ACLS Case: Acute Stroke
Introduction
The incidence of stroke in the United States is estimated to be approximately 800,000 per year. It is a leading cause of severe long-term disability and death.27 Acute ischemic stroke can be treated with medications, while hemorrhagic stroke requires surgery. Both disease conditions require radiologic imaging with an emergent CT scan of the head as the most important diagnostic modality.
For acute ischemic stroke, fibrinolytic therapy with alteplase must be administered within the first hours of symptom onset. Therefore, prompt activation of the emergency response system and dispatch of EMS personnel must occur. EMS personnel must appropriately triage the patient to a stroke center if needed and inform the center before they arrive.

Quick emergency response, including fibrinolytic therapy, is critical for acute ischemic stroke.
Family and community members and BLS responders must learn to recognize the signs and symptoms of stroke and immediately activate the emergency response system.
EMS dispatchers must be adept at suspecting a possible stroke diagnosis and relay that information to the emergency responders. They must also accurately record the time of symptom onset, provide cardiopulmonary support to the caller, and notify the receiving hospital of the impending arrival of a patient with a suspected stroke. It is essential that EMS triage the patient to an institution with a dedicated stroke center if available.
ACLS responders must understand the types of stroke and that the immediate focus is to identify ischemic stroke. The most critical modality when determining the use of fibrinolytic therapy is a CT scan of the head to confirm that the acute stroke is secondary to ischemia. Fibrinolytic therapy is contraindicated if the stroke is hemorrhagic. Best practice is for the stroke team to be activated prior to patient arrival and for the patient to be taken directly to the imaging center.
Stroke Types
The ACLS team must understand the initial in-hospital management of acute stroke. For the patient triaged as having an acute stroke, the team should pursue the stroke pathway and consider admitting the patient to a stroke unit.
They should determine if a patient is eligible to receive fibrinolytic therapy with alteplase and how to administer this treatment within the recommended time frame under the supervision of a neurologic specialist. The National Institute of Neurological Disorders (NINDS) has advised that the recommended time frames are critical success factors and must be achieved in at least 80% of patients with acute stroke.
Key Takeaway
Pharmacologic Treatments and Adjuncts for Acute Stroke
- Alteplase (approved fibrinolytic agent)
- Glucose D50
- Labetalol
- Nicardipine
- Enalaprilat
- Aspirin
- Nitroprusside
The ACLS responder must also be aware of pharmacologic therapies and other treatment options for acute stroke, such as endovascular therapy.
An ECG to evaluate for arrhythmia (a potential cause of embolic stroke) does not take precedence over a CT scan. However, the value of the ECG is in identifying an acute myocardial infarction (AMI) or an arrhythmia such as atrial fibrillation. These two conditions can lead to an embolic stroke.
The Adult Suspected Stroke Algorithm
Short Description
This algorithm outlines the steps to efficiently assess patients and manage suspected stroke.
Related Video: How Do You Treat a Stroke?
Algorithm at a Glance
- The lay rescuer recognizes the signs and symptoms of a stroke and calls EMS quickly.
- EMS begins the assessment and treatment process and transports the patient as rapidly as possible.
- The patient bypasses the ED and is taken directly to the imaging suite, where the stroke team is waiting whenever possible.
- Personnel stabilize the patient and obtain an emergent head CT scan.
- The stroke team does a more in-depth neurological assessment to determine appropriate definitive treatment.
- In the case of a hemorrhagic stroke, the clinician immediately calls for expert consultation.
- In the case of a nonhemorrhagic stroke and in the absence of contraindications, the clinician considers the administration of alteplase.
- Endovascular treatment (EVT) is considered for patients with nonhemorrhagic stroke who are not alteplase candidates and for patients who received alteplase.
- Following definitive treatment, the patient is continued on the poststroke pathway as defined by the facility.
Goals for the Management of Adult Suspected Stroke
The team must succeed in the following to successfully manage suspected stroke in adult patients:
- Quickly recognize stroke.
- Use brain imaging to rapidly differentiate between hemorrhagic and ischemic stroke.
- Complete the scan within 20 minutes of hospital arrival.
- Complete a review of the scan within 45 minutes of hospital arrival.
- Deliver the appropriate treatment based on the type of stroke as quickly as possible.
- Deliver fibrinolytic therapy within 45 minutes of hospital arrival.
