Multidisciplinary Approach to Postcardiac Arrest Care
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Patients receiving postcardiac arrest care are prone to myriad complications that require multidisciplinary care and support.
- Sedation after cardiac arrest is often necessary to provide comfort and reduce anxiety that can lead to the release of catecholamines, which can have a deleterious effect on the patient.
- Several modalities must be used to determine functionality and predict or diagnose brain death.
- Patients who are diagnosed as having suffered brain death should be evaluated for organ donation.
Neurologic Care
Postcardiac arrest patients with a brain injury are prone to morbidities and mortality, which can occur in 80% of out-of-hospital cardiac arrests and 23% of in-hospital cardiac arrests.1
Brain injuries present as coma, seizures, myoclonus, neurocognitive dysfunction, and brain death. These injuries are caused by the initial ischemic injury and reperfusion.
The initial ischemic injury from cardiac arrest can lead to brain injury.
There are neuroprotective drugs that have been suggested to treat these patients, but studies have not shown improvement in neurologic outcomes. Examples of these drugs include:
- Thiopental
- Glucocorticoids
- Nimodipine
- Lidoflazine
- Diazepam
- Magnesium sulfate
- Coenzyme-Q10
Postcardiac arrest patients who are comatose are monitored for irregular brain activities that may precipitate seizures through an electroencephalogram.2 The standard anticonvulsant drug regimens are recommended for patients with seizures or status epilepticus.
Adult Immediate Post-Cardiac Arrest Care Algorithm
Respiratory Care
Normal arterial carbon dioxide concentration must be maintained. The goal is to achieve an end-tidal carbon dioxide pressure of 30–40 mm Hg. Higher pressures may be considered in the presence of lung injuries or high airway pressure.
