Which Oxygen Delivery Device Should I Choose?
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
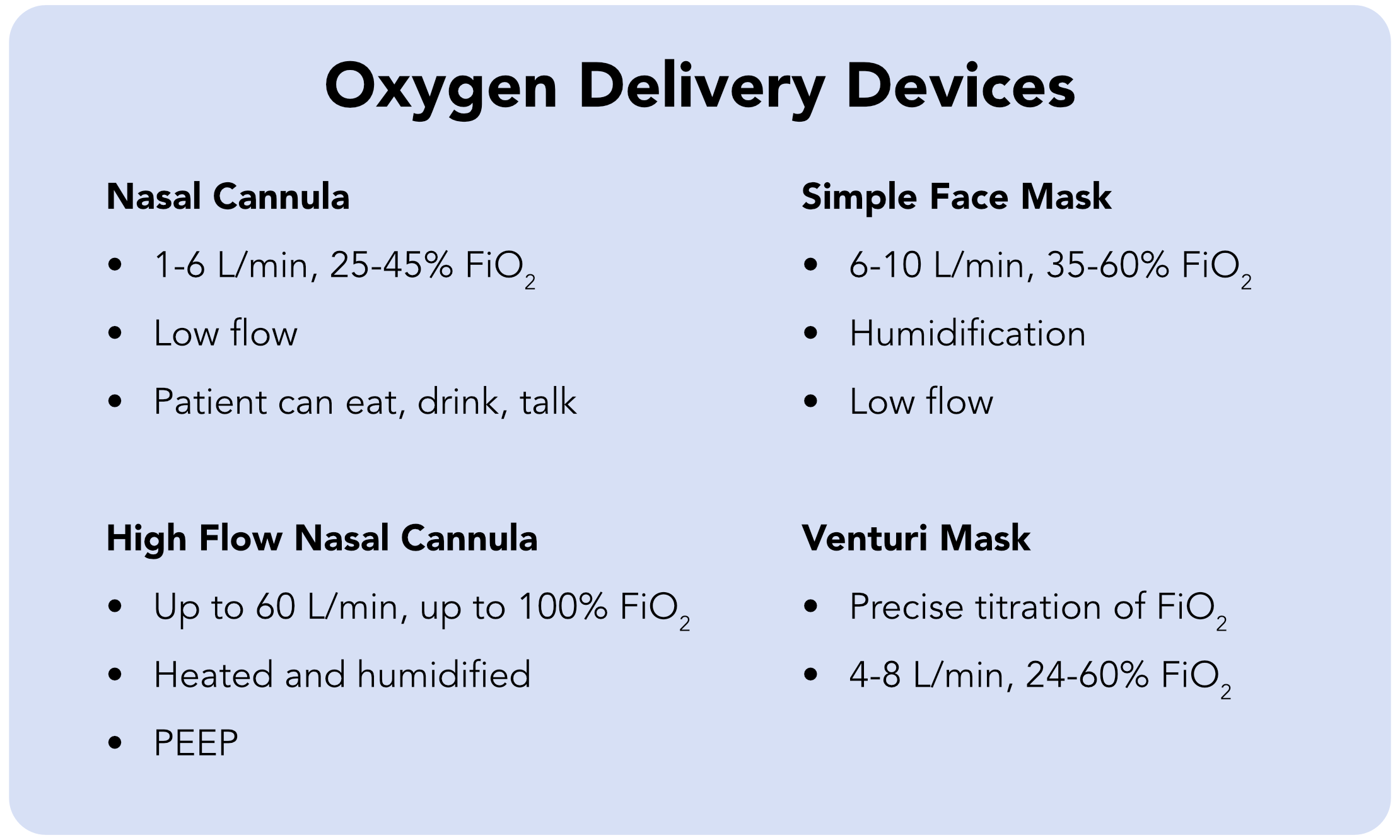
- Four common types of oxygen delivery devices are a nasal cannula, high-flow nasal cannula, simple face mask, and a Venturi mask.
- The fraction of inspired oxygen (FiO2) determines the amount of oxygen a patient actually receives, not the flow rate.
- Clinicians will learn about the different types of oxygen delivery devices.
Oxygen Delivery Devices
The four oxygen delivery devices are:
- Nasal cannula
- High-flow nasal cannula
- Simple face mask
- Venturi mask
Clinicians may also use a non-rebreather mask.
Four Oxygen Delivery Devices
Related Video – Tips for Bagging
“}” data-sheets-userformat=”{“2″:513,”3”:{“1″:0},”12″:0}”>
The nasal cannula is one of the most commonly used oxygen devices. It is a two-prong system that fits into the patient’s nose, and it’s hooked up to the oxygen on the wall. A clinician sets the nasal cannula according to liters per minute, otherwise known as the flow rate. A nasal cannula allows the patient to continue to eat, drink, and talk. A nasal cannula is a two-prong system that delivers oxygen into the patient’s nose. It’s important that providers note flow rate is not the amount of oxygen a patient is receiving, it’s the flow rate programmed by the clinician in the wall dial. A typical flow is between 1–6 liters per minute, so the patient receives anywhere between 25–45% FiO2. That is the actual amount of oxygen the patient receives. The nasal cannula is considered a low-flow device, so it delivers a low amount of oxygen into the nose. Low-flow devices are not able to deliver a precise amount of oxygen. High-flow devices deliver a high amount of oxygen into the patient at a precise amount. The nasal cannula fits into the patient’s nostrils. Clinicians use a nasal cannula for stable patients, setting the flow rate so the patient receives approximately 25% FiO2. A patient experiencing respiratory distress has an elevated respiratory rate. The tachypnea greatly reduces their FiO2. Clinicians can’t control how much FiO2 this patient receives, so a nasal cannula is insufficient. Nasal cannulas do not help with ventilation or the removal of CO2, so clinicians should only use them for stable patients. Read: Shock: Cardiogenic, Hypovolemic, and SepticNasal Cannula


