Pediatric BLS for a Single Rescuer
Short Description
This algorithm ensures that a pediatric patient receives the appropriate BLS care when only one rescuer is available.
Algorithm at a Glance
- Ensure scene safety
- Identify responsiveness
- Check for pulse and respirations
- Perform CPR as needed
- Use an AED when available
Goals for Management
The rescuer will be able to:
- Quickly recognize the need for BLS
- Intervene quickly using rescue breathing (if trained) and high-quality CPR
- Prevent deterioration
The Pediatric BLS for Single Rescuer Algorithm
This algorithm outlines the steps for assessing and managing children presenting with a need for basic life support when a single rescuer is present.
BLS HCP Pediatric Cardiac Arrest Algorithm
Box 1: Ensure Scene Safety
The rescuer looks around the environment to ensure it is safe when tending to a child. If the scene is not secure, the provider moves the child to a safe area. If the area is safe, the rescuer should not attempt to move the child because movement can worsen the injury.
Box 2: Unresponsive Child
The rescuer taps the child’s shoulder, rubs her feet or belly, and shouts, “are you all right?” If the child does not respond, the rescuer calls for help and activates the emergency response system using a cell phone if available. The rescuer can put the dispatcher on speakerphone to facilitate their communication.
Box 3: Visualize Chest Rise and Check Pulse
The rescuer spends no longer than 10 seconds looking for a pulse and checking for breathing. The rescuer should not mistake gasping for breathing.
Box 3a: Pulse Present and Normal Breathing
If the child is breathing and has a pulse, the responder stays with the child until EMS arrives.
Box 3b: Pulse Present and Abnormal Breathing
If the child is not breathing, but they have a pulse > 60 beats per minute, the rescuer begins rescue breathing, providing one breath every 2–3 seconds. The rescuer continues to check the child’s pulse every 2 minutes. If the child has no pulse and no breathing at any time, they proceed to box 4.
Related Video – Understanding Agonal Breathing
Box 4: Witnessed Collapse?
If yes, the rescuer proceeds to Box 4a. If no, they proceed to Box 5.
Box 4a: Activate EMS and Retrieve an AED
If the collapse is witnessed, the rescuer calls emergency response and retrieves an AED.
Box 5: Initiate CPR
If the collapse is not witnessed and the child has a pulse of < 60 beats per minute, the rescuer begins high-quality CPR with 30 compressions followed by two breaths. High-quality CPR continues until the AED arrives. The compression rate should be 100–120 per minute. The depth of compressions should equal one-third of the chest circumference. Full chest recoil occurs between compressions to allow the heart chambers to fill.

A rescuer performs CPR on a child.
Box 6: Activate EMS and Retrieve an AED
After 2 minutes of CPR, the rescuer activates EMS and retrieves an AED if not already done.
Box 7: Attach AED
When the AED is available, the rescuer opens the unit and follows the verbal instructions. The rescuer attaches the pads per the diagram on the AED. The rescuer pauses compressions and allows the AED to analyze the heart rhythm. If the AED determines the rhythm is shockable, the rescuer proceeds to Box 8. If the rhythm is not shockable, the AED will instruct the rescuer to resume CPR. The rescuer proceeds to Box 9.
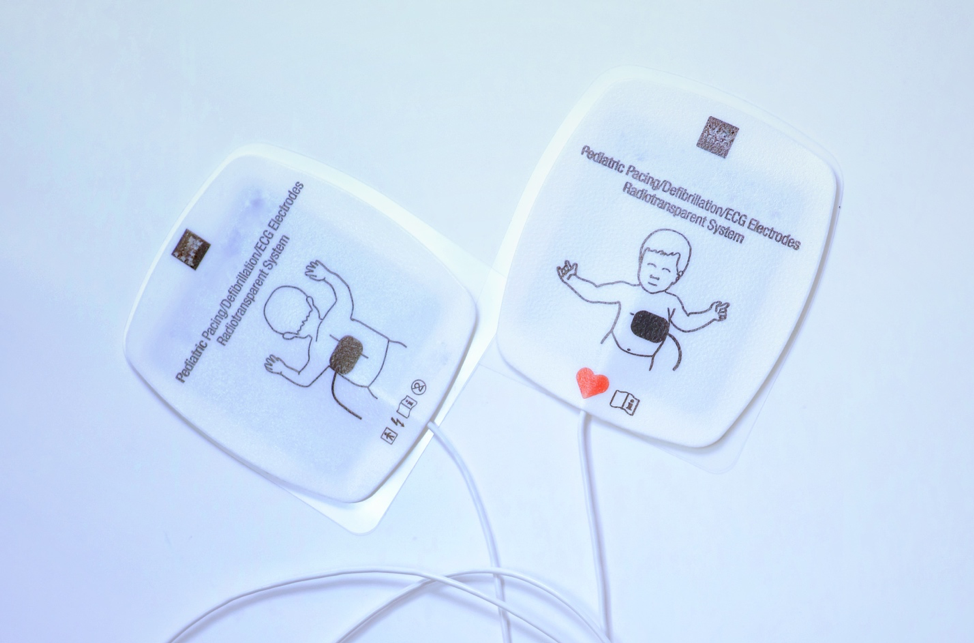
Some pediatric AED pads are placed on the body’s anterior and posterior.
Box 8: Administer Shock
If the AED determines the child’s rhythm is shockable, the AED will tell the rescuer to deliver a shock. The rescuer ensures that no one is touching the child and pushes the shock button on the AED. The rescuer immediately resumes CPR following the shock.
Box 9: Resume CPR
If the AED determines the child’s rhythm is nonshockable, the rescuer immediately resumes high-quality CPR until advised by the AED to stop for a rhythm check. The rescuer continues to provide CPR and shocks until the child moves or EMS arrives.
Chest Compressions
Providing chest compressions for infants is done by placing two fingers in the middle of the chest between the nipples. For children, one or two hands are used to provide the correct depth of compression. The depth of each compression should be 1/3 the depth of the child’s chest.
Related Video – Understanding Infant Landmarks
Breathing
Adult masks should not be used for young children. If the mask covers the child’s eyes or chin, it is too big, and ventilations will not be optimal.
Breaths for a child will typically not be as deep but should be > 1 second each and result in a visible rise of the child’s chest. Unless suspecting a neck injury, the rescuer opens the airway using the head tilt-chin lift technique.