When there is increased intracerebral pressure, hyperventilating the patient for a short time may be pursued. Mild hypocapnia produced by hyperventilation will cause cerebral vasoconstriction, preventing an increase in cerebral edema and increased intracerebral pressures.
The clinician must be aware that vasoconstriction decreases brain perfusion. Laboratory values of end-tidal carbon dioxide may be higher than that of the actual values if the patient has a lower than normal core temperature, particularly in patients who have undergone targeted temperature management.
Treatment of Pulmonary Embolism
Pulmonary embolism is treated with fibrinolytics. There is no risk of bleeding to consider when fibrinolytic therapy is given while performing cardiopulmonary resuscitation (CPR) during a reversible cause of cardiac arrest.
Mechanical thrombectomy restores pulmonary perfusion in 85% of patients. Surgical embolectomy also boasts high success rates.
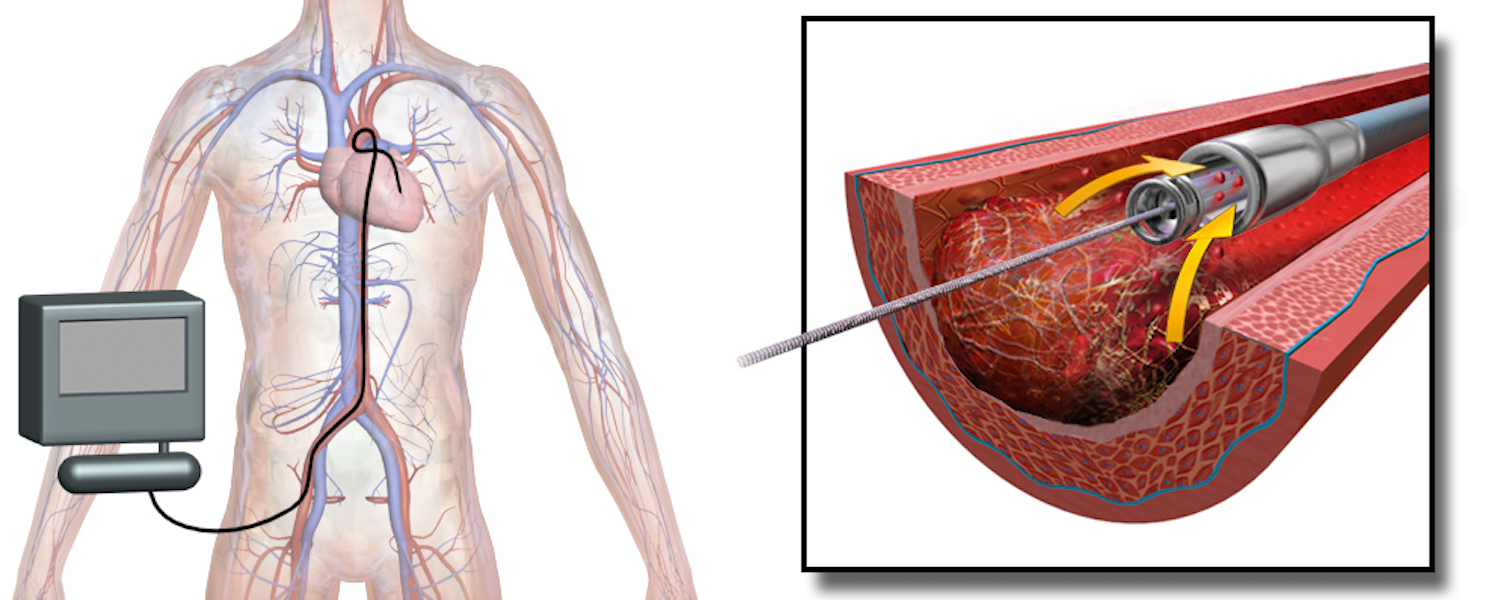
Aspiration embolectomy is a type of mechanical thrombectomy where the thrombus is removed by suction rather than pushing with a balloon.
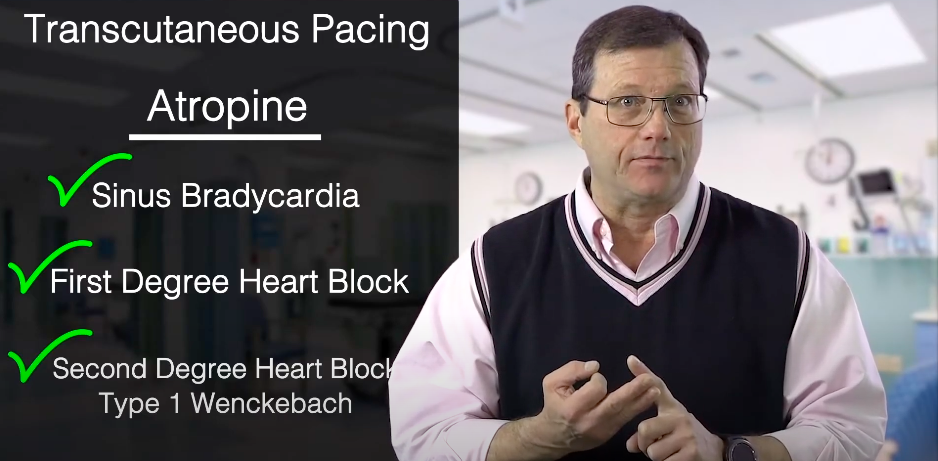
Related Video – Hs and Ts – Pulmonary Embolism
Sedation after Cardiac Arrest
Standard critical care can be taxing on the patient. For example, endotracheal intubation with mechanical ventilation can increase pain and anxiety.2 Sometimes, the resulting cognitive dysfunction from cardiac arrest can precipitate unconscious movements that risk the patient injuring themselves.
Analgesia and sedation provide comfort for these patients. Providers generally use a mix of opioids, anxiolytics, and sedative-hypnotics. The goal is to minimize stress, as stress and anxiety have the potential to increase catecholamine activity.
If a patient is agitated, neuromuscular blocking agents can be used to prevent violent motions. They must be used with caution and in short intervals and with adequate sedation. Neuromuscular blockade must be monitored with a nerve-twitch stimulator. These agents can also mask seizures. Therefore, electroencephalogram (EEG) monitoring is necessary.