The high-flow nasal cannula is gaining popularity. It’s useful for patients with COPD because it can apply a positive end-expiratory pressure (PEEP) effect. The PEEP effect keeps the alveoli open at the end of expiration by continuing to apply pressure, assisting with ventilation and CO2 removal. The high-flow nasal cannula is a high-flow device. Clinicians can set a flow rate up to 60 L/min, giving the patient up to 100% FiO2. But providers should not put anyone on 100% FiO2 because it can lead to oxygen toxicity, acute respiratory distress syndrome (ARDS), and other complications. A high-flow nasal cannula administers heated, humidified oxygen — a panacea for a patient’s nasal passages. A standard nasal cannula may dry out the nasal passage, which is problematic for patients on blood thinners. They may experience nosebleeds due to the higher risk of bleeding. A high-flow nasal cannula has longer tubing and looks different than the typical nasal cannula, but the patient can still talk, eat, and communicate. The provider should not set the cannula oxygen flow rate above 6 L/min for patients with COPD. These patients breathe differently compared to a patient without COPD. In a patient without COPD, CO2 builds up in the body and stimulates their breathing. Patients with COPD become tolerant to the higher levels of CO2, so it doesn’t stimulate their drive to breathe. Instead, hypoxemia stimulates COPD patients breathing, so their drive to breathe is called a hypoxic drive.High-Flow Nasal Cannula
A note on the Oxygen Flow rate for patients with COPD
Clinicians use simple face masks for patients that aren’t responding well to a nasal cannula due to mouth breathing. A simple face mask can administer more FiO2, but it’s not the preferred choice for a few reasons: The simple face mask is useful for people who prefer to breathe through their mouths.Simple Face Mask

The Venturi mask is considered a high-flow device. It’s connected to blue-green plastic tubing and allows providers to select the precise amount of FiO2. The Venturi mask is adjustable and delivers a specific amount of FiO2. The Venturi mask is designed to offer different levels of FiO2 using different color-coded adaptors. By attaching different color adaptors, the mask directs a specific amount of FiO2. For example, the yellow adaptor administers 35% FiO2. Some Venturi masks have a dial to adjust the FiO2. The Venturi mask flow rate is between 4-8 L/min. The mask doesn’t determine how much oxygen the patient is receiving. Instead, FiO2 determines how much oxygen the patient is receiving, and the Venturi mask precisely delivers specific levels of FiO2.Venturi Mask

The non-rebreather mask is an oxygen delivery device used in emergency situations and consists of a face mask connected to a reservoir bag. Non-rebreather masks have: Often, a non-rebreather mask is used if a patient requires mechanical ventilation and is about to be intubated. Clinicians may use the non-rebreather mask to keep the patient’s oxygen saturation up during pre-intubation. A non-rebreather mask is typically used in emergency situations. Providers must make sure the non-rebreather mask’s bag is fully inflated. They also should not leave a patient on a rebreather mask for longer than 24 hours. These masks are short-term fixes, and if a patient continuously requires a non-rebreather, they should receive a more invasive oxygen delivery intervention, such as intubation or mechanical ventilation.Non-Rebreather Mask

Related Video – Ventilators Basics – Part 1
The four main types of oxygen delivery devices are nasal cannula, high-flow nasal cannula, Venturi, and a simple face mask. The nasal cannula and simple face mask are low-flow devices providers typically use on stable patients or mouth breathers. High-flow devices include the high-flow cannula and Venturi masks, and providers use them to more accurately maintain FiO2.Summary
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.