Routes for Medication Delivery
Timing of IV/IO Access
The rescuer should obtain intravenous or intraosseous access while chest compressions are ongoing. However, in order of priority, the performance of chest compressions comes first, rapid defibrillation second, and establishing IV/IO access is third.
Key Takeaway
Preferred Routes for Medication Administration (in order of preference):
- Intravenous (IV)
- Intraosseous (IO)
- Endotracheal (ET)
Drug therapy is most efficacious when administered IV or IO, IV being the preferred route. Previous studies showed lower survival rates when intravenous or intraosseous access is not available.57 A later randomized trial of adult OHCA demonstrated increased short-term but not long-term survival rates in patients with IV access and drug administration.58
Endotracheal Drug Delivery
Administration of medications via the endotracheal route is a last resort. Higher doses of medications are required to reach the central circulation via this method. If the ET route is the only available route, compressions should be stopped, and the medication delivered. This should be followed by a 5 mL saline flush and five consecutive positive pressure ventilations.
The ET route is not appropriate for all medications. The following mnemonic can be used to remember which medications are safe to administer via the ET route: NAVEL – naloxone, atropine, vasopressin, epinephrine, and lidocaine. Much higher dosages, 2 to 3 times the normal dose, are required when giving medications via this route.
Animal studies have reported enhancement of the β-adrenergic effects of epinephrine given through the endotracheal route, which resulted in vasodilation.59 The clinician must keep this in mind when giving epinephrine via the endotracheal route and be ready to respond quickly if the patient becomes hypotensive.
Peripheral IV Drug Delivery
The most common and preferred route of drug delivery is through the peripheral IV route. During resuscitation, drug dispersion throughout the systemic circulation is limited due to cardiac arrest and thus is dependent on the effectiveness of chest compressions.
Most drugs given by IV push in cardiac arrest should be followed up with a 20 mL bolus of IV fluid to help push the drug into the central circulation. The extremity where the team administers the drug can be elevated to allow gravity to assist in drug dispersion. It is also necessary for chest compressions to continue while the team administers the drug. Selecting the largest vein possible and the largest gauge needle (18 g or larger) that the chosen vein can hold will enhance drug delivery. The veins of the antecubital fossa are large and can be easily accessed while the team performs compressions.

A three-way stopcock can be helpful with multiple drug administration.
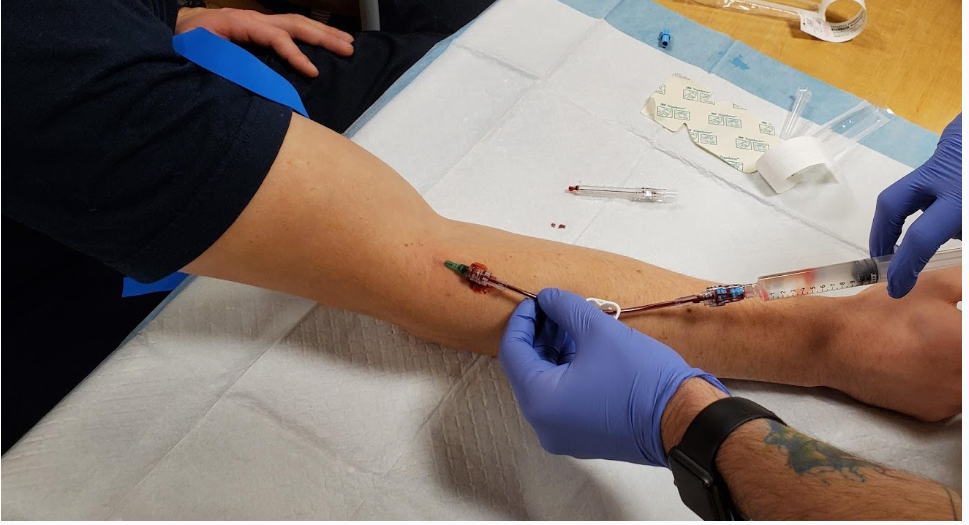
Student practices vascular access technique

Multiple IV Sites on the Same Arm
Intraosseous Drug Delivery
The IO route allows access to a non-collapsible venous plexus. This method of drug delivery achieves a similar effect to peripheral IV access. It is also safe, and the team can use it for sampling blood for laboratory testing. There are no reported contraindications for the use of IO cannulations during cardiac arrest. Therefore, if the team is unable to insert an IV, intraosseous access is a viable option.
Manual pressure or an infusion pump may be required to deliver fluid boluses or medications that are viscous. As with IV administration, drugs given IO should be followed by a saline bolus to ensure delivery into the central circulation.
Central IV Drug Delivery
A central IV line allows for the delivery of higher drug concentrations to the central circulation more rapidly. Moreover, a central IV line also allows access to monitoring other physiologic modalities such as central venous oxygen saturation and estimated cerebral perfusion pressure during CPR. Favorable readings of these two measurements are predictive of ROSC.