- Provide EVT within 90 minutes for direct admits by EMS and 60 minutes for accepted transfer patients.
- Admit to the appropriate stroke or neuro unit within 3 hours of hospital arrival.
The Adult Suspected Stroke Algorithm
This algorithm was created to present the steps for assessing patients presenting with stroke symptoms and determining management. All ACLS responders must be familiar with the AHA Stroke Algorithm:
Adult Suspected Stroke Algorithm ACLS Guidelines
Related Video: Stroke Algorithm
Box 1: Identifying Signs of Possible Stroke
Acute ischemic stroke is a clinical condition in which there has been no blood circulation to a part of the brain, causing a sudden loss of brain function in the dependent area(s). The signs and symptoms of stroke can be temporary or permanent, depending on how long the area has been deprived of adequate blood flow.
Box 2: Critical EMS Assessments and Actions
A trained EMS responder uses a validated out-of-hospital stroke assessment tool such as the Cincinnati Prehospital Stroke Scale (CPSS) and makes a presumptive diagnosis in < 1 minute.
The sooner EMS personnel bring the patient with suspected stroke to a suitable institution, the better the chances for appropriate treatment. That is because only a dedicated stroke care facility can provide the definitive therapy efficiently and effectively.
EMS personnel can provide supportive treatments to lessen the effects of stroke during transport to the ED. Interventions by EMS en route to the stroke center include:
- Ensuring proper management of the patient’s ABCs
- Initiating stroke protocol
- Providing oxygen for patients with oxygen saturation < 94%, or if oxygen saturation cannot be determined
- Checking the patient’s blood glucose level with appropriate treatment of hypoglycemia
- Performing a rapid neurological assessment within 1 minute using an appropriate tool
- Attempting to establish the time when symptoms started
- Determining the nearest stroke center
- Alerting the receiving facility
- Transporting the patient to the stroke center
Key Takeaway
When a designated Stroke Center is available, transfer the suspected stroke patient to that unit. Studies show better patient outcomes in hospitals with dedicated stroke units.
Related Video: Stroke Assessment and Important Time Frames Outside the Hospital
Box 3: Arrival Imaging Suite or ED
Best practice is for the EMS team to bypass the ED and take the patient directly to the imaging suite where the stroke team is awaiting arrival. When the patient arrives, the in-hospital team completes their assessment and stabilizes the patient within 10 minutes.
The stroke team, consisting of qualified nurses, a neurovascular consultant, and an emergency physician, performs the patient’s neurologic assessment. These team members take a focused patient history, perform a physical examination, and determine the time of the onset of stroke symptoms.
The neurologic assessment also makes use of an evaluation tool such as the National Institutes of Health Stroke Scale (NIHSS) or the Canadian Neurological Scale exam. Neurologic assessment by the stroke team and the CT scan should be completed within 20 minutes of the patient’s arrival.
Critical to the treatment of acute ischemic stroke is determining the time of symptom onset confirmed by multiple informants, who may include the patient, family members, and other potential witnesses. The healthcare staff asks when the patient was last known to be healthy.
The general assessment and stabilization process should include:
- Assessing and managing ABCs and vital signs
- Delivering oxygen to keep the oxygen saturation ≥ 94%
- Completing an emergent CT scan of the brain upon arrival or as soon as radiology is ready if the patient is not brought directly to the imaging suite by EMS
- Activating the stroke team if not activated prior to the patient’s arrival
- If not completed by EMS, establishing IV access and obtaining blood samples
- Assessing and treating hypoglycemia
- Performing a basic neurologic assessment using the hospital’s prescribed tool. An excellent tool is the National Institutes of Health Stroke Scale (NIHSS).
- Obtaining an ECG—this should not delay the CT scan
Box 4: CT Scan Interpretation to Determine Cause of Stroke
The most crucial factor in treating acute stroke is to ascertain whether the patient’s symptoms are due to ischemia or hemorrhage. Hence, an important imaging modality is a noncontrast CT scan of the head. The scan not only detects ischemia or hemorrhage but may also identify if other anatomic anomalies within the brain may have precipitated the stroke.
Key Takeaway
The head CT scan must be obtained within 20 minutes of ED arrival.

A Mobile CT Stroke Unit.

Helicopters efficiently airlift patients.