Sedation, analgesia, and neuromuscular blockade are also standard treatments when inducing targeted temperature management to control the patient’s shivering and discomfort.
Neuromuscular blocking agents should be used with caution and require close monitoring due to persistent side effects, such as respiratory depression.
Sepsis-like Syndrome
Due to the susceptibility of multiple organs to ischemic injury in cardiac arrest, sepsis-like syndrome can also occur after cardiac arrest. Therapies such as fluid replacement and vasoactive drug administration can improve survival from sepsis.
Steroids
Due to the sepsis-like syndrome precipitated by cardiac arrest, patients are likely to have adrenal insufficiency after the return of spontaneous circulation (ROSC).
Steroids are meant to balance this deficiency. However, no studies have proven the benefits of steroid therapy in postcardiac arrest care. The use of steroids in these patients is of unknown value and requires further study.
Glucose Control
The benefits of glucose control are uncertain in the postcardiac arrest patient because too much insulin or other hypoglycemic agents may lead to hypoglycemia, which is far more detrimental. There are no studies showing any benefit from glucose control in postcardiac arrest care.
Read: Respiratory Arrest
Hemofiltration
Hemofiltration aims to improve the humoral response to ischemic-reperfusion injury after cardiac arrest. However, studies have not shown any benefit in providing hemofiltration compared to patients receiving standard care.4 Hemofiltration does not increase 6-month survival rates among the groups investigated.
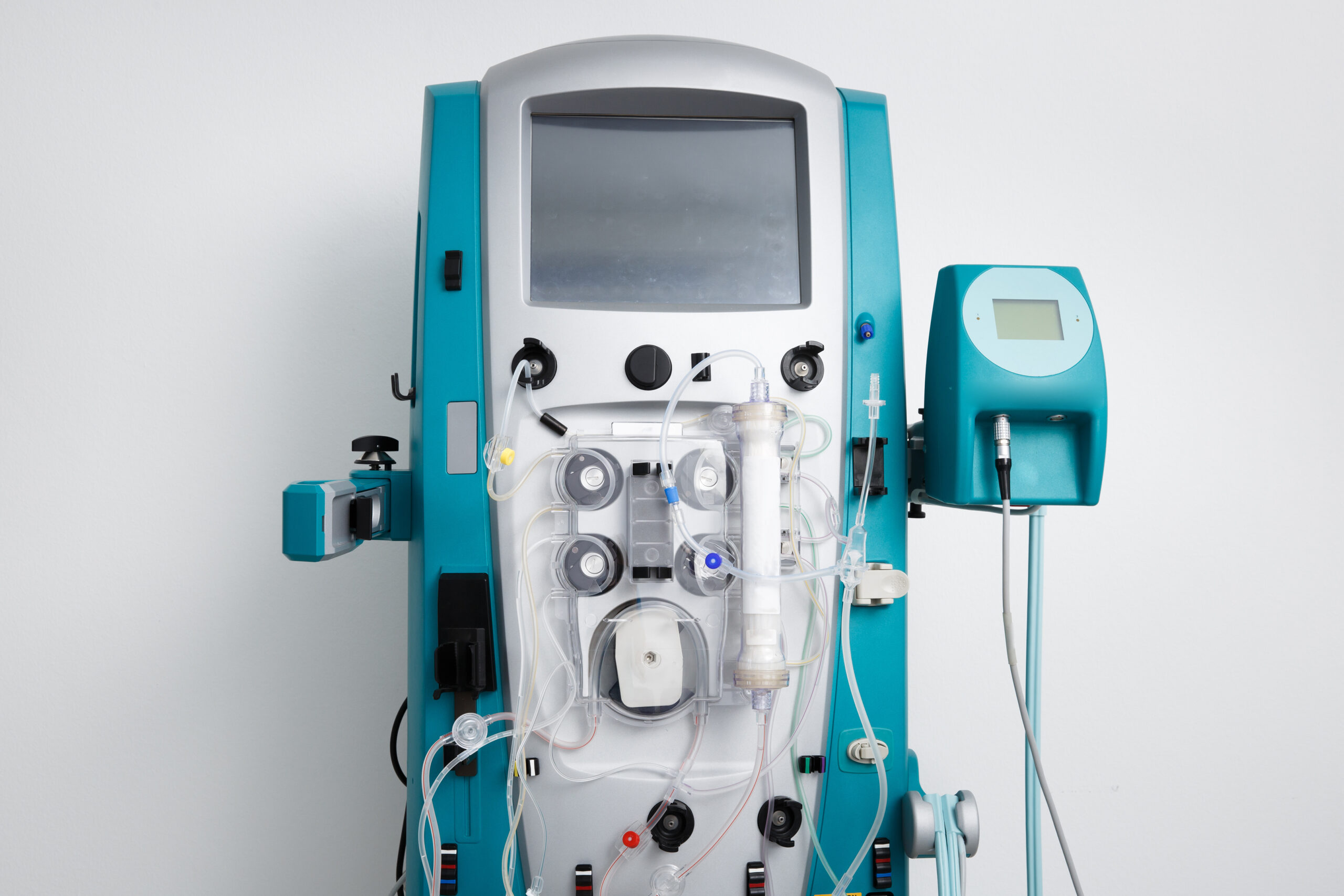
The hemofiltration machine removes inflammatory mediators, such as cytokines, and is thought to reduce the harmful effects on tissues. However, further research is needed.
Prognostication of Outcome
Assessing a postcardiac arrest patient’s functionality is an important endpoint, and determining brain death plays an essential part. Neurologic improvement of derangements involves a good clinical eye, including extensive clinical examination, physiologic and radiologic modalities, and evaluation of biomarkers.
