Systems of Care: In-Hospital Cardiac Arrest
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- The goal of systems of care is a successful outcome.
- Hospitals utilize two systems of care: in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA).
- Prearrest emergency response systems help clinicians earlier recognize and treat pre-cardiac arrest conditions.
- Systems of care should provide continuous, quality improvement.
- Post-cardiac arrest syndrome is treated in the post-cardiac arrest phase, increasing the likelihood of survival and discharge with optimal neurologic function.
Systems of care (SOC) is a framework for linking the interdependent components of the resuscitation system of healthcare institutions.1 It identifies the strengths and weaknesses of current protocol to make improvements. SOC should increase the probability of successful resuscitation.
Systems of Care Taxonomy
A system of care must have structure, including competent personnel, proper equipment, and necessary training and education, to create processes. The structure involves producing programs, organizations, and cultures to achieve optimal patient outcomes, strengthening the quality of healthcare delivery systems.
The structure, processes, and systems are continuously improved based on data gathered from the institution’s outcomes, experiences, advances in technology, and latest resuscitation research.
In-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA) are two aspects of a SOC. They revolve around the adult chain of survival.2
American Heart Association (AHA) guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC) provide system-specific chains of survival for IHCA and OHCA.
IHCA Chains of Survival
OHCA Chains of Survival
IHCA patients require instant access to additional trained hospital personnel. The first link in the IHCA chain of survival is a magnifying glass, representing the availability of effective surveillance and cardiac monitoring systems to avoid IHCA.
The telephone represents the cardiac arrest emergency response team, involving trained advanced cardiac life support (ACLS) providers such as doctors, nurses, respiratory therapists, and others. Hospitals must implement accessible and efficient methods of activating the emergency response team.
After notifying the team, clinicians administer high-quality CPR, rapid defibrillation, and ACLS support with post-cardiac arrest care, represented via the hand, heart, and hospital bed. The final step in the IHCA is a multidisciplinary plan for recovery and rehabilitation after discharge from the inpatient hospital stay.
OHCA is more challenging due to the lack of trained personnel and limited space for ACLS equipment. OHCA depends on community training instead of healthcare workers. A trained lay rescuer must recognize and perform the appropriate steps when there is a cardiac arrest outside the hospital setting, represented by the telephone and hands.
Rapid defibrillation is also recommended if an automated external defibrillator (AED) is available, represented by a heart on the chains of survival. When emergency medical services arrive, they take over the rescue sequence, as seen by the ambulance.
EMS delivers the patient to the appropriate healthcare institution, so they can undergo further treatment such as cardiac catheterization or ICU admission. That is represented by the hospital bed. The final step in the OHCA is a multidisciplinary plan for recovery and rehabilitation after discharge from the inpatient hospital stay.
Ideally, all bystanders will know how to perform high-quality CPR and immediate defibrillation, increasing the patient’s chances of survival.
Clinicians also implement SOC in situations such as regional trauma, stroke, and ST-segment elevation myocardial infarction.
The community, EMS, and hospital systems are interlinked. The hospital is the final destination.