If the patient is transferred to an institution where a CT scanner is not available, the patient must first be stabilized and then transferred to a higher level of care. Anticoagulation medications must not be given to patients until a CT scan has ruled out the possibility of intracerebral hemorrhage.

A patient awaits a CT scan.
Box 5: Hemorrhagic Stroke Protocol Initiation
If the CT scan detects hemorrhage, a specialist such as a neurologist or neurosurgeon will be consulted to assess the patient for possible surgical intervention and other appropriate treatments.
Box 6: Fibrinolytic Therapy with Alteplase Considered for Patients with Acute Ischemic Stroke
Alteplase is the only currently recommended fibrinolytic medication for nonhemorrhagic stroke. If the team administers alteplase within 3 hours of symptom onset, the patient is likely to have a better outcome. Some patients may be given alteplase up to 4.5 hours after the onset of symptoms. The best results are obtained when the intervention is done in an institution with a specialized stroke unit following the NINDS protocol.
The earlier the treatment is given, the better the outcomes will be. In this step, the patient is reassessed to determine whether the symptoms are quickly resolving. If so, fibrinolytic therapy may not be necessary.
The following table lists the inclusion and exclusion criteria for patients with ischemic stroke who may be eligible for alteplase treatment.
Inclusion and Exclusion Characteristics of Ischemic Stroke Patients for Alteplase Treatment Within 3 Hours of Symptom Onset
Extending the time-dependent criteria for alteplase therapy after the onset of acute stroke symptoms may be possible in certain circumstances.
The next table provides additional inclusion and exclusion criteria for patients who may be eligible to receive alteplase between 3 hours to 4.5 hours from the onset of symptoms:
Ischemic Stroke Inclusion/Exclusion Criteria
The most significant adverse effect of fibrinolytic therapy is intracranial hemorrhage. Minor and major bleeding complications may also occur elsewhere in the body. Other adverse reactions to alteplase are angioedema and transient hypotension.
Box 7: Fibrinolytic Candidacy Decision Point
In this step, the patient is reassessed to determine whether symptoms are quickly resolving. If so, fibrinolytic therapy may not be necessary.
Box 8: Informed Consent and Alteplase Administration
After it is determined that the patient is a candidate for fibrinolytic therapy, the attending physician must discuss the risks and benefits of alteplase with the patient or a family member. After all questions are answered, and the consent has been signed, the attending physician proceeds with the treatment.
The team should not give anticoagulants or antiplatelet therapy for 24 hours after administering alteplase or until a follow-up CT scan at 24 hours reveals that there is no intracranial hemorrhage present.
Related Video: How do You Treat a Stroke?
Box 9: Evaluate for Endovascular Therapy
Patients who are not candidates for fibrinolytic therapy with alteplase are next evaluated for EVT. Patients receiving alteplase should also be assessed for EVT candidacy.
Endovascular Therapy
Selected patients with ischemic stroke can also receive EVT. This treatment is directed toward resolving a clot that may have formed in the intracerebral blood vessels by disrupting its integrity or removing it and restoring blood flow to the associated brain tissue.
Patients who are not candidates for alteplase should still be evaluated for treatment with EVT. The AHA also recommends EVT for some patients (especially those with large vessel occlusions) in addition to alteplase treatment.
Patients appropriate for EVT are among the following:
- Pre-stroke Modified Rankin Scale (mRS) score of 0 to 1
- Causative occlusion of the internal carotid artery or proximal middle cerebral artery (MCA)
- Age 18 years and older
- NIHSS score of 6 or more
- Alberta Stroke Program Early CT score (ASPECTS) of 6 or greater
- Treatment can be initiated (via groin puncture) within 6 hours of the onset of symptoms
The clinician should treat any patients meeting the criteria with EVT in addition to IV alteplase.
Related Whiteboard: What are the Immediate Therapies for Stroke?
Box 10: Decision Point for EVT
The team decides whether to proceed with EVT and obtains consent as appropriate.
Box 11: Patient Quickly Taken to Cath Lab for EVT
Patients who qualify for EVT are taken rapidly to the cath lab.
Box 12: Patient Taken to Neurological ICU Following EVT
After the EVT procedure, the patient is admitted to a hospital inpatient unit capable of providing neurological intensive care. The appropriate poststroke pathway is initiated.