Choosing which tests to perform depends on the clinical aspects of the patient. If a patient recovers quickly, for example, no testing is necessary.
Timing and Outcome Prediction
Prognostication must be performed 72 hours after ROSC in patients who have not undergone targeted temperature management (TTM). If a patient has been treated with TTM, then clinicians must wait 72 hours after the patient has achieved normothermia. That is necessary to avoid false-positive test results from analgesics and neuromuscular blockade.
Most institutions perform a prognostication of postcardiac arrest patients 4–5 days after ROSC.5
Neuroprognostication Assessment
Pupillary Light Reflex
Poor neurologic outcome is expected if the patient is comatose and has no pupillary reflex in response to a light stimulus 72 hours postcardiac arrest (or 72 hours after normothermia is achieved). The clinician observes for pupillary constriction in response to light stimulation in the ipsilateral and contralateral eye. Uneven pupil size is a sign of increased intracerebral pressure.
Motor Movements
Clinical findings of motor movements have high false-positive rates. Motor movements, extensor posturing, and the presence of myoclonus for the sole use of predicting neurologic outcomes are not recommended. These findings can be used to identify which postcardiac arrest patients need further prognostic testing.
For example, the presence of status myoclonus (a prolonged period of jerking movements) during the first 72–120 hours, in combination with other diagnostic tests performed at 72 hours or more after cardiac arrest, helps in predicting poor neurologic outcomes.
EEG Findings
The EEG measures brain and cortical activity and diagnoses seizure activity. Poor outcomes are expected if EEG activity is absent 72 hours after ROSC or 72 hours after the patient has been normothermic. Signs of status epilepticus recorded on the EEG also indicate a poor outcome.
Evoked Potentials
Somatosensory evoked potentials, showing the presence of the N20 waveform after stimulating the median nerve, are signs of good neurologic recovery in postcardiac arrest patients. Performing this test requires highly skilled technicians. It is necessary to eliminate artifacts from muscle twitching.
