The Neurological Assessment
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- The patient’s level of consciousness is the most basic indicator of their neurological status.
- The Glasgow Coma Scale assesses eye opening, verbal, and motor response.
- The neurological assessment contains five key steps.
This lesson discusses the neurological assessment, detailing its most important parts. Five topics will be discussed: The rescuer will assess all of these each time they perform a neurological assessment. The intricacies of the neurological assessment are detailed below.Understanding the Neurological Assessment
The level of consciousness is the most sensitive and basic indicator of how the patient is doing neurologically. The level of consciousness indicates how awake and alert the patient is. At the very top of the scale, a patient is awake and alert. The next level down is a lethargic patient. This patient falls asleep easily, perhaps even when the rescuer is talking to them. But they’re still easily aroused. The next level of consciousness is obtunded. These patients fall asleep very easily and are difficult to arouse. Unlike a lethargic patient, a rescuer may have to shake them lightly to wake them. When woken they will talk in sentences. They are easily understood but difficult to arouse. Following obtunded is stuporous. Patients are classified as this level when they are barely above comatose. A stuporous patient is very difficult to arouse. If a clinician does arouse them, they may express themselves in grunts and groans. They will be nonsensical, won’t form words, and will not be able to answer questions. The very last level of consciousness is comatose. These patients don’t wake up. Keep in mind that level of consciousness should not be confused with mental status. Mental status measures something else entirely. Stuporous refers to a patient who is difficult to arouse and unable to form words.Level of Consciousness
Level of Consciousness
Patient Description
Awake and alert
Awake, alert
Speaks appropriately
Lethargic
Falls asleep easily
Easily aroused
Speaks appropriately
Obtunded
Falls asleep easily
Difficult to arouse
Speaks appropriately
Stuporous
Very difficult to arouse
Unable to form words
Comatose
Not able to be aroused
Unconscious