Box 13: Patient Transferred to Stroke Unit, ICU, or Higher Level of Care
Patients with hemorrhagic stroke are transferred to the appropriate inpatient unit or moved to a hospital equipped to provide the appropriate level of care. Patients with nonhemorrhagic strokes who are not EVT candidates are also admitted to a stroke unit, neurological ICU, or transferred to a location with the appropriate level of care. The appropriate poststroke pathway is initiated.
Related Video: Hypertensive Medications For Stroke
General Stroke Care
After successful fibrinolytic or endovascular therapy, and within 60 minutes of arrival to the hospital, the patient receives general stroke care, which includes the following interventions:
- The patient is placed on the stroke pathway, which involves a transfer to the stroke unit for close monitoring of neurologic status and vital signs (blood pressure monitoring is critical). The stroke unit can also provide support for the ABCs.
- If a patient worsens in the stroke unit, a CT scan of the brain is requested. There may be cerebral edema or intracerebral hemorrhage present.
- Patients with acute ischemic stroke should also be monitored closely for blood glucose levels < 60 mg/dL. Insulin should be given through the subcutaneous route to patients with blood glucose levels of ≥ 185 mg/dL.
- The patient should be monitored for complications of fibrinolytic therapy and stroke, including seizures and increased intracerebral pressure. It is critical for the team to monitor for and treat hypertension, as described in the following table:
Hypertension Control for Stroke Patients
Related Video: What is Involved in General Stroke Care?
Related Video Drugs for Hypertension in Stroke
Approach to Stroke Care
Intravenous fibrinolytic therapy is only useful for the treatment of ischemic stroke if given within 3 hours of symptom onset. Some patients in select situations may still be eligible up to 4.5 hours after symptom onset.
EVT should occur within 6 hours of the onset of symptoms. Therefore, prompt diagnosis and access to treatment facilities are necessary when managing patients with acute ischemic stroke. Patients who do not meet criteria for fibrinolysis with alteplase should be considered for EVT. EVT should also be considered for all patients subsequent to treatment with alteplase.
A proposed system of care is the stroke chain of survival, where the community, EMS, and healthcare institutions work together to manage acute stroke.
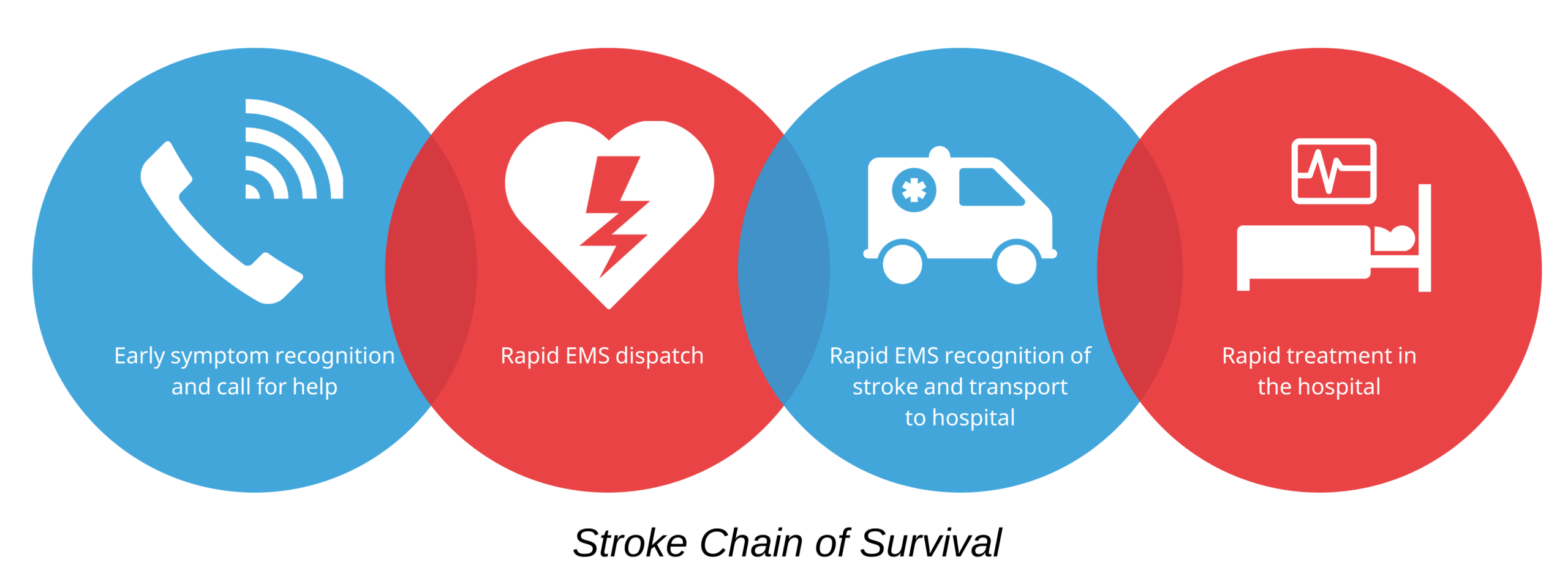
Stroke Chain of Survival
The first link represents the recognition of stroke signs and symptoms by the patient or family members and calling EMS. The second link is immediately dispatching EMS to the patient’s location. The third link is transporting the patient by EMS to a suitable institution, during which EMS personnel perform prearrival notification to the receiving hospital. Finally, the fourth link is diagnosis and treatment in the hospital.
