Understanding the PALS Systematic Approach Algorithm
The algorithm has two significant pathways. If a child is unresponsive, immediate interventions should begin as required while following the left side of the algorithm. If the child’s condition is not life-threatening, the systematic approach to additional assessment can be continued, following down the right side of the algorithm.
Initial Impression
Three factors influence the initial impression of an acutely ill child: the child’s appearance,work of breathing, and circulation (ABC– appearance, breathing, circulation).
These three factors are part of the Pediatric Assessment Triangle (PAT). A clinician uses them to perform a rapid assessment of the patient concerning three clinical systems, namely: respiratory, circulatory, and neurologic.
A child with abnormal PAT findings may require quick intervention.
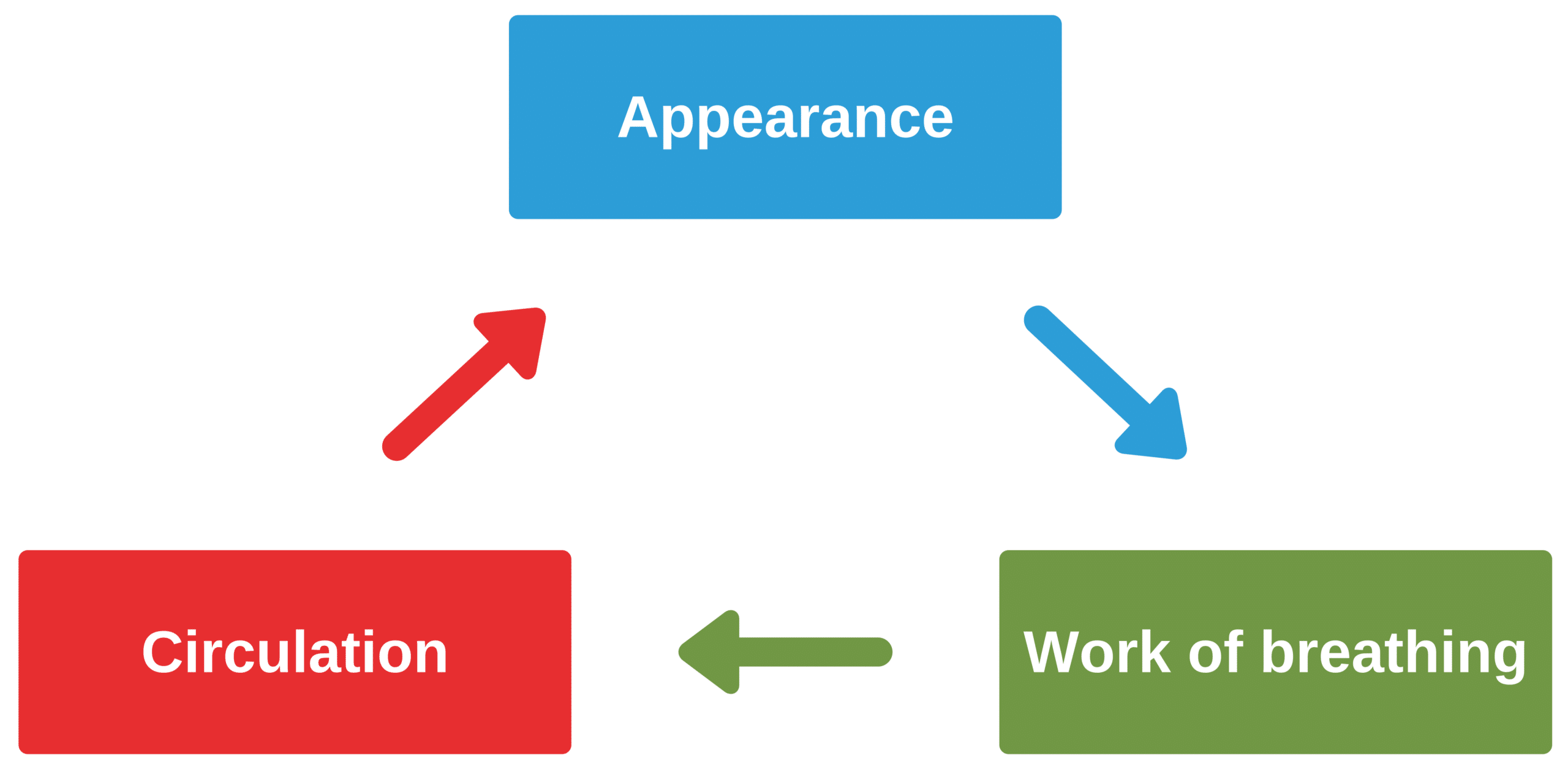
Pediatric Assessment Triangle (PAT).
