ACLS Case: Respiratory Arrest
Respiratory arrest is defined as absent or significantly inadequate oxygenation and ventilation. Respiratory arrest is not to be confused with agonal gasps with no pulse present. Agonal breathing is an abnormally slow, irregular, or gasping breathing pattern associated with imminent cardiac arrest and may also appear at the onset of cardiac arrest.
Related Video: What is Respiratory Arrest?
Adult Respiratory Rates
There are two types of significant respiratory problems categorized by their severity: respiratory distress and respiratory failure.
Respiratory Distress
Respiratory distress is further divided into mild, moderate, and severe.
In mild respiratory distress, the clinician notices a mildly increased respiratory rate and effort, and there may be some changes in breath sounds such as wheezing or crackles. In severe respiratory distress leading to respiratory failure, there is a more visibly increased respiratory effort, changes in skin color, and altered mental status.
Respiratory Failure
Respiratory failure is the end stage of respiratory distress. Some patients with lesions or toxins affecting the central nervous system where breathing is controlled may be in respiratory failure but lack clinical signs of respiratory distress.
Respiratory failure requires interventions such as assisted ventilation and medications. When left unrecognized and untreated, it can lead to cardiac arrest. Respiratory failure presents as an increase in carbon dioxide (hypercapnia) and a drop in oxygen concentration (hypoxia).
Signs of Respiratory Distress/Failure
Respiratory Arrest
Respiratory arrest is the complete absence of breathing. This is treated with assisted ventilation using a bag-mask device that can provide tidal volumes of approximately 500 to 600 mL.
Higher pressures may be necessary if the patient has poor lung compliance or significant airway obstruction. If the bag-mask device has a pressure release valve, it must give the clinician an option to bypass the valve and provide an adequate tidal volume of about 600 mL.
When a patient is in respiratory arrest, the responder must first ensure that the scene is safe and activate the emergency response system. The next step is to assess the patient by checking the pulse.
If a patient is in respiratory arrest but with a pulse, ventilations must be given every 6 seconds using a bag-mask device or with any advanced airway. Every 2 minutes, the pulse is rechecked for at least 5 seconds but no longer than 10 seconds.

Assessment of respiratory distress includes lung sound auscultation and chest exposure.
Primary Assessment
Responders must learn how to assess the adequacy of ventilation they are providing. If bag-mask ventilation achieves a good and strong pulse and maintains the blood pressure, then insertion of an endotracheal (ET) tube, a laryngeal mask, a laryngeal tube, or an esophageal-tracheal tube may be unnecessary.
Only trained healthcare professionals may use these advanced airways. When inserting an endotracheal tube, it is optimal to confirm correct placement using waveform capnography, in addition to clinical assessment and monitoring of placement.
Related Video: What is the Respiratory Assessment?
Key Takeaway
Avoid overventilation caused by too many breaths or too large a volume for each breath. Hyperventilation can result in decreased blood flow to the brain.
When providing ventilation to patients in respiratory arrest with a pulse, the rescuer should deliver 1 breath every 6 seconds.
If chest rise is not visible, one must assume inadequate ventilation and take appropriate steps to open the airway.
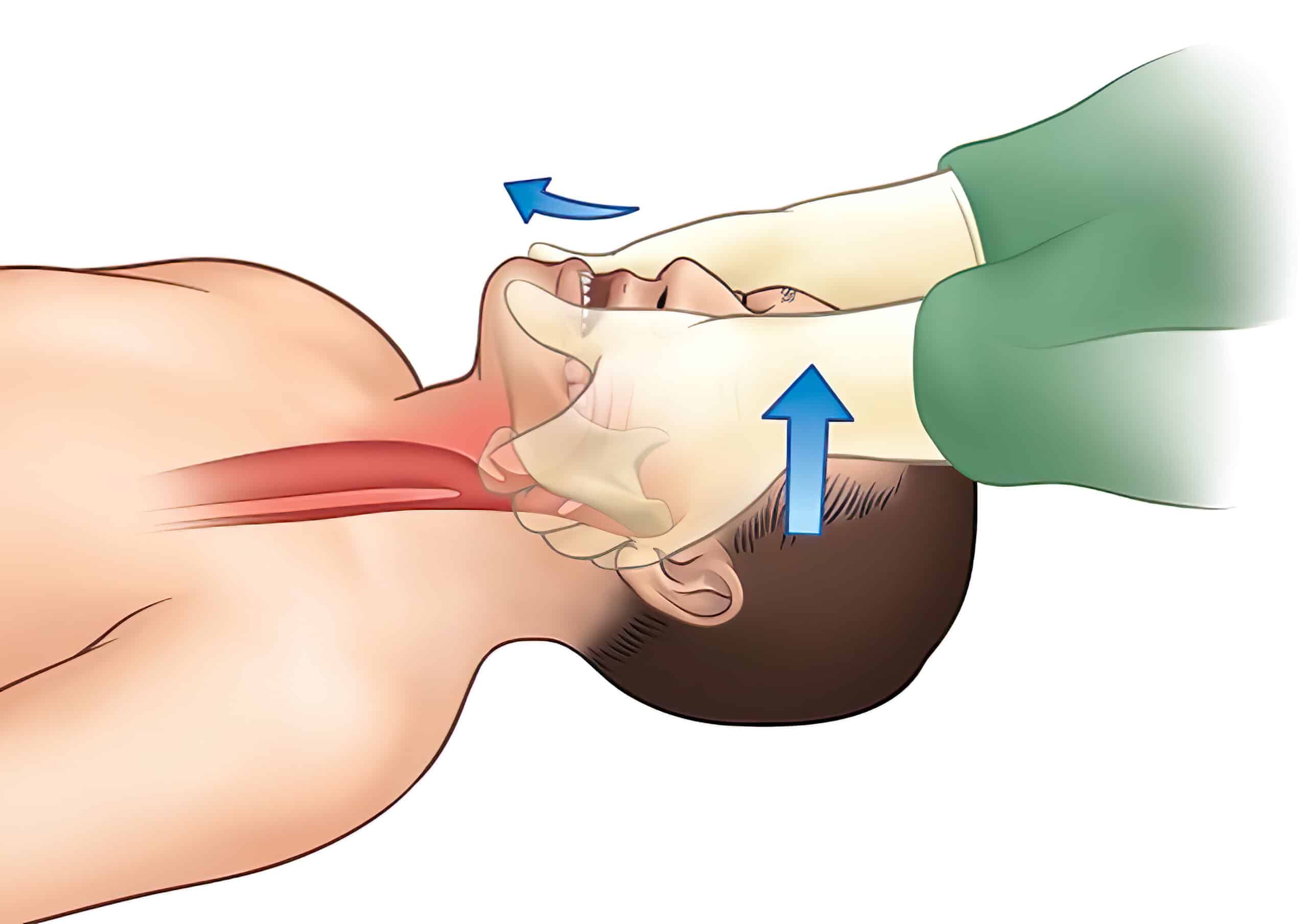
Head-tilt/chin-lift.
Responders must also be aware that excessive ventilations cause negative outcomes. The team should avoid too many breaths per minute or too high a volume for each ventilation.
Overventilation can lead to increased intrathoracic pressure, reduced coronary perfusion, increased gastric inflation, and decreased survival rates. Between compressions during CPR, a negative pressure develops in the chest, which forces venous blood back to the heart. More frequent ventilations mean less blood return to the heart, resulting in reduced CPR effectiveness.
Typically, individuals breathe at a rate of 12 to 16 breaths/minute. If compressions are adequate, there is no reason to provide a ventilatory rate higher than that.