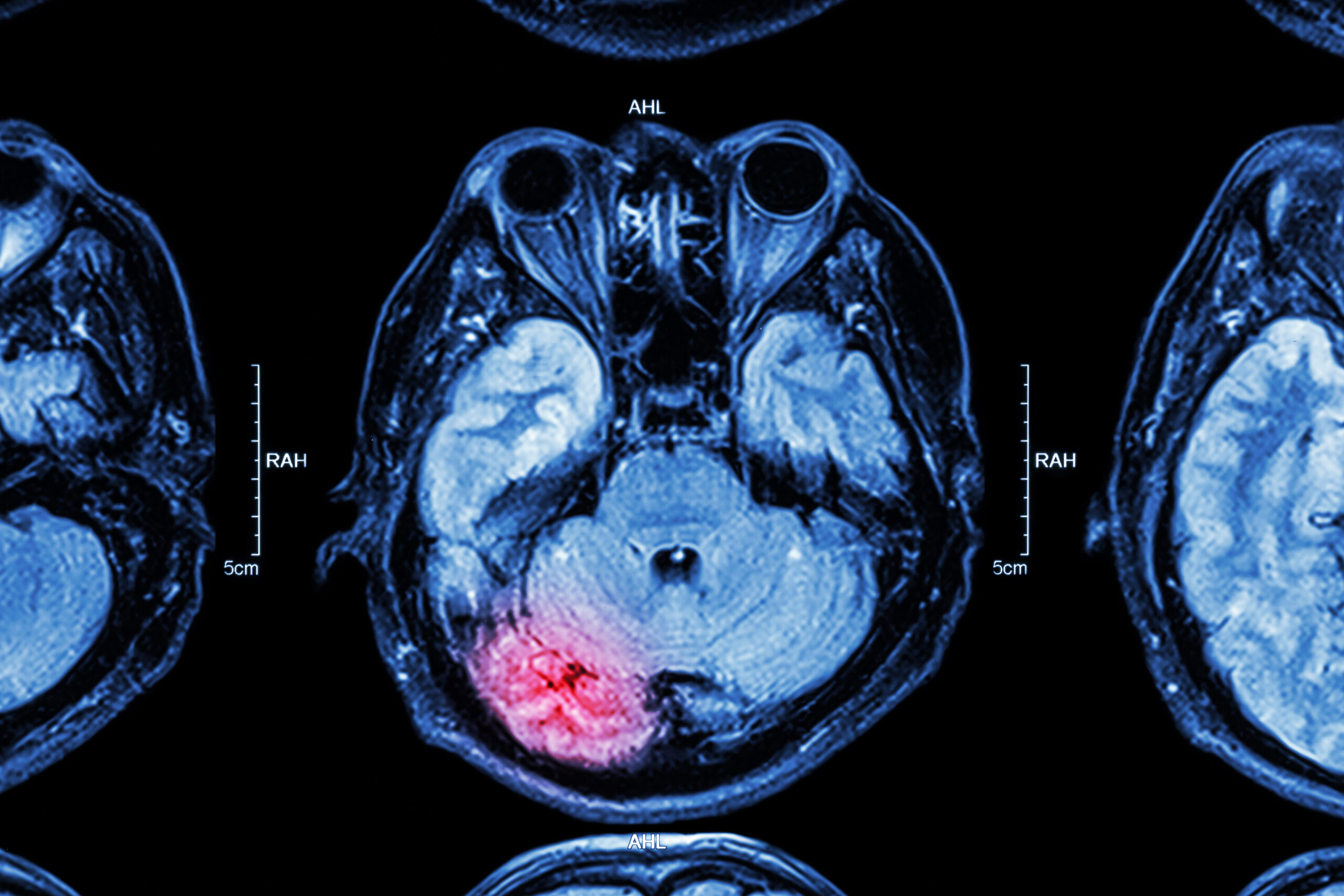
Imaging Tests
The presence of brain edema on a computed tomography (CT) scan is an indication of poor neurologic outcome as evidenced by a lower than normal gray-white matter ratio.
The normal gray-white matter ratio is 1:3. If a CT scan is performed within 2 hours after ROSC, a marked reduction of the gray-white matter ratio is a predictor of poor outcome.6
Magnetic resonance imaging (MRI) can also detect brain edema via restricted diffusion on diffusion-weighted imaging sequences. It is quantified by calculating the apparent diffusion coefficient (ADC). Normal ADC values range from 700 to 800 × 10-6 mm2/second and decrease with edema.