The downside of a central IV line is that its placement may interrupt chest compressions significantly as it is difficult and time-consuming to insert, and a specialist is needed. Also, a central IV line is a relative contraindication for fibrinolytic therapy used to treat patients with acute coronary syndrome.
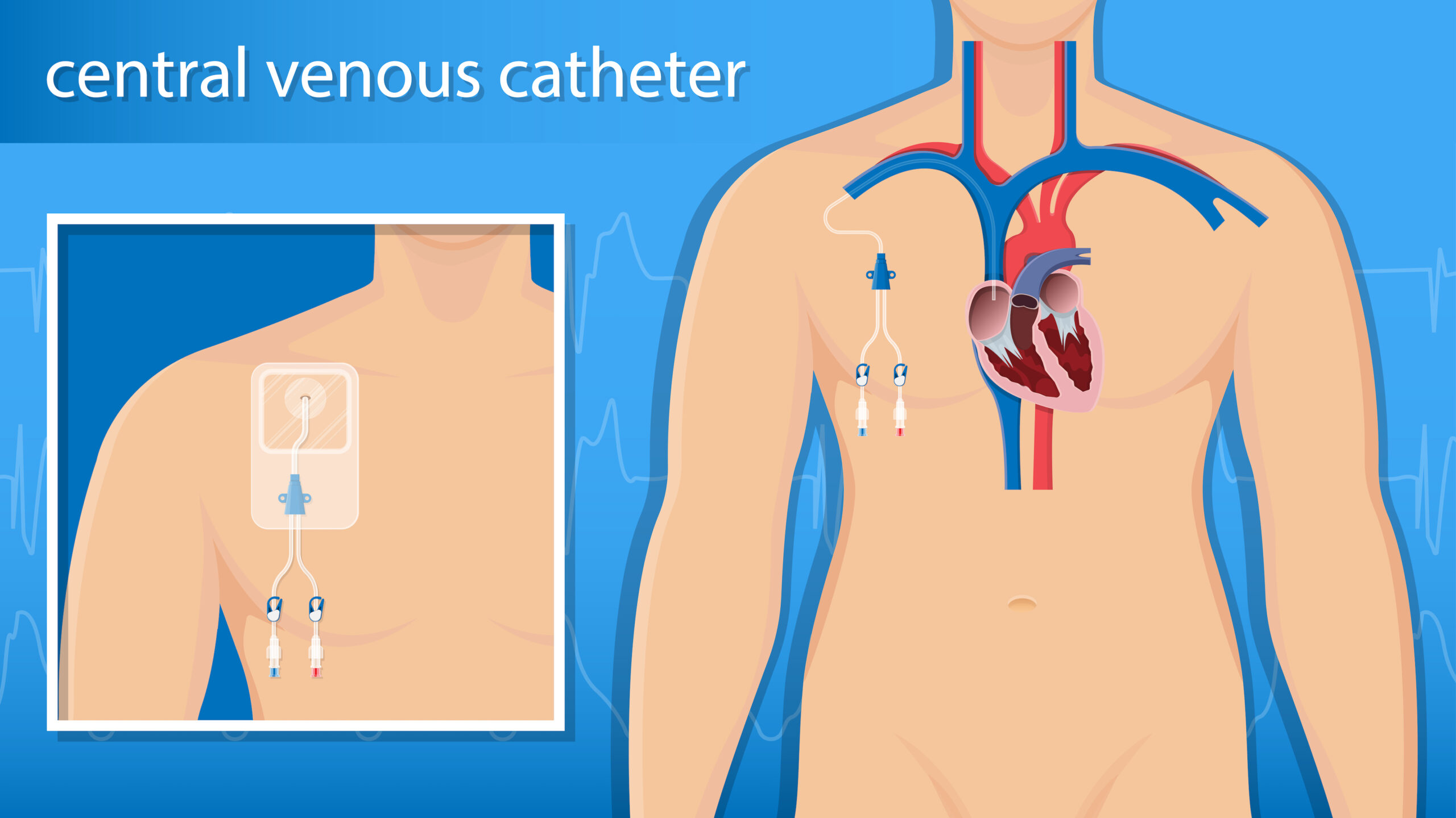
A central IV line is placed into the vein and extends to a location near or into the heart.
57 Kudenchuk PJ, Cobb LA, Copass MK, et al. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999;341:871–878.
58 Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial: a randomized trial. JAMA. 2009;302(20):2222–2229.
59 Elizur A, Ben-Abraham R, Manisterski Y, et al. Tracheal epinephrine or norepinephrine preceded by beta blockade in a dog model. Can beta blockade bestow any benefits? Resuscitation. 2003;59(2):271–276.