In-Hospital Cardiac Arrest

In-Hospital Cardiac Arrest Scenario.
IHCA: Where Do Hospitals Combat Cardiac Arrest?
In-hospital cardiac arrest continues to be a leading cause of death in the US, with approximately 290,000 events occurring each year.5 However, over the years, the outcomes of in-hospital CPR have improved. Hospitals participating in the AHA’s Get with the Guidelines® resuscitation program demonstrated a 4% per year increase in survival rates from 2000 to 2009.6 In 2016, the overall IHCA rate of survival to discharge had increased to 25% from 17% in 2000.7
Effective improvement strategies enacted by institutions can prevent more cardiac arrests and increase survival rates. According to AHA data, 19% of in-hospital CPR occurred in the unmonitored general wards, compared with 48% in the ICU and 18% in the ED.8
However, there are gaps in maintaining a consistent result in survival rates. Some studies have shown that survival rates are lower if resuscitation is performed at night and over the weekends compared to weekdays.9 Also, a recent European study revealed lower-income patients tended to have lower survival rates after IHCA.10
Prearrest Rapid Response Systems
Recognition of Patients at Risk of Cardiac Arrest
The most common causes of cardiac arrest are respiratory failure and hypovolemic shock. Earlier studies showed that, in the general medical and surgical wards, 1 in 5 patients developed abnormal vital signs, and an astonishing 50% of these patients were unidentifiable before the arrest.11 AHA Get with the Guidelines®-Resuscitation investigators more recently reviewed 7,851 patient records and found that in the 4 hours or less before IHCA, at least one abnormal vital sign was seen in 59.4% of patients. And as the number of abnormal vital signs increased, there was an associated rise in mortality.12
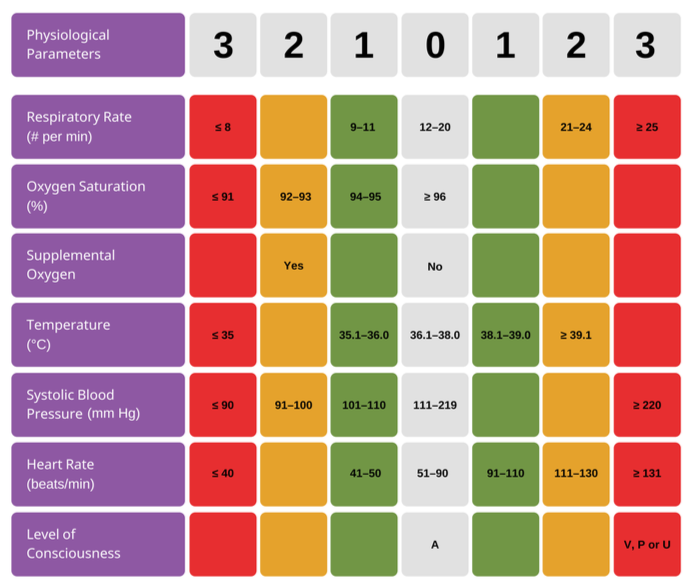
Strategies for the early recognition of deteriorating patient status include implementing continuous electronic monitoring and advanced telemetry for high-risk patients. Another tool to quickly assess critically ill patients is the use of composite risk scores and the development of algorithms that consider multiple parameters such as the National Early Warning Score (NEWS).13
NEWS Trigger System
Early Warning Systems vary across institutions.
