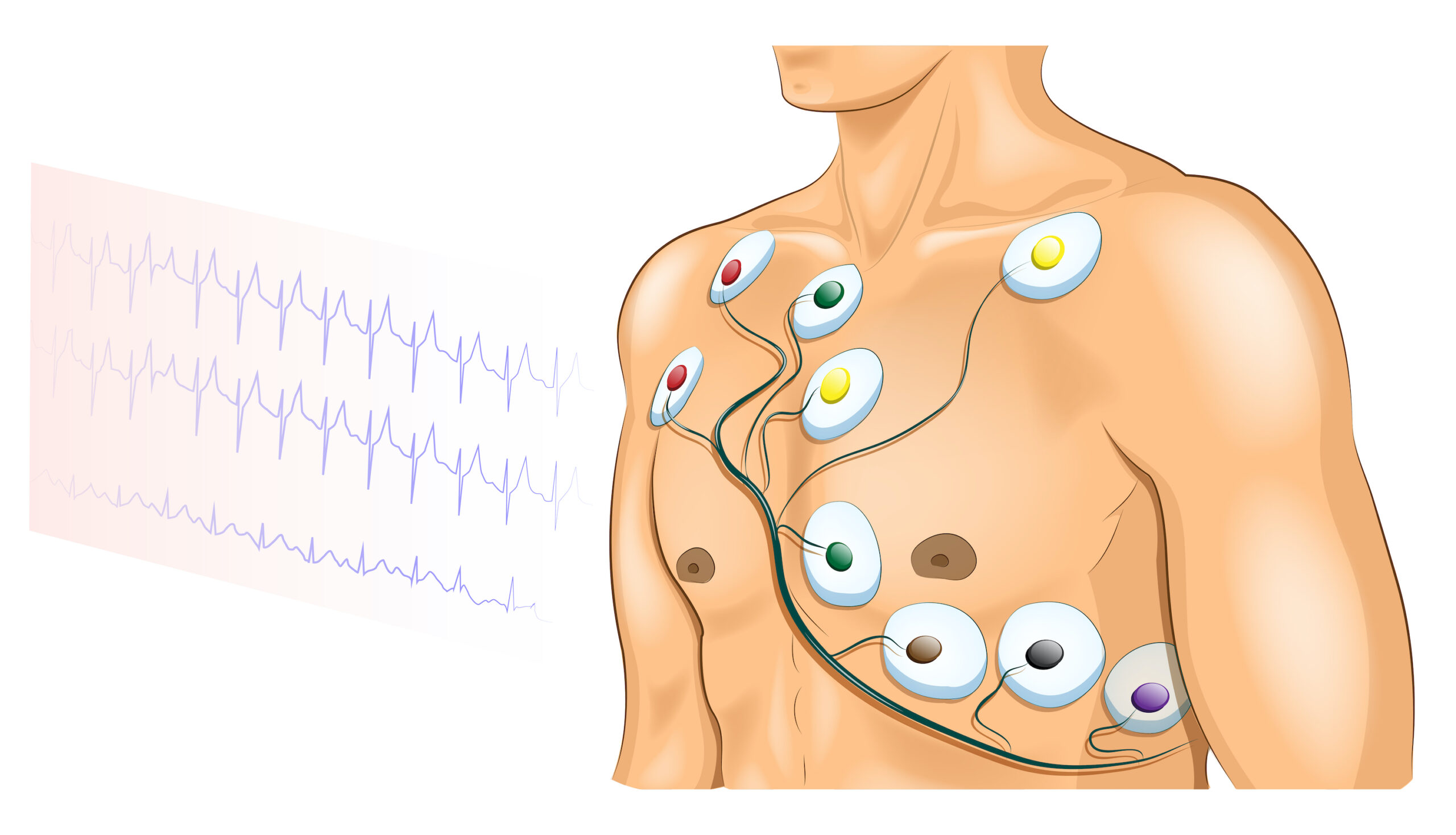
A 12-lead ECG is attached to a patient.
During the first 10 minutes of arriving at the ED, the team monitors the patient’s vital signs and record oxygen saturation. They immediately establish IV access and obtain a blood sample for cardiac marker levels, electrolytes, and coagulation factors. The team completes a short but focused history and physical examination together with the fibrinolytic checklist.
Box 4: Classifying Patients With ACS According to 12-Lead ECG Findings
The team leader evaluates the ECG and classifies the patient with ACS into one of two groups based on the 12-lead ECG: STEMI (team proceeds to Box 5) or non-ST elevation ACS (NSTE-ACS) (team proceeds to Box 9).
Box 5: ST Elevation or New LBBB?
The clinician identifies ST elevation or new left bundle branch block (LBBB) in the STEMI group.
By definition, ST elevation is considered present if there is ≥ 1 mm (0.1 mV) elevation in at least two contiguous leads other than V2 and V3. ST elevation is considered present in V2 and V3 if there is a > 2 mm (0.2 mV) elevation.
Box 6: Considering Adjunctive Therapies
The team ensures that any adjunctive therapies will NOT delay reperfusion.
Box 7: Determining the Onset of Symptoms
The timing will influence whether the patient is a candidate for reperfusion therapy. Patient outcomes are best when they undergo reperfusion therapy ≤ 12 hours from the onset of symptoms.
If the time from symptom onset is ≤ 12 hours, the team proceeds to box 8. If the time is > 12 hours, the team proceeds to box 11.
Box 8: Defining Reperfusion Goals
Percutaneous coronary intervention (PCI) and fibrinolytic therapy are the mainstay treatments for patients with STEMI within 12 hours of symptom onset. These treatments reduce the risk of mortality and morbidity. The goal is a first medical contact-to-balloon time of ≤ 90 minutes. If fibrinolysis is indicated instead of PCI, the goal is a door-to-needle time of ≤ 30 minutes.
Box 9: Non-ST Elevation ACS (NSTE-ACS) Risk Stratification
Patients with NSTE-ACS are classified as high-risk or low-/intermediate-risk ACS using a validated scoring tool such as the Thrombolysis in Myocardial Infarction (TIMI) or Global Registry of Acute Coronary Events (GRACE).
For patients classified as high-risk NSTE-ACS, the team proceeds to box 10. For patients classified as low-/intermediate-risk NSTE-ACS, the team proceeds to box 12.
Box 10: High-Risk NSTE-ACS
The high-risk group may present with ST depression, dynamic T-wave inversion, transient ST elevation, or a high risk score. For these patients, the team proceeds to box 11.
Box 11: Considering an Early Invasive Strategy
The clinician considers invasive therapies for patients who are considered high risk or have elevated troponin levels. High-risk patients have hemodynamic instability, ischemic chest pain, persistent ST deviation, ventricular tachycardia, or heart failure.
The team also considers adjunctive therapies such as heparin or nitroglycerin if indicated.
Box 12: Low-Risk or Intermediate-Risk NSTE-ACS
Patients in the low/intermediate risk group as determined by a risk assessment tool such as TIMI or GRACE may present with a normal ECG or with nondiagnostic changes in the T wave or ST segment. For these patients, the team proceeds to box 13.
Box 13: Considering Admission
For low-risk or intermediate-risk patients, the team leader considers inpatient admission to the appropriate level of care for continued monitoring.