Rescuer providing positive pressure ventilation.
Management of Respiratory Arrest
The management of respiratory arrest involves giving supplemental oxygen, opening the airway, giving necessary ventilation, utilizing essential airway adjuncts, and suctioning. When giving oxygen, the responder should aim to administer a 100% fraction of inspired oxygen (FiO2).

Pulse oximeter in use.
The most common cause of upper airway obstruction among unconscious patients is laxity of the throat muscles and the lack of tone necessary to keep the airway open. The tongue can potentially fall back into the pharynx, causing airway obstruction as well.
Tongue obstructing the airway.
Airway Management and Rescue Breathing
Airway Skills
To properly ventilate the patient in respiratory arrest, the responder must be adept in the following basic skills:
- Head tilt-chin lift maneuver
- Jaw-thrust without head extension maneuver
- Mouth-to-mouth ventilation
- Mouth-to-nose ventilation
- Mouth-to-barrier device ventilation
- Bag-mask ventilation
- Basic airway adjuncts
- Suctioning
- Advanced airway adjuncts
Key Takeaway
For a review of airway skills, refer to the Adjuncts for ACLS chapter in this guide.
Related Video: Maintaining Airway Patency
Respiratory Arrest in Patients With Trauma
For patients with a cervical spine injury, the rescuer needs to avoid unnecessary spinal movements when opening the airway and giving ventilations. Spinal alignment must be maintained at all times to prevent spinal cord damage that may be irreversible. For patients with multiple traumatic injuries, particularly in the head and neck area, the team should always suspect a cervical spine injury.
Special precautions are necessary, such as using the jaw-thrust method to open the patient’s airway. When performing the jaw-thrust, the neck should not be extended. If this maneuver is ineffective, it is a priority to open the airway, and the team must use the head tilt-chin lift method.
Jaw-thrust technique.
For multiple rescuers, one rescuer must stabilize the patient’s head in the neutral position during airway manipulation. Manual spinal restriction is recommended rather than using neck braces or cervical collars. Studies show that cervical collars complicate airway management to the point that it interferes with maintaining a patent airway.25
Spinal immobilization devices are also available and may be used during transport.
Key Takeaway
The rescuer must be skilled in identifying the indications and use of basic and advanced ventilation techniques.
Refer to the ACLS Adjunct chapter in this guide for more detailed information.
Basic ventilation techniques include:
- Maintaining a patent airway by positioning
- Mouth-to-mouth or mouth-to-nose
- Bag-mask ventilation
- Oropharyngeal airway
- Nasopharyngeal airway
Advanced ventilation techniques include:
- Esophageal-tracheal tube
- Endotracheal tube
- Laryngeal mask and tube
25 Yuk M, Yeo W, Lee K, Ko J, Park T. Cervical collar makes difficult airway: a simulation study using the LEMON criteria. Clin Exp Emerg Med. 2018;5(1):22–28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5891742/