Respiratory failure and circulatory shock cause most IHCA incidences. Prompt treatment requires early recognition of respiratory distress, signs of shock, and neurologic deterioration. Clinicians typically admit IHCA patients to a highly monitored intensive care setting. According to the AHA’s “Get With The Guidelines” program, there has been a 4–8% increase in survival rate amongst in-hospital CPR patients over the years. Improvement strategies also play an important role in preventing cardiac arrest and increasing survival rates. According to AHA data, 19% of in-hospital CPR occurred in unmonitored general wards, compared to 48% in the intensive care units (ICU) and 18% in the emergency departments (ED). Most hospitals provide teams and optimized SOC for patients in the ICU and ED.3 There are still gaps in healthcare SOC. Studies show a decrease in resuscitation outcomes during the nighttime, weekends, and holidays. Lower-income patients also have lower survival rates after IHCA. Read: General Stroke CareSystems of Care: In-Hospital Cardiac Arrest
The following details the pre-arrest rapid response systems. Hypovolemic shock and respiratory failure are the most common IHCA causes. These patients present with tachypnea, tachycardia, and hypotension. Cardiac arrest commonly occurs in non-specialized hospital wards, such as general surgical or medical wards. It’s likely due to the lack of monitoring equipment and specialized personnel. Studies show personnel in the medical and surgical wards don’t report abnormal or critical vital signs in 10% of patients. Critical care areas have a higher nurse-to-patient ratio and specialized monitoring equipment. Frequent monitoring is possible and clinicians quickly recognize the first signs of instability. Monitoring strategies must be advanced via more accessible advanced monitoring equipment. Quick assessment tools may also be utilized to clinically monitor patients for early warning signs of cardiac arrest, such as the national early warning score and early warning sign system. The rapid response team (RRT) and the medical emergency team (MET) intervene in IHCA patient care. They’re composed of physicians, nurses, and respiratory therapists. They’re available around the clock and are equipped with advanced tools for monitoring and resuscitation. RRTs and METs reduce cardiac arrest incidence, especially in general wards. Early Warning Sign Systems (EWSS) are scorecards grading the severity of a patient’s critical condition, reducing incidences of cardiac arrest. They require mandatory actions based on the scoring and are displayed for easy nurse access. When a critical patient is treated, the RRTs and METs perform continuous assessment until the patient is stabilized. If the patient is not improving or has a high risk of IHCA, they are transferred to the ICU for close monitoring. Studies show if critically ill patients are not promptly transferred to the ICU, they have a high chance of mortality. Continuous assessment prevents further deterioration to cardiac arrest.4 Some situations require clinicians to allow the natural process of death, such as when a medically insurmountable condition prevents life or a good quality of living. In such cases, RRTs focus on palliative care after obtaining advanced directives and do not resuscitate orders. Clinicians must seek family input regarding aggressive resuscitation measures if it wasn’t discussed before the event.Pre-Arrest Rapid Response Systems
