Systems of Care: Out-Of-Hospital Cardiac Arrest
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Table of Contents
- Communities Combating Cardiac Arrest
- Community Involvement in OHCA
- Public Safety Answering Point and Emergency Medical Services
- Dispatcher Recognition of Cardiac Arrest
- Dispatcher Instruction in CPR
- Social Media’s Role in Summoning Rescuers
- OHCA Quality Metrics and EMS Transition to Hospital
- Continuous Quality Improvement
- Summary
Article at a Glance
- Community involvement is a crucial part of increasing survival rates in out-of-hospital cardiac arrest.
- EMS dispatchers should coach lay rescuers to provide high-quality compression-only CPR, which is often the difference between life and death for cardiac arrest patients.
- Social media may aid rescuer response in an out-of-hospital cardiac arrest, decreasing time to first compression.
- Continuous quality improvement is required to effect meaningful systems of care change.
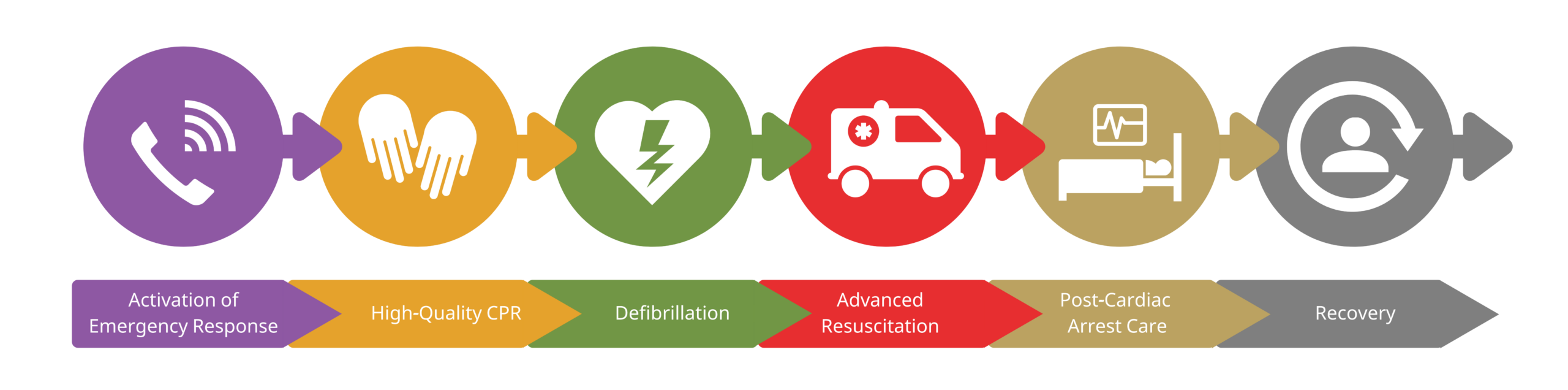
World wide, out-of-hospital cardiac arrest (OHCA) has an incidence rate between 30 to 97 people per 100,000 people.1 Communities must play a greater role in the fight against OHCA. Local government leaders and non-governmental organizations should train lay persons to provide bystander CPR and early defibrillation as soon as the cardiac event takes place, increasing resuscitation success rates. OHCA Chain of SurvivalCommunities Combating Cardiac Arrest
The community is a valuable stakeholder vested in the interests of people experiencing cardiac arrest. Clinicians can teach bystander CPR to everyone, including children. With limited access to equipment, a layperson can still provide highly effective, hands-only CPR. Clinicians should administer traditional face-to-face CPR instruction, though self-instruction media may be acceptable depending on the participant’s requirements. Some governmental policies have approved training of high school students, volunteer members of the community, and caregivers in the public school setting or other large community venues. Public access defibrillator initiatives provide instructional courses on AED uses. Federal and local governments have enacted laws placing AEDs in municipal buildings and areas where there are mass gatherings, such as airports and schools. Local initiatives also place AEDs in public swimming pools, arenas, town halls, golf courses, and other local venues. Defibrillators are available in most public spaces. Cardiac arrest patients in private residences are not likely to receive CPR as quickly. Some efforts to improve these statistics include training emergency dispatch services in real-time instruction on confirming cardiac arrest and performing compression-only CPR.2Community Involvement in OHCA

The public safety answering point (PSAP) is a 24-hour call center, serving as an interface between emergency medical services (EMS) and the general public. 9-1-1 is the most common PSAP. Trained community members recognize cardiac arrest and immediately activate the PSAP. Dispatchers send EMS to assist lay rescuers. Emergency dispatchers may also help the bystander intervene in other life-threatening conditions such as acute coronary syndrome, trauma, or stroke. Studies show reducing time to first compression via dispatcher-assisted CPR improves outcomes. A dispatcher sends emergency medical services (EMS) to assist lay rescuers.Public Safety Answering Point and Emergency Medical Services

Related Video – What is Stroke Volume?