The 8 Ds and Critical Periods of Stroke Care
Another useful mnemonic that showcases the diagnosis, treatments, and potential delays of stroke management is the 8 Ds of Stroke Care based on the Suspected Stroke algorithm:
- Detection – Recognition of stroke symptoms often in the community
- Dispatch – Activation and dispatch of EMS as soon as symptoms are detected
- Delivery – Identification, management, and transport of the patient to a stroke facility
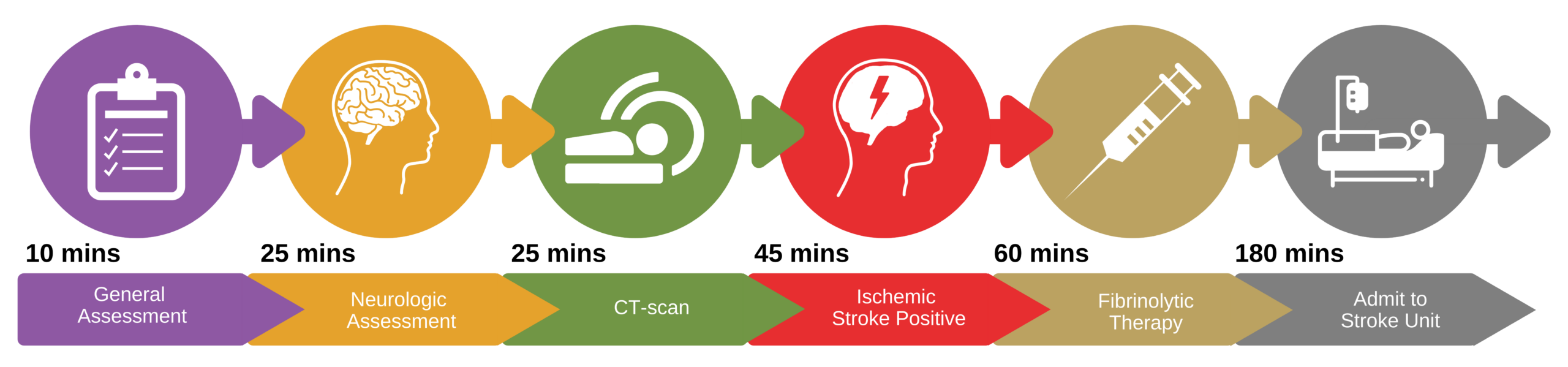
- Door – Arrival at a stroke center
- Data – Collection of data and general assessment by ED physician or stroke expert, ordering a CT scan within 10 minutes of ED arrival. Completion of CT scan within 20 minutes of arrival.
- Decision – Neurologic consult and therapy selection based on the CT scan interpretation within 45 minutes of ED arrival
- Drug/Device – Intervention via fibrinolytic therapy within 45 minutes of ED arrival; EVT door-to-device goal is 90 minutes for direct arrivals and 60 minutes for transfer patients
- Disposition – Admission to stroke unit or ICU within 3 hours of ED arrival
Fibrinolytic Therapy Critical Time Periods
Stroke Assessment
ACLS responders must concentrate on the prehospital care of stroke patients, including a prompt diagnosis that makes use of the stroke scale and rapid transport to an appropriate stroke facility for definitive treatment.