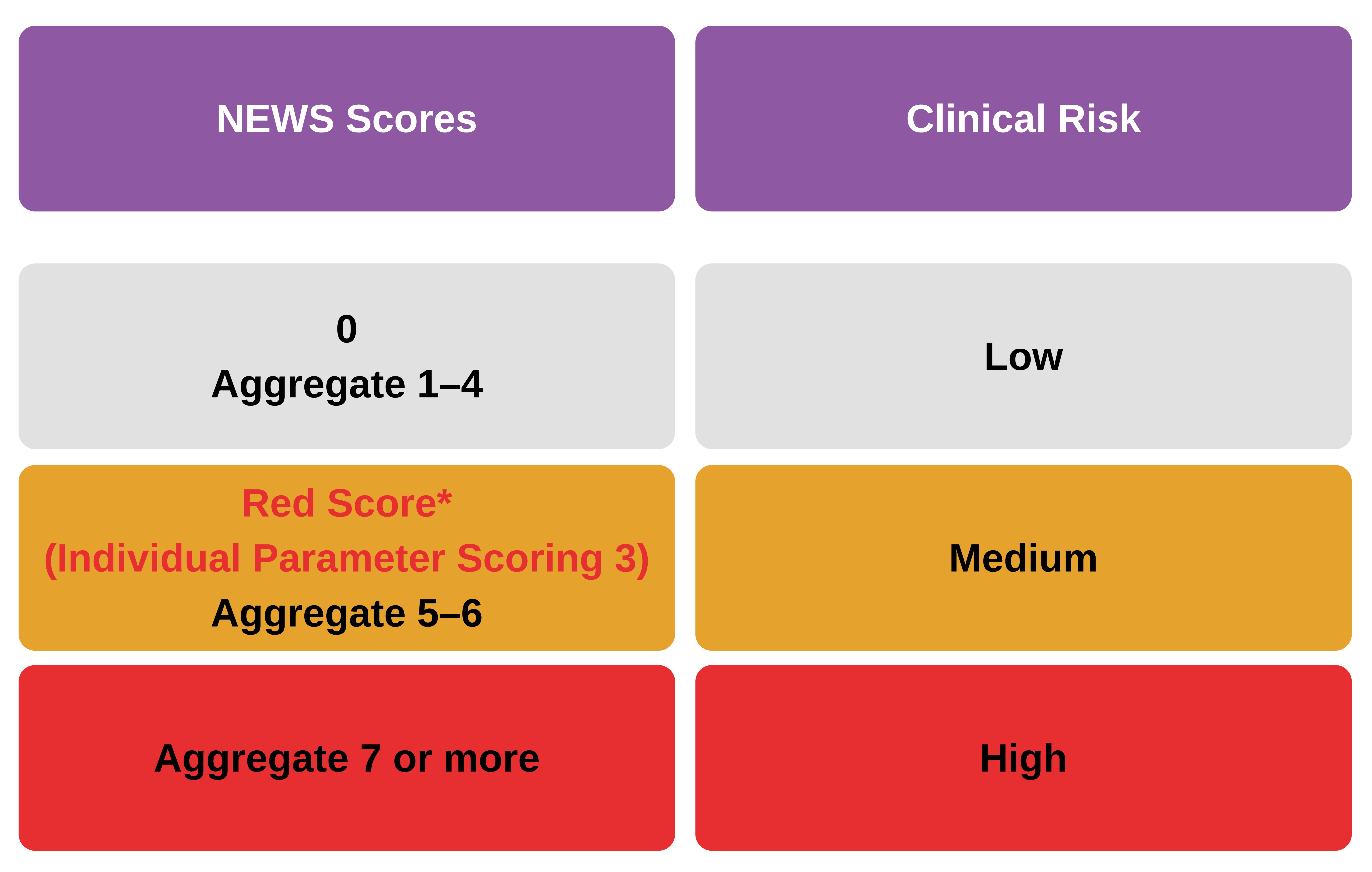
The NEWS trigger system is aligned to the scale of clinical risk.
Key Takeaway
Rapid response teams (RRTs) and medical emergency teams (METs) are available to intervene BEFORE the patient’s condition deteriorates quickly. The goal is to reduce the need for resuscitation and increase positive outcomes. The longer the delay in moving a critical patient to the ICU, the higher the mortality risk.
Crisis Resource Management Principles
Resuscitation teams perform best if each member recognizes the team leader, understands the role assigned to them, performs seamless teamwork, and relays effective communication.
The principles in crisis resource management include:
- The importance of training to be an ACLS team leader.
- Using checklists for leadership activities.
- Standardized communication between team members.
- Performing cross-checks for the safety of team members before defibrillation.