Respiratory Arrest
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- In respiratory arrest, the patient is not breathing or is struggling to breathe but has a pulse.
- Agonal breathing involves abnormal or gasping breaths that occur as a prelude to cessation of breathing.
- It is important to know the normal rate of breathing to recognize when breathing is too fast or too slow.
- Severe respiratory distress can lead to respiratory failure or respiratory arrest.
- The mnemonic DRS ABCD (danger, respond, shout for help, airway, breathing, circulation, defibrillate) is used to remember the steps of basic life support (BLS).
Patients presenting with absent or significantly inadequate breathing but have a pulse are in respiratory arrest. In contrast, if there is no pulse present and there is a complete cessation of breathing or the patient has agonal breathing, the diagnosis is cardiac arrest.
Agonal breathing can be defined as slow and irregular breathing with periods of apnea and may sound abnormal (snoring, gasping, labored, or even moaning).1
Normal breathing (adults): 12–16 breaths per minute with a tidal volume of 8–10 mL/kg. Tachypnea: > 20 breaths per minute. Bradypnea: < 12 breaths per minute. Hypoventilation: Patients present with poor oxygenation and ventilation parameters that necessitate the use of oxygen supplementation or assisted ventilations, such as a bag-mask device.Definition of Terms
The three primary types of respiratory problems are respiratory distress, respiratory failure, and respiratory arrest. The characteristics and other important information about each type of problem are outlined in the following sections.Types of Respiratory Problems
CHARACTERISTICS: SEVERITY: Respiratory distress may be mild, moderate, or severe. Severe respiratory distress indicates impending respiratory failure and is recognized by2: Severe respiratory distress can cause bluish discoloration of the extremities, especially in the fingers and lips.Respiratory Distress

Related Video – How to Manage Respiratory Arrest on an Adult
CHARACTERISTICS: Respiratory failure is the end stage of respiratory distress. It requires interventions such as assisted ventilations and medications.3 There will be an increase in carbon dioxide (hypercapnia) and a decrease in oxygen concentration (hypoxia). SPECIAL CIRCUMSTANCES: Patients with lesions in the central nervous system may be in respiratory distress without showing any significant signs due to disruptions to the autonomic controls.Respiratory Failure
CHARACTERISTICS: Respiratory arrest is the complete absence of breathing. It is treated with assisted ventilation with a bag-mask device that can deliver a volume of 500–600 mL. WARNING: Avoid excessive ventilation because studies have shown that it can cause poor outcomes. Excessive ventilation causes gastric insufflation, regurgitation, and aspiration of stomach contents. Gastric inflation compresses the structures and organs in the mediastinum. The resulting increase in intrathoracic pressure compromises the venous return to the heart, diminishing cardiac output. Respiratory arrest is treated with assisted ventilation using a bag-mask device. Read: Multidisciplinary Approach to Postcardiac Arrest CareRespiratory Arrest