The Cincinnati Prehospital Stroke Scale (CPSS) assesses three clinical signs of a stroke, including facial droop, arm weakness, and abnormal speech. The scale takes under a minute to perform and is a very specific tool for detecting stroke.28 All EMS personnel must be trained to use a validated out-of-hospital neurologic evaluation tool such as the CPSS.
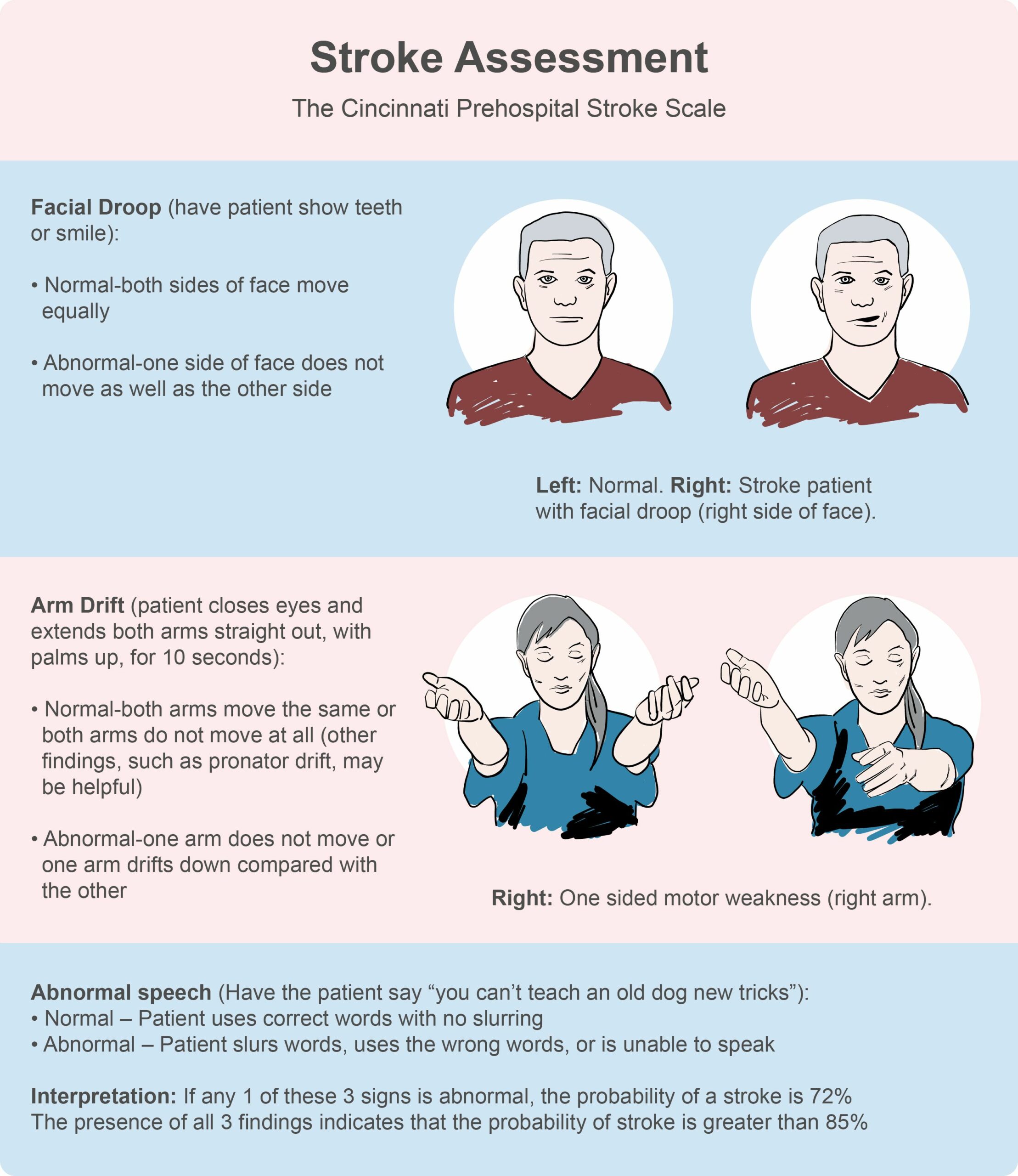
Cincinnati Prehospital Stroke Scale