Related Video – Neurogenic Shock Versus Spinal Shock
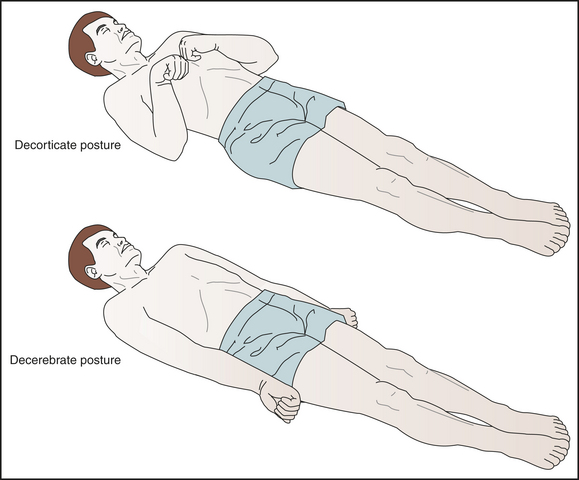
The Glasgow coma scale (GCS) is a neurological scale for objectively evaluating a person’s level of consciousness and mental status. This scale is commonly used following a possible traumatic brain injury. The Glasgow Coma Scale assesses a person’s level of consciousness. The Glasgow coma scale ranges from 3–15. The lowest possible score is a three, which could be a score given to a person who is comatose or dead.. The highest score is a 15. The Glasgow coma scale evaluates three areas of a patient’s overall neurological status, including: Read: Neurogenic Shock vs. Spinal Shock If the clinician enters the room and the patient’s eyes open spontaneously, they get full points. If they must speak to the patient to wake them up, they get one less point. That is still okay as the patient could just be taking a nap. If the clinician needs to pinch the patient or inflict noxious stimuli to encourage them to open their eyes, the patient loses another point. If they don’t open their eyes at all, only one point is awarded. Verbal response helps determine the patient’s mental status. If the patient is oriented to person, place, time, and situation, they receive the full five points. If they’re a little bit confused, they get four points. If they answer the clinician in sentences but don’t make sense, they receive three points. If the only sounds they emit are incomprehensible, they receive two points. Finally, if the patient gives no verbal response, they get one point. There are a few terms regarding mental status which require a bit more clarification. Obviously, the best mental status for a patient is oriented, but even if they are oriented, they can still be confused. A patient can be awake and alert while simultaneously being confused. Mental status refers to such states as confusion, agitation, and delirium. Clinicians will also assess the patient’s motor response. That is performed by entering the room and asking the patient to “squeeze my hands.” The patient receives full points for a motor reaction. If a patient does not obey commands, they lose one point on the scale. Next, a clinician looks for a pain response. There are two levels of response to pain, including: One response is called localizing