Out-of-Hospital Cardiac Arrest
OHCA: When Communities Fight Cardiac Arrest
To address mortality from OHCA, communities must play an essential role in creating an organized program for training laypersons to provide bystander CPR and early defibrillation. These two interventions increase resuscitation success rates.
With limited access to equipment, a trained layperson performing hands-only CPR is equivalent to an EMS responder performing traditional CPR in adult patients with witnessed OHCA.15 A follow-up meta-analysis found compression-only CPR superior when performed by untrained bystanders in the first 4 minutes of the cardiac arrest.16
Once communities organize resources and training, they can be part of the community link in the OHCA chain of survival.
Dispatcher Recognition of and Instructions for Cardiac Arrest
Emergency dispatchers must know if a patient is in cardiac arrest even though they are not present on the scene. Scripts and protocols are developed to guide EMS and community dispatchers in directing the bystander during an OHCA.

Dispatcher providing callers with instructions for chest compressions via AHA, CPR, and ECC guidelines.17
Some communities have added phone calls, SMS text messages, and social media to alert emergency dispatchers in OHCA situations. One protocol includes the use of computer-generated phone calls and text messages by emergency dispatchers to instruct trained volunteer lay responders to arrive on the scene of an OHCA.
EMS Transition to Hospital
An OHCA patient’s transition to the hospital or receiving facility typically involves ACLS, including advanced cardiac monitoring, 12-lead ECG, other defibrillation or cardioversion methods, vascular access, pharmacologic interventions, and advanced airway implementation and care. Once the patient achieves a return of spontaneous resuscitation (ROSC), ACLS teams provide comprehensive postresuscitation care, including hemodynamic optimization, oxygen, and volume-monitored (ETCO2) ventilation.
An ST elevation myocardial infarction (STEMI) is a significant cause of cardiac arrest. Its treatment involves integrating a well-organized SOC that includes including primary prevention, recognition, EMS, ED, hospital, specialty cardiac center, rehabilitation, and secondary prevention community resources.
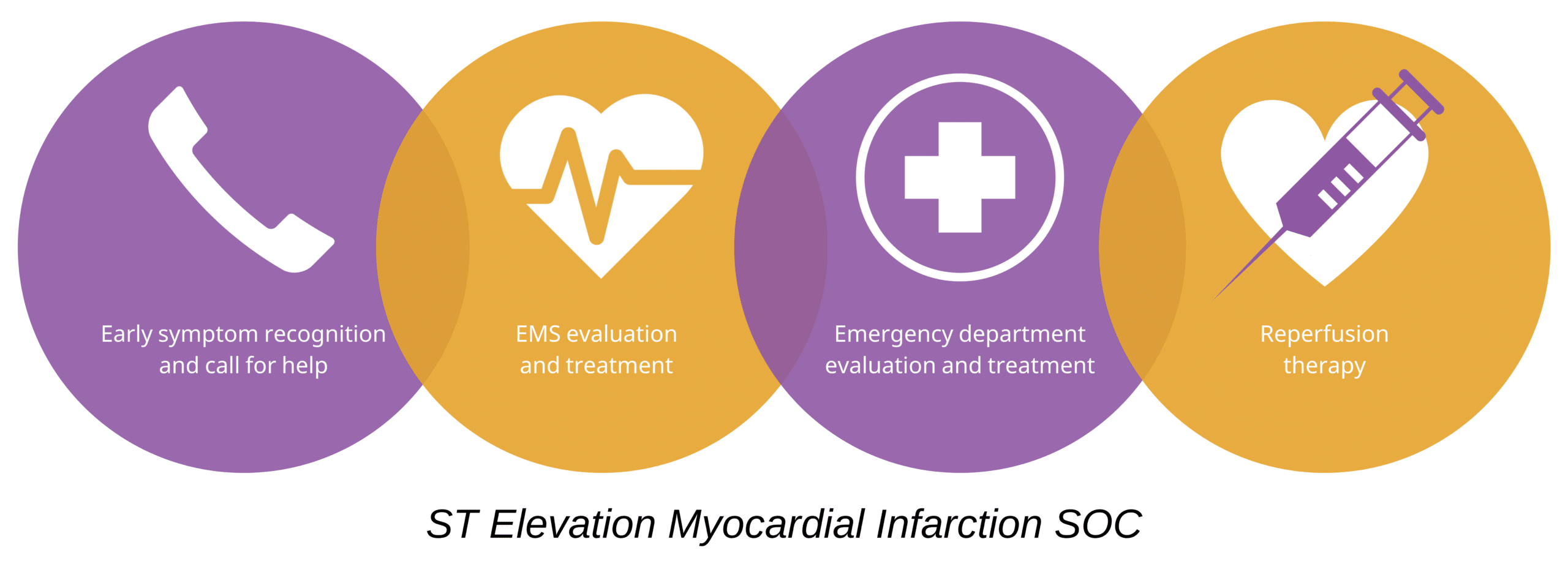
ST Elevation Myocardial Infarction SOC
EMS should transport OHCA patients to hospitals with a certified cardiac care center when such a center is available. A specialized center for cardiac care provides the capability to practice evidence-based resuscitation and post-cardiac arrest care. Studies have shown that there is an association between resuscitation at specialized cardiac arrest centers and improved survival.18, 19
Key Takeaway
Effective OHCA treatment is influenced by:
- Training community members to provide high-quality CPR
- Early defibrillation with an AED or defibrillator
- Early mobilization of EMS responders
15 Sayre MR, Berg RA, Cave DM, et al. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out- of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117(16):2162–2167.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.189380
16 Cabrini L, Biondi-Zoccai G, Landoni G, et al. Bystander-initiated chest compression-only CPR is better than standard CPR in out-of-hospital cardiac arrest. HSR Proc Intensive Care Cardiovasc Anesth. 2010;2(4):279–285.
17 Berg KM, Cheng A, Panchal AR, et al. Part 7: systems of care: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142(suppl 2):S580–S604.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000899
18 Bosson N, Kaji AH, Niemann JT, et al. Survival and neurologic outcome after out-of-hospital cardiac arrest: results one year after regionalization of post-cardiac arrest care in a large metropolitan area. Prehosp Emerg Care. 2014;18(2):217–223.
https://www.tandfonline.com/doi/abs/10.3109/10903127.2013.856507