What is Transcutaneous Pacing?
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
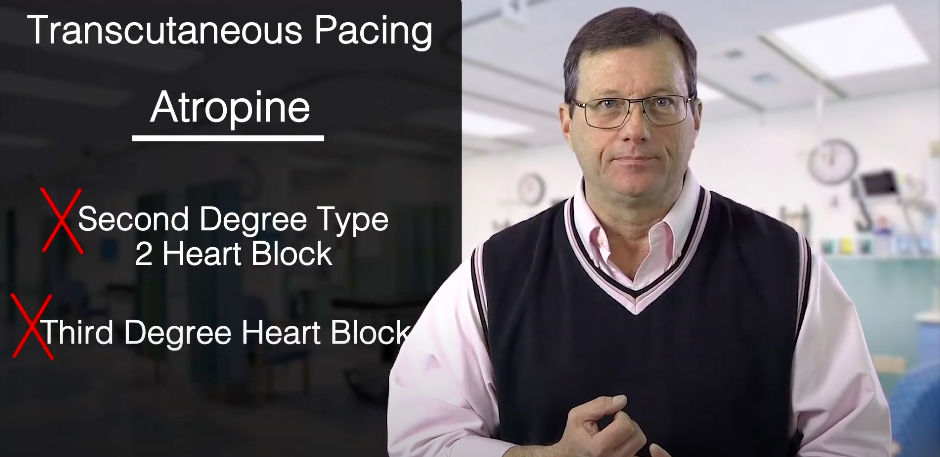
- Transcutaneous pacing is used during bradycardia when atropine is not effective, particularly in 2nd-degree Type II and 3rd-degree AV blocks.
- The placement of pads is the same as for defibrillation.
- The provider must know how to use the equipment at their facility.
- To use: change monitor to pacing mode, set the rate, and adjust the electrical current until there is a pacer spike on the monitor.
- Always check for a central pulse during pacing.
- The provider should consider sedation before pacing.
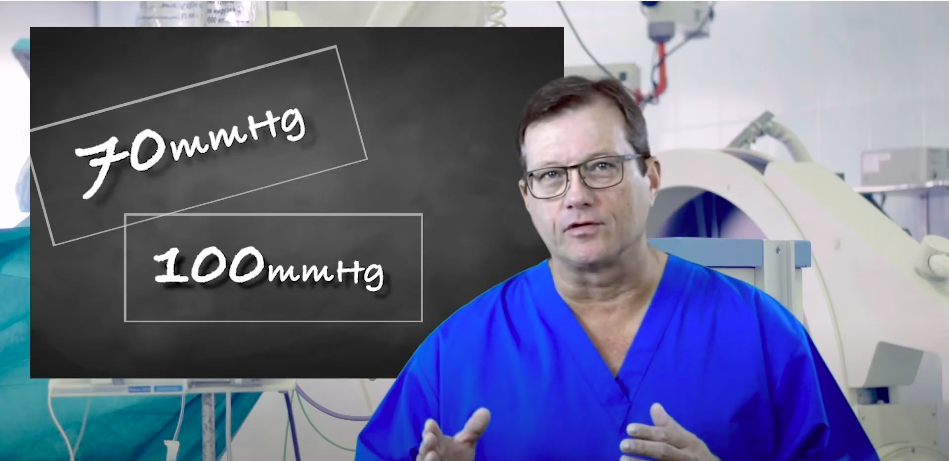
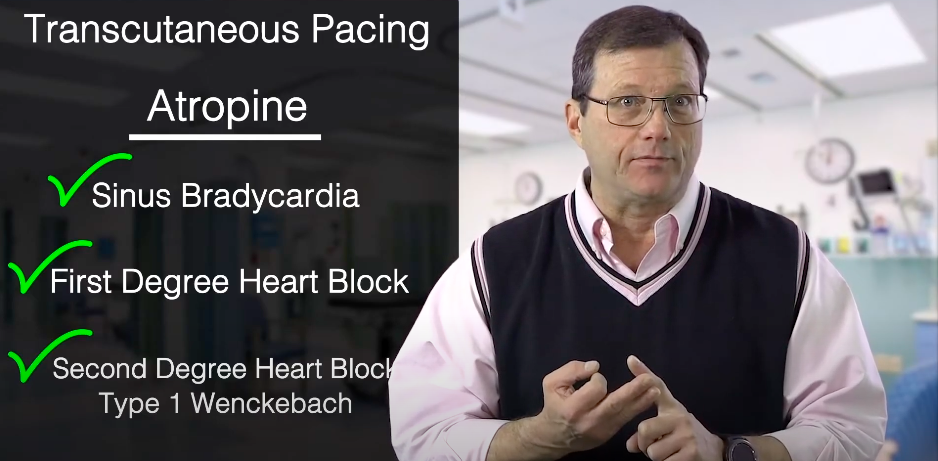
We use transcutaneous pacing on bradycardic patients when atropine is ineffective, which typically occurs in lower blocks. Administer atropine for a sinus bradycardia, sinus with a first-degree heart block, and sinus with a second-degree heart block Type 1 Wenckebach. Atropine can be effective for these blocks. If the block is below those blocks, atropine will likely be ineffective. If a patient is experiencing a second-degree Type II heart block or third-degree heart block, quickly prepare your pacer. Since atropine does not work well for lower heart blocks, turn to transcutaneous pacing.A Quick Review on Transcutaneous Pacing
Related Video – ECG Rhythm Review – Sinus Bradycardia
Related Video – ECG Strip: First-Degree Heart Block
Related Video – One Quick Question: What is Second-Degree Heart Block Type 2?