pain. That is when a clinician pinches the skin over the patient’s sternum, and they reach over and can brush the clinician’s hand away. They’re able to localize the pain as a movement in response to a pain stimulus. The other response is called withdrawal from pain. That occurs when the clinician pinches that same spot on their sternum, and the patient simply moves or turns in the bed. They’re withdrawing from the pain but are not able to localize the source. This response receives a lower score. If the patient can only withdraw as opposed to localize it, they’ve reached posturing. Clinicians note two different types of posturing depending on the patient’s neurological status. The first level is called decorticate posturing. That is when the patient draws their arms into their core as a response to noxious stimuli. Decerebrate posturing is the next level of response to the noxious stimuli. That occurs when the patient hyperextends their arms out and hyperpronates their wrists outward. That is neurologically more worsrisome than decorticate posturing. Decorticate and decerebrate posturing are types of motor responses. Finally, a patient that doesn’t respond to noxious stimuli receives only one point — the lowest level for the motor response.Glasgow Coma Scale
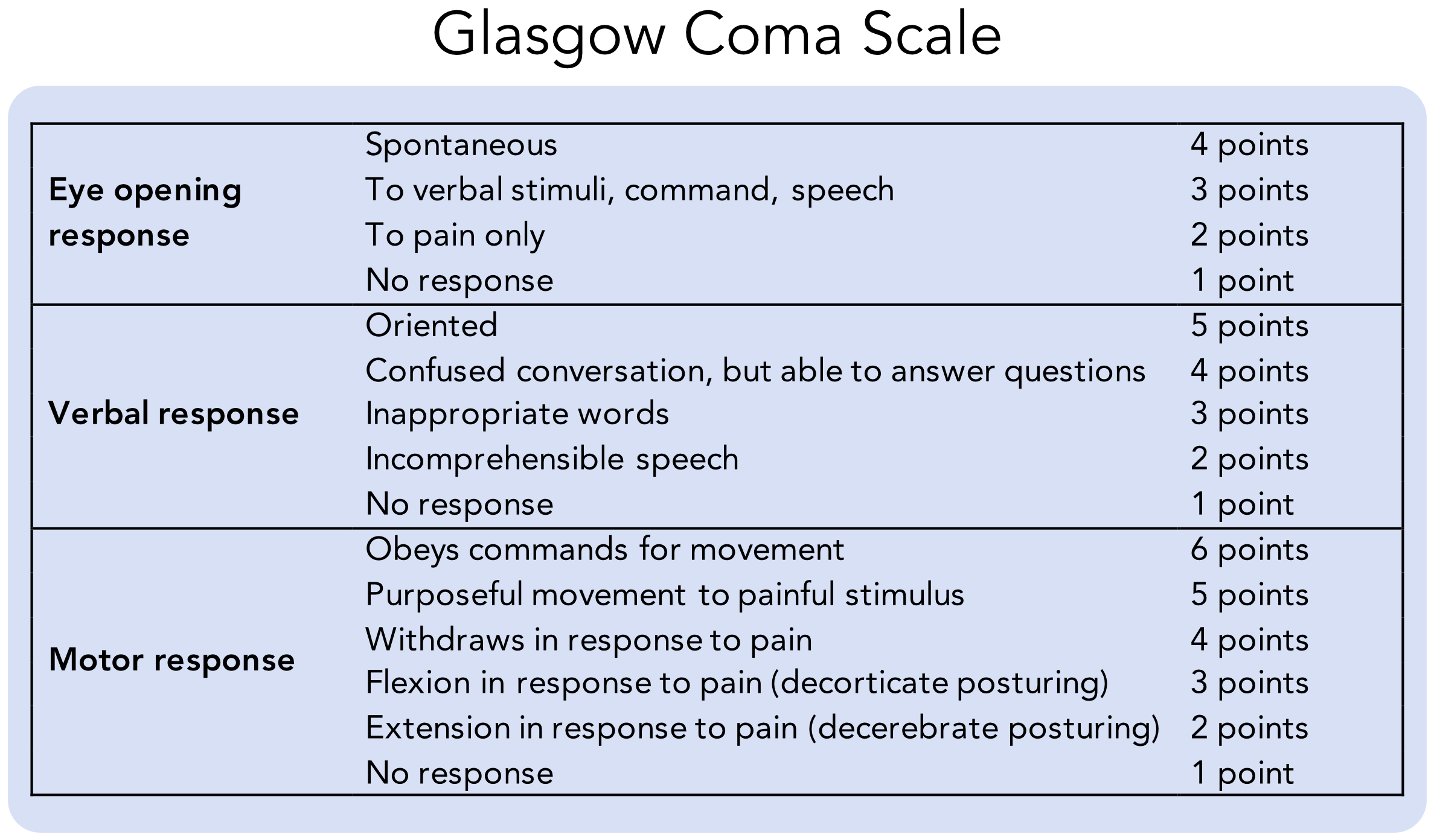
Eye Opening Response
Verbal Response
Motor Response
Localizing Pain
Withdrawal From Pain
Decorticate Posturing
Decerebrate Posturing
Clinicians also need to check the pupils during the physical assessment. The PERRLA test is used to examine the pupils. PERRLA stands for: The clinician tests light reactivity by shining a light in the patient’s eyes. The patient should look directly at the clinician’s nose, so the light doesn’t blind them. The clinician is looking for bilateral constriction. Next, the clinician will ask the patient to focus on something very close, for example, a pen. Then, the clinician will ask the patient to focus on something in the distance, like a clock on the wall. When the patient’s focus shifts to the distant object, their pupils should dilate as their eyes accommodate. The clinician will check the patient’s pupil size to determine if they are equal. After establishing the patient’s pupils are round and equal, the clinician assigns a size. The average