Nuclear single-photon emission computerized tomography (SPECT) imaging of the brain with radiopharmaceuticals can also predict brain death.
Technetium exametazime (Tc-99m) labeled diethylenetriamine pentaacetate (DTPA), hexamethylpropyleneamine oxime (HMPAO), and ethyl cysteinate dimer (ECD) are commonly used.
The absence of radionuclide activity within the brain is consistent with the diagnosis of brain death.
As an adjunct to CT and MRI imaging, nuclear SPECT imaging of the brain with radiopharmaceuticals is an available option.
Blood Markers to Predict Outcomes
Blood markers such as neuron-specific enolase (NSE) and S-100B are used to prognosticate neurologic outcomes. However, studies have shown high false-positive rates.7 Therefore, these are not routinely used to prognosticate neurologic outcomes. NSE and S-100B are not specific to neuronal damage and can be affected by hemolysis, neuroendocrine tumors, myenteric plexus, and muscle and adipose tissue breakdown.
Related Video – Understanding the Post Cardiac Arrest Algorithm
Organ Donation
Cardiac arrest patients who have been resuscitated and then progress to death or brain death must be evaluated for possible organ donation. Patients who do not achieve ROSC after resuscitation must be considered as candidates for kidney or liver donation in institutions that practice these policies.
Some institutions have developed programs that recover the kidneys and liver when ROSC cannot be achieved. These programs rely on continued mechanical circulatory support and very rapid mobilization of the transplant team after the patient is pronounced dead. These institutions have reported more than three organs procured from each donor.
Organs transplanted from these donors, such as adult and pediatric hearts, lungs, kidneys, livers, intestines, cornea, skin, and bone, have very high success rates, which do not differ from any other type of donors.
Summary
The care of postcardiac arrest patients requires a multidisciplinary approach. This article provides an overview of the types of care needed and the precautions that clinicians need to take with these patients.
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Claudio Sandroni, Tobias Cronberg, and Mypinder Sekhon. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis. Intensive Care Medicine. 2021.
2. Elizabeth A. Cahill, PhD, David L. Tirschwell, MD, MSc, and Sandeep Khot, PhD. An Update in Postcardiac Arrest Management and Prognosis in the Era of Therapeutic Hypothermia. The Neurohospitalist. 2014.
3. Judith Ann Tate, Annette Devito Dabbs, Leslie Hoffman, Eric Milbrandt, and Mary Beth Happ. Anxiety and Agitation in Mechanically Ventilated Patients. HHS Author Manuscripts. 2011.
4. Koichiro Shinozaki, Joshua W. Lampe, Junhwan Kim, Tai Yin, Tong Da, Shigeto Oda, Hiroyuki Hirasawa, and Lance B. Becker. The effects of early high-volume hemofiltration on prolonged cardiac arrest in rats with reperfusion by cardiopulmonary bypass: a randomized controlled animal study. Intensive Care Medicine Experimental. 2016.
5. Mary Ann Peberdy, Clifton W. Callaway, Robert W. Neumar, Romergryko G. Geocadin, Janice L. Zimmerman, Michael Donnino, Andrea Gabrielli, Scott M. Silvers, Arno L. Zaritsky. Post-Cardiac Arrest Care. American Heart Association. 2010.
6. Wen Jie Wang, Jie Cui, Guang Wei Lv, Shun Yi Feng, Yong Zhao, Su Li Zhang, and Yong Li. Prognostic Values of the Gray-to-White Matter Ratio on Brain Computed Tomography Images for Neurological Outcomes after Cardiac Arrest: A Meta-Analysis. BioMed Research International. 2020.
7. Robert Ryczek, Przemysław J. Kwasiborski, Agnieszka Rzeszotarska, Jolanta Dymus, Agata Galas, Anna Kaźmierczak-Dziuk, Anna M. Karasek, Marta Mielniczuk, Małgorzata Buksińska-Lisik, Jolanta Korsak, and Paweł Krzesiński. Neuron-Specific Enolase and S100B: The Earliest Predictors of Poor Outcome in Cardiac Arrest. Journal of Clinical Medicine. 2022.