Related Video – Pediatric Assessment Triangle
Appearance
A child’s appearance can help determine their level of consciousness. Is the child awake and crying? Alternatively, is the child unconscious or not arousable?
Other signs that provide clues to the child’s level of consciousness are included in the mnemonic TICLS: tone, level of interaction, ability to be consoled, the child’s look, gaze or stare, and the child’s speech or cry.
The PALS provider must keep the child as calm as possible to better assess the child’s clinical status. Some strategies include having the parents hold the child or using a toy for distraction if clinically feasible and the condition is non-life-threatening.
Work of Breathing
It must be quickly determined if the child is in respiratory distress or respiratory arrest. A child in respiratory distress will present with nasal flaring, retractions,grunting, stridor, or wheezing. The child’s positioning should be noted. If the child has positioned themselves in a tripod position, they may be in respiratory distress. The provider should auscultate the chest to ascertain the quality of breathing and the presence of abnormal breath sounds such as rales.
Circulation
Observing the child’s skin color is one way to assess for overall tissue perfusion, oxygenation, and the presence of significant bleeding if trauma is likely. Poor perfusion or oxygenation will present on the skin as pallor, cyanosis (particularly of the lips and fingernails), or mottling. On the other hand, if a patient has a reddish or flushed skin coloration, it may be a sign of fever or shock from anaphylaxis sepsis, or toxins.

Note the infant’s bluish skin tone (cyanosis).
Bruising may indicate an accidental or intentional injury. Petechiae and purpura indicate bleeding into or under the skin and can be seen with conditions such as meningitis, trauma, low platelets, or other severe, life-threatening conditions.

An Infant With Severe Meningitis
When performing this initial assessment, the patient’s skin should be exposed, particularly the face, arms, and legs, to look for signs of inadequate tissue perfusion or oxygenation.
After the clinician performs a quick assessment, the patient’s condition is categorized as either life-threatening or non-life-threatening. Patients with life-threatening conditions require rapid intervention or transport to a specialty institution. Patients with non-life-threatening conditions can be monitored in the emergency department until discharge.
Life-threatening conditions prompt the rescuer to immediately start life support interventions by activating the emergency response system and continuing the BLS sequence. If the child’s condition is non-life-threatening, the clinician should continue with the systematic approach.
Evaluate-Identify-Intervene
The evaluate-identify-intervene sequence is a process of ongoing assessment and management of the seriously ill child who is not in cardiac arrest. The evaluation phase includes data gathering and performing a primary assessment secondary assessment and diagnostic assessment using laboratory and radiologic tests.