Related Video – One Quick Question: What are the Third-Degree Complete Heart Block Criteria?
Related Video – One Quick Question: What are the Second-Degree Heart Block Criteria?
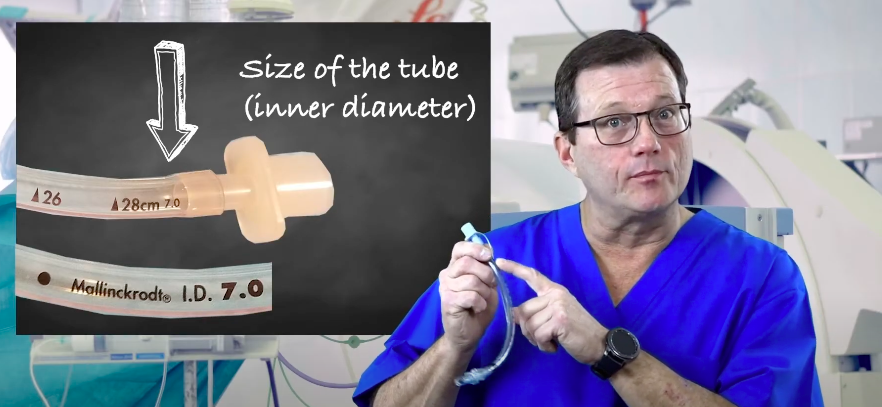
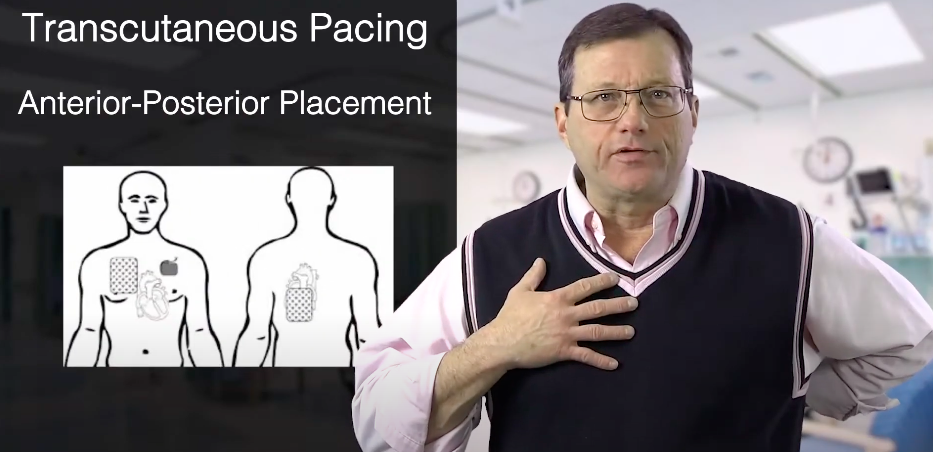
For transcutaneous pacing, place the pads on the patient’s chest and back. This method is called anterior-posterior placement. You may also place the pads anterolaterally, or on the high right and low left of the chest. Anterior-posterior pad placement After applying the pads, make sure the wires are not under the pads. Also, ensure there is no jewelry, medication patches, implanted devices, or anything else underneath the pads or in the way. You need a clear path from one pad, through the heart, to the other pad. Make sure there are no items under the pads or between the pads. Read: What is Synchronized Cardioversion?Pad Placement

Cardiac Monitors
While there are some differences, most cardiac monitors operate similarly. You must know how the equipment works.