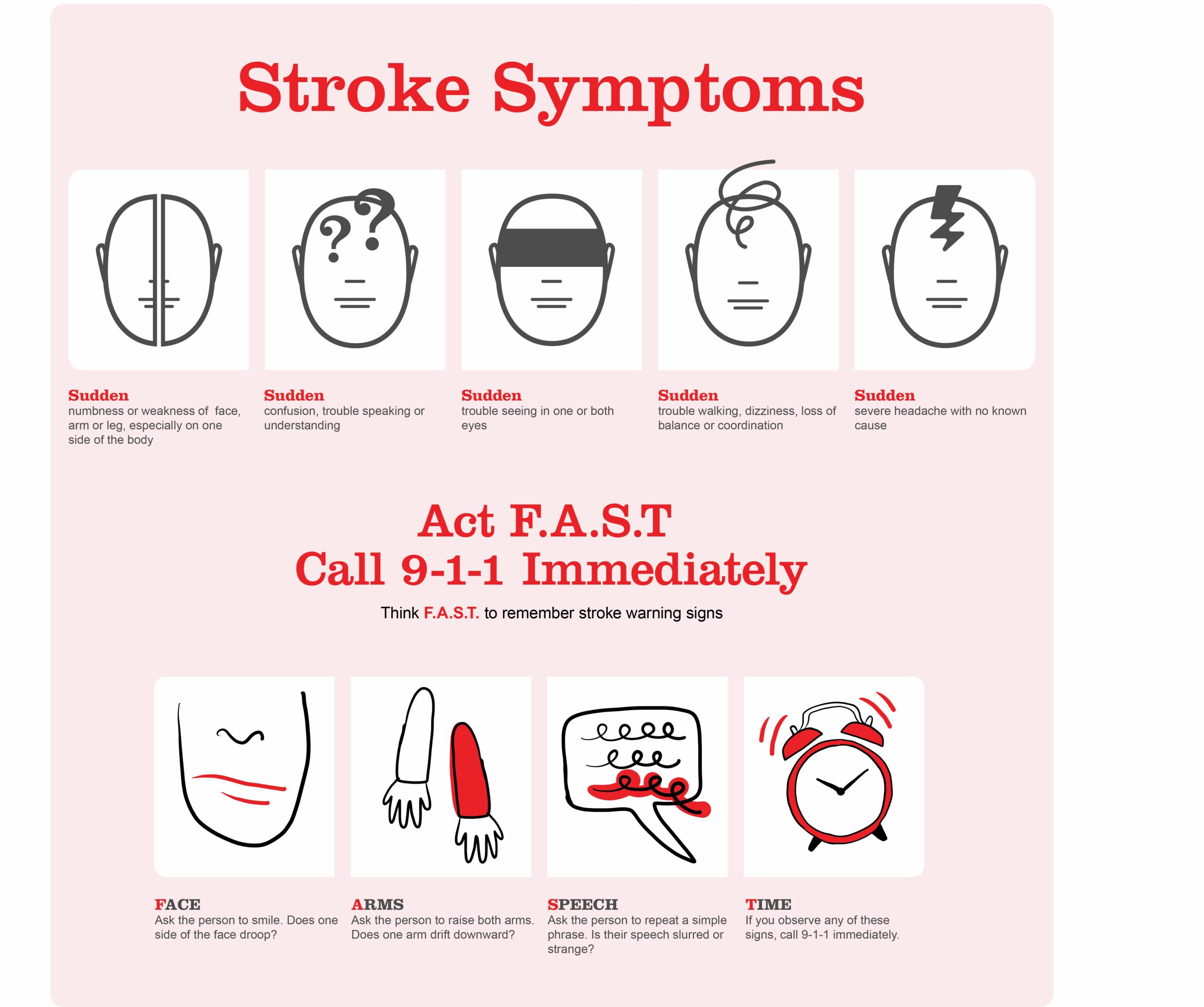
Stroke Symptoms Poster
When these signs and symptoms are apparent, the patient (when able to) or family members should call immediately to activate the EMS system.
27 Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000152
28 Maddali A, Razack FA, Cattamanchi S, Ramakrishnan TV. Validation of the Cincinnati Prehospital Stroke Scale. J Emerg Trauma Shock. 2018;11(2):111–114.