1. Recognition of Patients at Risk for Cardiac Arrest
Related Video – Hs and Ts – Hypovolemia
2. Rapid Response Teams, Medical Emergency Teams, and Early Warning Sign Systems
Related Video – Acute Coronary Syndrome – Emergency Medical Services
3. Continuous Assessment
4. Do not Resuscitate and Palliative Care
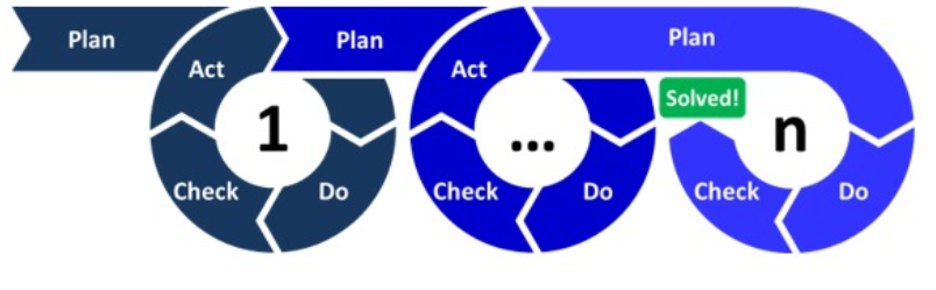
To continually improve, resuscitation teams must optimize their teams, equipment, and processes. Teams collaborate to identify possible problems, plan the next steps to improve performance, and practice frequently. Teams that perform effective and well-choreographed ACLS, high-quality CPR, effective ventilation, and early defibrillation see excellent outcomes. Continuous quality improvement involves measuring key performance indices, comparing and analyzing data, and creating new interventions to improve outcomes. A common tool for continuous improvement is the “PLAN-DO-CHECK-ACT” model. Plan-Do-Check-ActContinuous Quality Improvement
The most common way to call the RRT or MET teams is via the hospital’s public address system. Additionally, hospitals should implement policies which improve the team’s timing.Activating the IHCA SOC
Resuscitation teams perform their best if each member: There are several crisis resource management principles. Clinicians and institutions must:Crisis Resource Management
Resuscitation team personnel have adequate training and retraining skills to minimize errors and optimize patient outcomes.5 The team is composed of physicians, nurses, and trained ancillary healthcare workers such as respiratory therapists and pharmacists. Some institutions utilize other personnel such as security guards, clergy members, and social workers. Each team member frequently practices resuscitation procedures, including just-in-time or just-in-place training. Just-in-time training may involve a simplified training session for basic life support on a mannequin. Other training involves an interdisciplinary ACLS approach, utilizing face-to-face lectures and hands-on simulations. It’s supervised by an expert physician certified by the AHA or another recognized body.The Resuscitation Team
The ALERT program teaches early identification and rapid intervention for pre-arrest patients. It trains personnel to prevent further deterioration of critically ill patients, even if early interventions were already performed. Studies show this course of action reduces the number of patients with IHCA and improves rates of survival to hospital discharge. The system is continuous and interval training updates are required. This training requires face-to-face lectures and simulations. It is designed around individual wards of the hospital, increasing familiarization and improving team effectiveness whenever they respond to cardiac arrest. The course encourages participants to be proactive in identifying where they can reflect and improve on their actions.Acute Life-Threatening Events Recognition and Treatment (ALERT) Program