Cardiac monitors may look different but work the same.
After pad application, set the monitor to pacing mode. Follow your local protocols to set the rate. A standard pace is 80 ppm.
Next, slowly turn up the milliamps (mA). You’ll see ‘mA’ on the monitor next to the dial. Turn up the milliamps until you see electrical capture on the monitor evidenced by a pacer spike followed by a wide QRS complex. Most importantly, check for mechanical capture to ensure the pacer is generating a pulse.
Related Video – What is ECG Pacing?
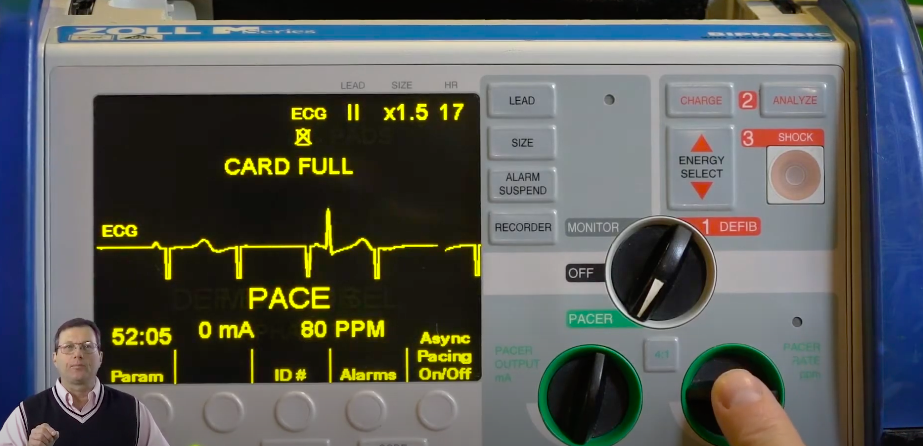
The provider is setting the pacer rate to 80 ppm, and there are currently 0 milliamps.
While pacing, feel for a femoral pulse. You should feel a pulsation coming off of the heart and down through the aorta. Remember, when you check for a pulse, check for a central pulse. It’s not uncommon for a patient to twitch while you’re pacing, so it may be hard to detect a pulse on the periphery.
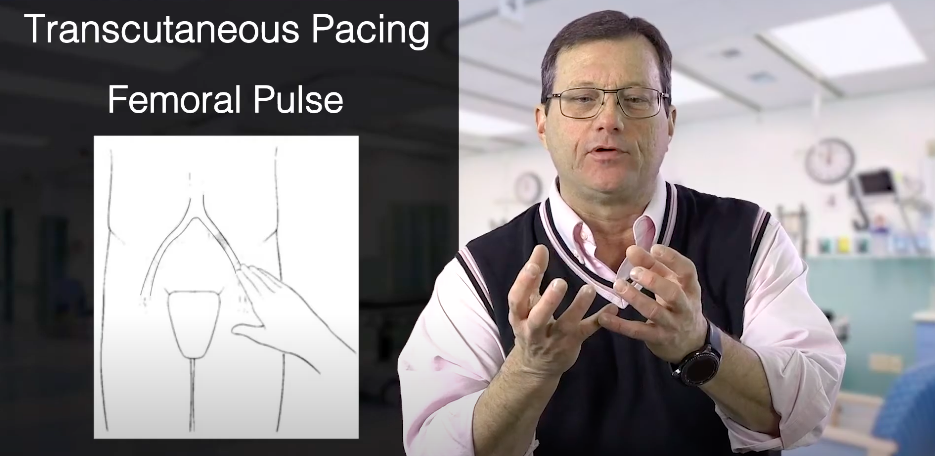
While pacing, find the femoral pulse.
We want to use the least amount of energy necessary to generate a pulse. If the monitor’s milliamps are high, you may want to throttle back and use the least amount of energy necessary to generate a pulse. Also, keep in mind that transcutaneous pacing hurts. You’re electrifying the body to get the heart to beat. Fentanyl might be a nice option because it doesn’t have a lot of hemodynamic effects. Importantly, you have to treat the pain. Your protocol may call for a little midazolam (Versed) or a sedative, which is appropriate. Other Considerations
Transcutaneously pace bradycardic patients if atropine is ineffective. Use either anterior-posterior or anterolateral pad placement. Make sure to set the rate and milliamps on the cardiac monitor and check for a femoral pulse while pacing. Remember to treat the patient’s pain and use a sedative if possible.Summary
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.