person’s pupils will be 2–3 mm on the pupil size chart. On the chart, one mm indicates extremely small pupils, while anything larger than four mm is extremely dilated. In the case of dilated pupils, the patient may have had some medication or drug that has caused it. By checking PERRLA and pupil size, the clinician has already addressed cranial nerves number II and III. Cranial number II is the optic nerve that controls vision and visual acuity. Cranial nerve number III controls pupil constriction and dilation. The cranial nerves connect the brain to the head, neck, and body.Pupils
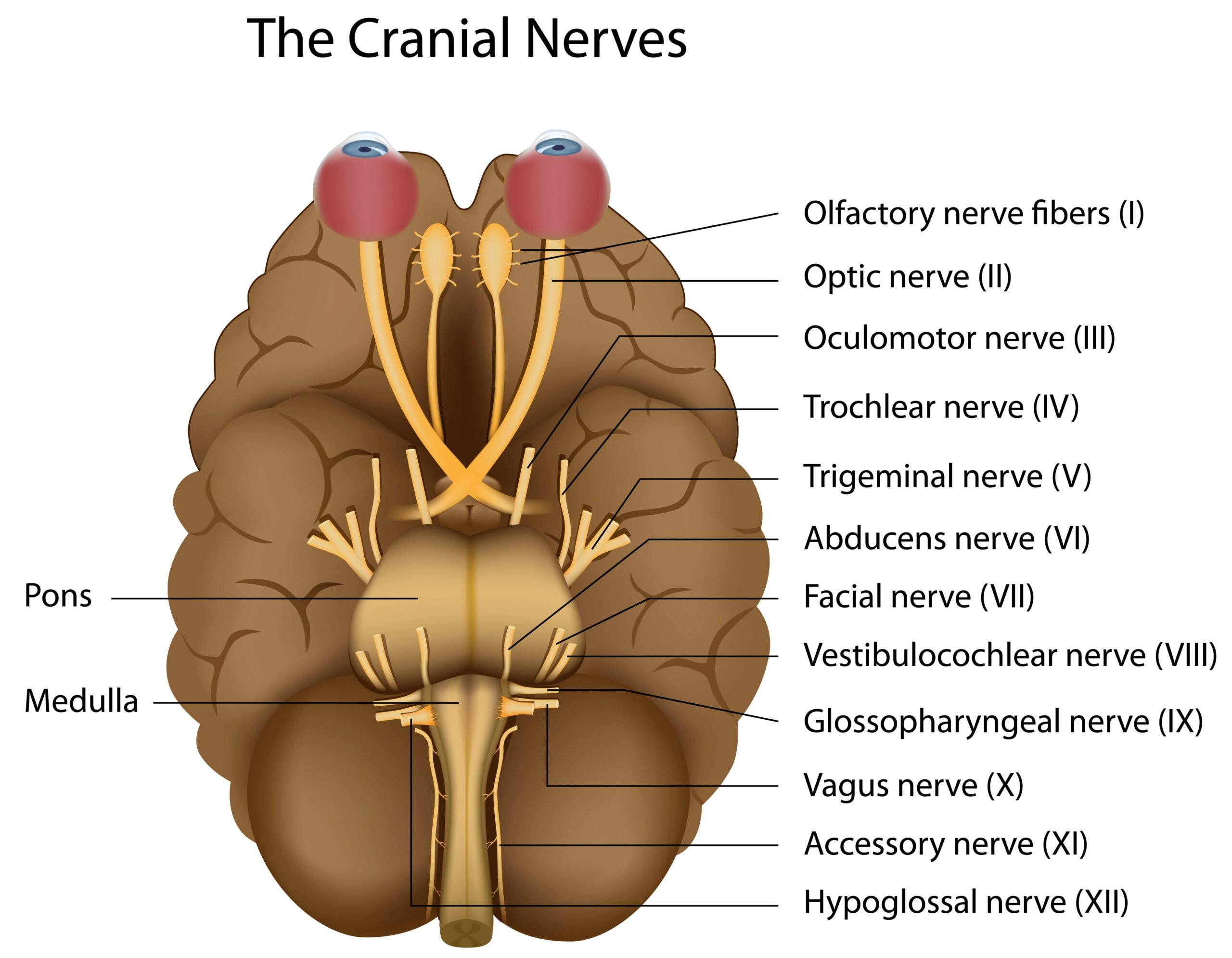
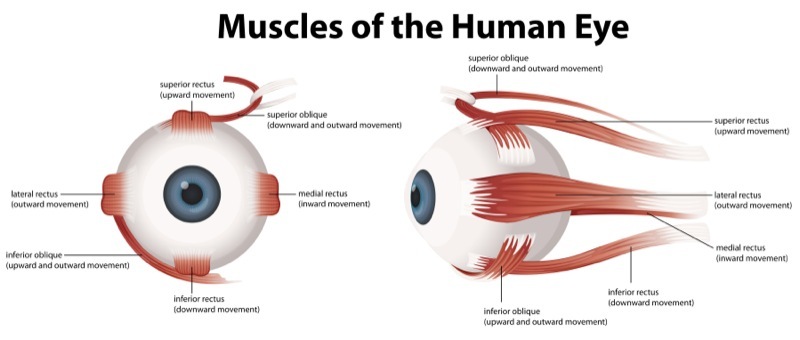
Extraocular movements (EOMs) are assessed using the six cardinal fields of gaze. The six cardinal fields of gaze confirm extraocular movement. Have the patient follow a pen through the six cardinal fields of gaze. If the patient can follow the pen without nystagmus, the clinician will chart that EOS is intact. However, if the patient starts following the pen and the clinician sees their eyes wiggle, nystagmus is noted. That is a negative response, and the clinician must make a note. After the EOS test, a clinician has now checked cranial nerves III, IV, and VI.Extraocular Movements
Related Video – Understanding the Pathophysiology of Increased Intracranial Pressure
Finally, the clinician checks grips and strength. The patient squeezes a clinician’s hand, and the clinician assigns them a number. The strength itself doesn’t matter. It’s only important that the grips are equal in both hands. Testing leg strength is similar. The clinician has the patient push with their legs against the clinician’s hands and assesses for equality of strength. If the patient’s legs are equally weak, it’s not a neurological problem but a muscular problem. Yet, if one leg or arm is much stronger than the other, it could indicate a neurological problem, such as a stroke.Grips and Strength
This has been a quick overview of the neurological assessment. The clinician will utilize this information every time they assess a patient. During a focused assessment, such as after a stroke or other neurological incident, clinicians may perform the neurological assessment more often.Conclusion
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.