Debriefing encourages continuous improvement of the resuscitation team. The hot debriefing is conducted right after a resuscitation effort, so team members’ memories are still fresh. Some challenges may occur, such as when physicians and nurses are unavailable because they’re administering post-cardiac-arrest care. Team members may also have a difficult time narrating information regarding the events that took place, particularly if the resuscitation did not end well. The cold debriefing is performed later (several hours to a few days), allowing team members time to reflect and prepare. Plus, all team members can be present for the activity. Other experts may be invited to conduct a multidisciplinary assessment of the situation.Debriefing
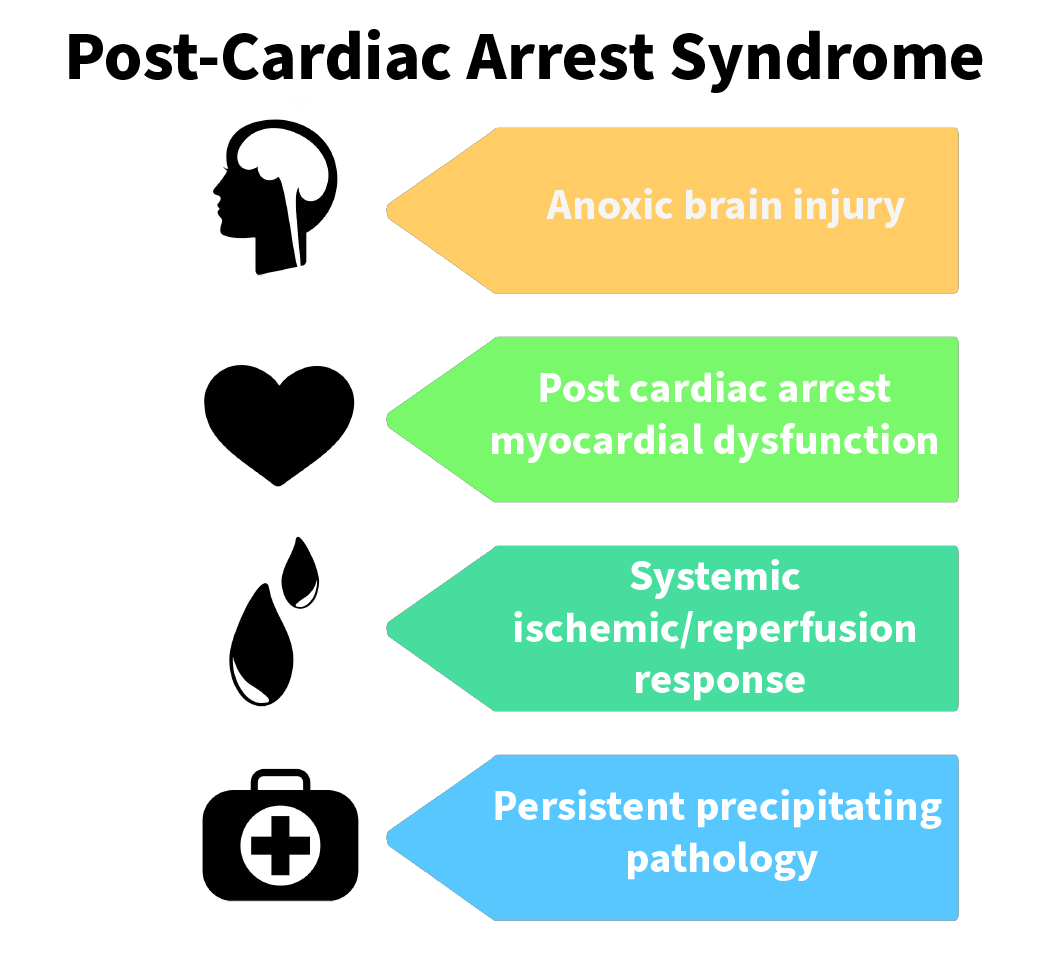
When the patient achieves a return of spontaneous circulation (ROSC) after cardiac arrest, clinicians start post-cardiac arrest care. Cardiac arrest patients usually present with complications affecting the normal pathophysiologic process, known as post-cardiac arrest syndrome, a factor in patient mortality. These patients have a 32% to 54% IHCA survival rate when they achieve ROSC.6 Post-cardiac arrest care optimizes the patient’s hemodynamics, treatment of precipitating factors, and targeted temperature management with the goal of addressing the effects of post-cardiac arrest syndrome. It’s recommended that clinicians refer these patients to a multidisciplinary team of specialists. If a hospital is not equipped to provide these services, its SOC should address the seamless transfer to more specialized institutions. Complications after a cardiac arrest are known as post-cardiac arrest syndrome.Post-Cardiac Arrest Care
All hospitals have two systems of care, IHCA and OHCA. OHCA may require laypeople to perform proper cardiac monitoring and procedures before EMS arrival. SOC should provide continuous, quality improvement. There are several training programs for IHCA and OHCS, improving effectiveness and patient mortality rates.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. American Heart Association. Systems of Care. 2020.
2. American Heart Association. Highlights of the 2020 AHA Guidelines Update for CPR and ECC. 2020.
3. Steven L. Kronick, Michael C. Kurz, Steve Lin, Dana P. Edelson, Robert A. Berg, John E. Billi, Jose G. Cabanas, David C. Cone, Deborah B. Diercks, James (Jim) Foster. Systems of Care and Continuous Quality Improvement. American Heart Association. 2015.
4. Matthew M Churpek, MD, MPH, PhD, Blair Wendlandt, MD, Frank J Zadravecz, MPH, Richa Adhikari, MPH, Christopher Winslow, MD, and Dana P Edelson, MD, MS. Association Between ICU Transfer Delay and Hospital Mortality: A Multicenter Investigation. National Library of Medicine. 2017.
5. Ulmer C, Miller Wolman D. System Strategies to Improve Patient Safety and Error Prevention. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. 2009.
6. Kelly N. Sawyer, Teresa R. Camp-Rogers, Pavitra Kotini-Shah, Marina Del Rios, Michelle R. Gossip, Vivek K. Moitra, Kirstie L. Haywood, Cynthia M. Dougherty, Steven A. Lubitz. Sudden Cardiac Arrest Survivorship: A Scientific Statement From the American Heart Association. American Heart Association. 2020.