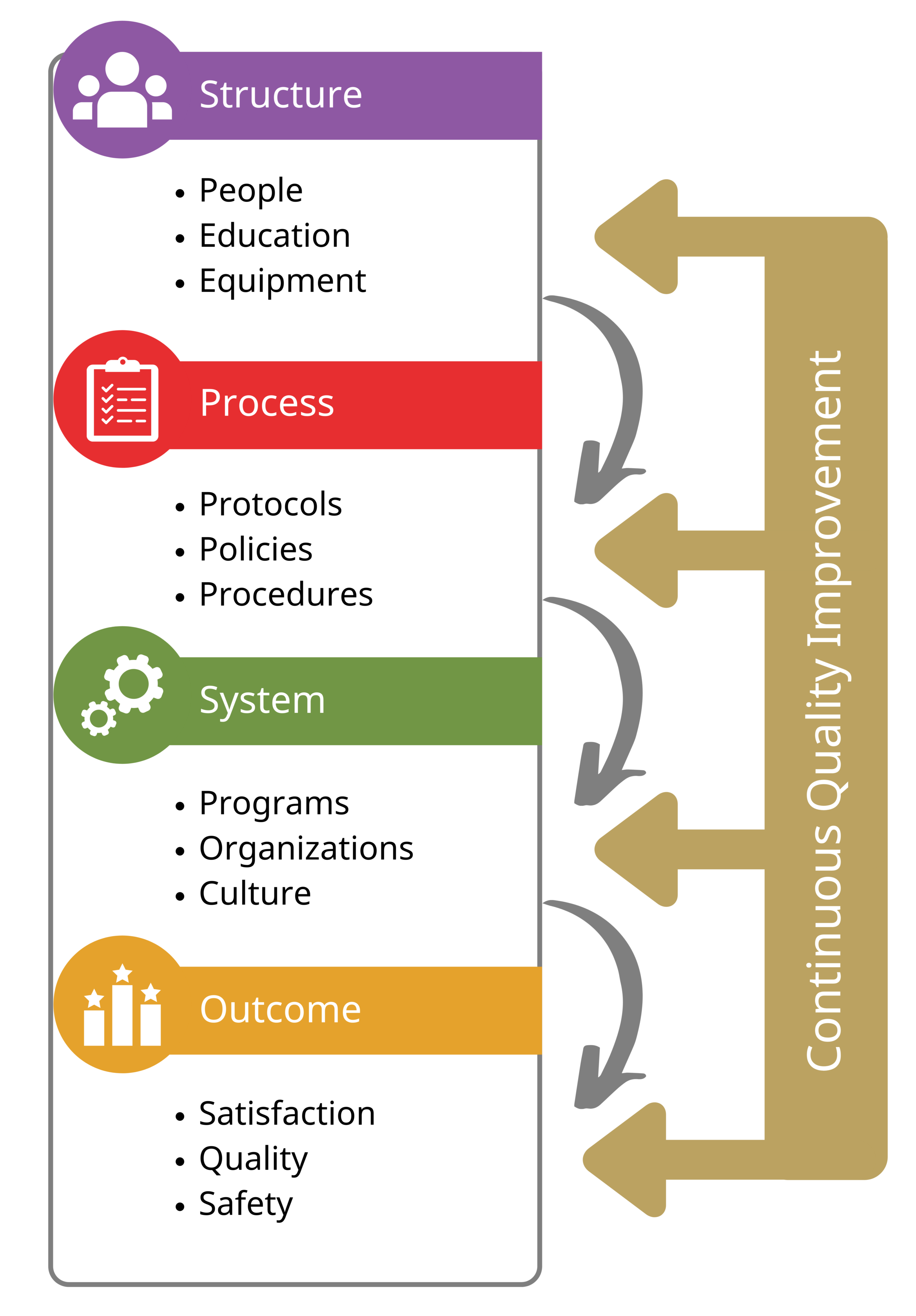
The following explains how a provider should go about the systematic assessment in respiratory arrest.Systematic Assessment in Respiratory Arrest
A foreign object can obstruct the patient’s airway, leading to choking and respiratory arrest.BLS Assessment (Remember DRS ABCD)

A (airway) = The provider should maintain the patient’s airway by performing maneuvers such as the head tilt-chin lift or jaw thrust. Patients in respiratory arrest will have a pulse but are not breathing. Chest compressions and the use of an AED are not necessary at this point. B (breathing) = The rescuer should give assisted ventilations — one rescue breath every 5–6 seconds. Mouth-to-mouth ventilations should only be performed with a barrier device. Medical devices, such as an oropharyngeal airway, nasopharyngeal airway, or a bag-mask device, can be used to assist in giving ventilations. The provider must make sure not hyperventilate the patient. C (circulation) = The provider should check for a pulse every 2 minutes and make sure not to exceed 10 seconds when checking for a pulse.4 If a pulse is present, the provider continues rescue breathing for 2 minutes and checks for a pulse again, repeating the cycle until emergency medical services (EMS) arrives. If the pulse is absent or if the provider is unsure if there is a pulse within 10 seconds, then they should begin high-quality cardiopulmonary resuscitation (CPR). D (disability) = Some communities have adapted treatment protocols for opioid use. If available, give naloxone if the patient is suspected or known to have overdosed on opioids. Many medical professionals (and laypersons) always carry a naloxone kit with them because opioid overdose is so prevalent. When a patient is in respiratory arrest, they have a pulse but are not breathing or are struggling to breathe. The medical provider must understand the types of respiratory problems and how to assess and treat the patient.Primary Assessment
Related Video -Understanding the Steps of the Primary Assessment
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. James Roland. What You Should Know About Agonal Breathing. healthline. 2018.
2. Johns Hopkins Medicine. Signs of Respiratory Distress.
3. Matthew Diamond; Hector L. Peniston; Devang Sanghavi; Sidharth Mahapatra. Acute Respiratory Distress Syndrome. National Library of Medicine. 2022.
4. American Heart Association. Adult Basic Life Support Algorithm for Healthcare Providers.