It’s important that dispatchers diagnose cardiac arrest over the phone even when the dispatcher is not present at the scene. They must communicate effectively and ask the correct questions. PSAPs develop scripts to assist dispatchers in detecting OHCA. Studies show scripts have a 99% accuracy rate of diagnosing cardiac arrest.3 An important clinical sign the bystander relays to the emergency dispatcher is the presence of abnormal breathing or agonal gasps. Once detected, the emergency dispatcher may instruct the bystander in performing dispatcher-guided CPR.Dispatcher Recognition of Cardiac Arrest
Dispatcher-instructed CPR increases survival rates by 2.4%. No evidence proves dispatcher-instructed CPR improves neurologic outcomes or return of spontaneous circulation (ROSC).4 American Heart Association guidelines recommend dispatchers provide compression-only CPR instructions to callers for adults with OHCA.Dispatcher Instruction in CPR
Community SOC include phone calls, SMS text messaging, and social media to alert emergency dispatchers of OHCA situations. Social media companies embed messaging services as a gateway to reaching dispatchers and volunteer lay responders. OHCA patients require instant access to bystander-initiated CPR. Social media can fill this gap by sending the closest trained lay rescuers to the scene. The lay rescuer’s proximity to the cardiac event is necessary and lifesaving. Read: ACS and STEMI Systems of CareSocial Media’s Role in Summoning Rescuers
Data collection and utilization are necessary for quality improvement initiatives. The Utstein resuscitation registry templates for OHCA is a data-capturing tool organizations implement in SOC policies. The standardized template incorporates core elements of resuscitation performance for OHCA, community response times, EMS treatment accuracy, and hospital SOC. Other data, such as 12-lead ECG and CPR quality measurement, are also available. High-quality CPR performance improves when clinicians know they are constantly evaluated for their performance, as skills are reinforced in basic arrhythmia certification training. Metrics measuring CPR effectiveness include chest compression fraction, chest compression quality (compression depth, compression rate, and allowance of full chest recoil after each compression), and ventilation rate. Rescuer feedback helps them understand their CPR-providing abilities and areas of improvement. EMS provides ACLS to OHCA patients transferring to a hospital. ACLS involves advanced cardiac monitoring, 12-lead ECG, defibrillation or cardioversion, vascular access, pharmacologic interventions, and advanced airway implementation and care. Once ROSC is achieved, ACLS providers begin comprehensive post-resuscitation care, including hemodynamic and oxygenation optimization with volume-limiting ventilation, as well as targeted temperature management.OHCA Quality Metrics and EMS Transition to Hospital
Related Video – Systems of Care: In-Hospital Cardiac Arrest
Bystander CPR, CPR quality, early defibrillation, rapid response systems, and post-cardiac arrest care are focus areas for continuous quality improvement. High-performing systems improve resuscitation success rates. An effective system of care benefits the public if stakeholders focus on clarity, discipline, and engagement to further improve policies and procedures. It involves goal setting, a process-centric focus, data gathering, and accountability. Goal setting defines what the SOC must achieve. An entity (person or a system) must be held accountable for the success or failure of these goals. They’re aligned with key performance indicators based on the change expected and achievement date. For example, in 2010 the AHA set a goal of doubling of survival from cardiac arrest survival between 2010 and 2020 from 19%–38% for IHCA and 7.9–15% for OHCA.55 Stakeholders should pay attention to four principles when goal setting. They must focus on the important, act on lead measures, keep a compelling scoreboard, and create a cadence of accountability.66 SOC should focus on one or two important goals to ensure success. An example goal is “doubling the number of states with CPR/AED training as a high school graduation requirement.” Various tools guide stakeholders through continuous policy improvement. The Lean tool transforms waste into customer value, the Six Sigma tool decreases errors, and the Plan-Do-Check-Act tool monitors for continuous small improvement iterations. Stakeholders must agree on a framework. They identify a priority problem, gather all data pertaining to the problem, and formulate a root-cause analysis. After identifying the problem, the team analyzes it to develop a solution. The solution is either implemented immediately or as part of a pilot-testing protocol, so it can be assessed for successes and failures. If successful, it will be implemented as part of the new SOC. It’s a continuous cycle. One problem is solved and another is identified. Data gathering is integral to goal setting and effecting change. Data represents the structure, processes, and outcomes in OHCA resuscitation performance. The Utstein Standardized Template for Reporting Outcomes is a data-gathering tool. Data registries also collaborate with AHA programs such as Get With The Guidelines-Resuscitation and the Cardiac Arrest Registry to Enhance Survival. Performance feedback for clinicians helps them improve. They’re held accountable for the success or failure of their performance. Accountability is important in creating positive changes within SOC. For OHCA, the community is accountable. For hospitals, accountable entities are the senior executives, chief quality assurance officers, nursing officers, and medical officers.Continuous Quality Improvement
Goal Setting
Effecting Change
Measurement
Accountability
It is crucial that communities are involved with OHCA patients. EMS dispatchers should train lay rescuers to provide CPR. Social media is a crucial component of community OHCA awareness and may raise rescuer response time, saving the patient. Meaningful SOC requires continuous quality improvement.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Kiguchi T, Okubo M, Nishiyama C, et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. 2020.
2. Hidetada Fukushima and Francesco Bolstad. Telephone CPR: Current Status, Challenges, and Future Perspectives. Open Access Emergency Medicine. 2020.
3. Greif R, Bhanji F, Bigham BL. Education, implementation, and teams: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2020.
4. Kristine Elisabeth Eberhard, Gitte Linderoth, Mads Christian Tofte Gregers, Freddy Lippert, and Fredrik Folke. Impact of dispatcher-assisted cardiopulmonary resuscitation on neurologically intact survival in out-of-hospital cardiac arrest: a systematic review. Scandinavian Journal of Trauma, Resuscitation, and Emergency Medicine. 2021.
5. Pasupula DK, Bhat A, Siddappa Malleshappa SK, et al. Impact of change in 2010 American Heart Association cardiopulmonary resuscitation guidelines on survival after out-of-hospital cardiac arrest in the United States: An analysis from 2006 to 2015: An analysis from 2006 to 2015. Circ Arrhythm Electrophysiol. 2020.
6. McChesney, Chris. 4 Disciplines of Execution. Simon & Schuster. 2012.