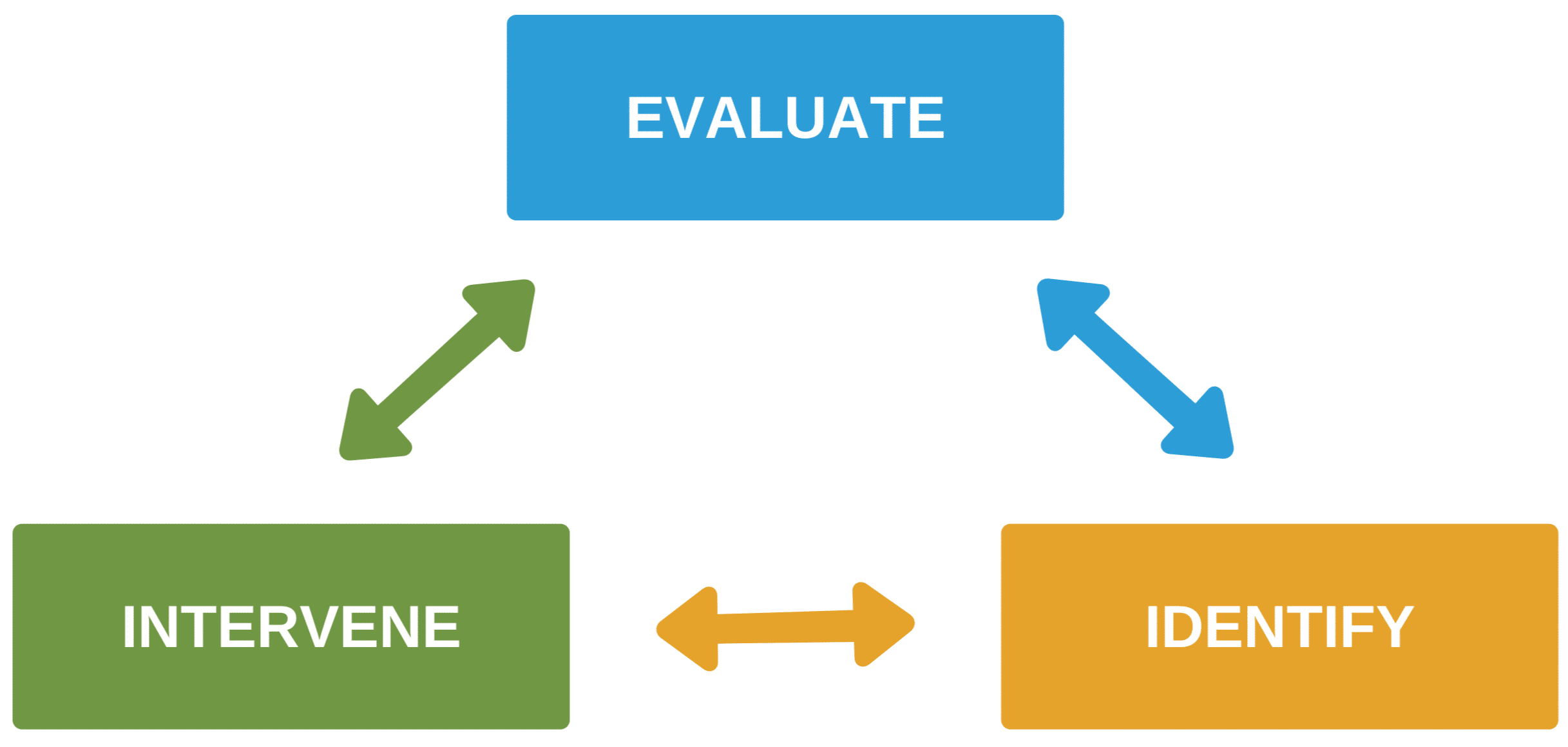
Evaluate-Identify-Intervene sequence
Once the provider identifies a preliminary diagnosis, the team intervenes with appropriate management for the child.
The evaluate-identify-intervene sequence is performed continuously until the critically ill child is stable. This process guides the clinician to treatment and its effectiveness once the team administers an intervention. Children may seem stable upon initial evaluation, only to deteriorate unexpectedly. Children and infants have limited compensatory mechanisms, and upon reaching the limit of those mechanisms, their status can change rapidly.
The following are interventions discussed in this course:
- Maintaining a patent airway
- Activating the emergency response system
- Performing high-quality CPR
- Preparing the crash cart and monitoring the patient
- Utilizing the cardiac monitor and pulse oximeter
- Administering supplementary oxygen
- Supporting ventilation
- Administering fluids and medications
