Pathophysiology of Increased Intracranial Pressure
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Different etiologies can lead to increased intracranial pressure.
- Some signs and symptoms of increased intracranial pressure are restlessness, headache, nausea and vomiting, and the Cushing triad.
- Read on to learn about the etiology and unique signs and symptoms of increased intracranial pressure in more detail.
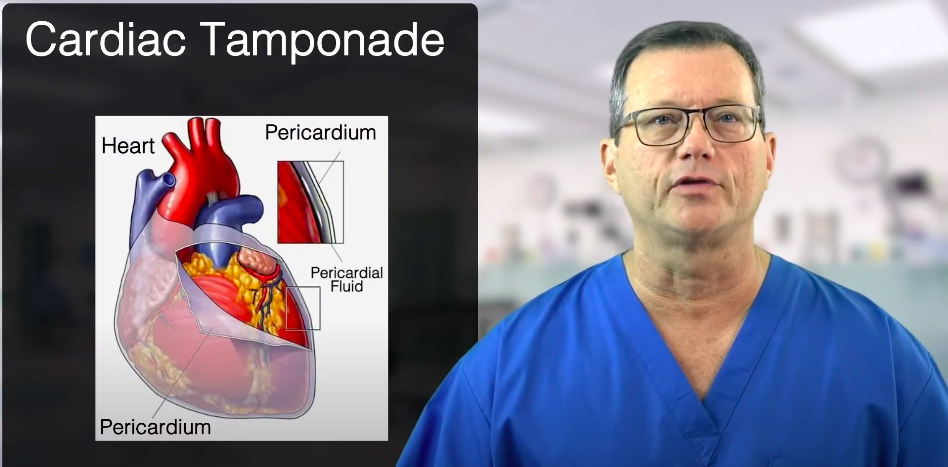
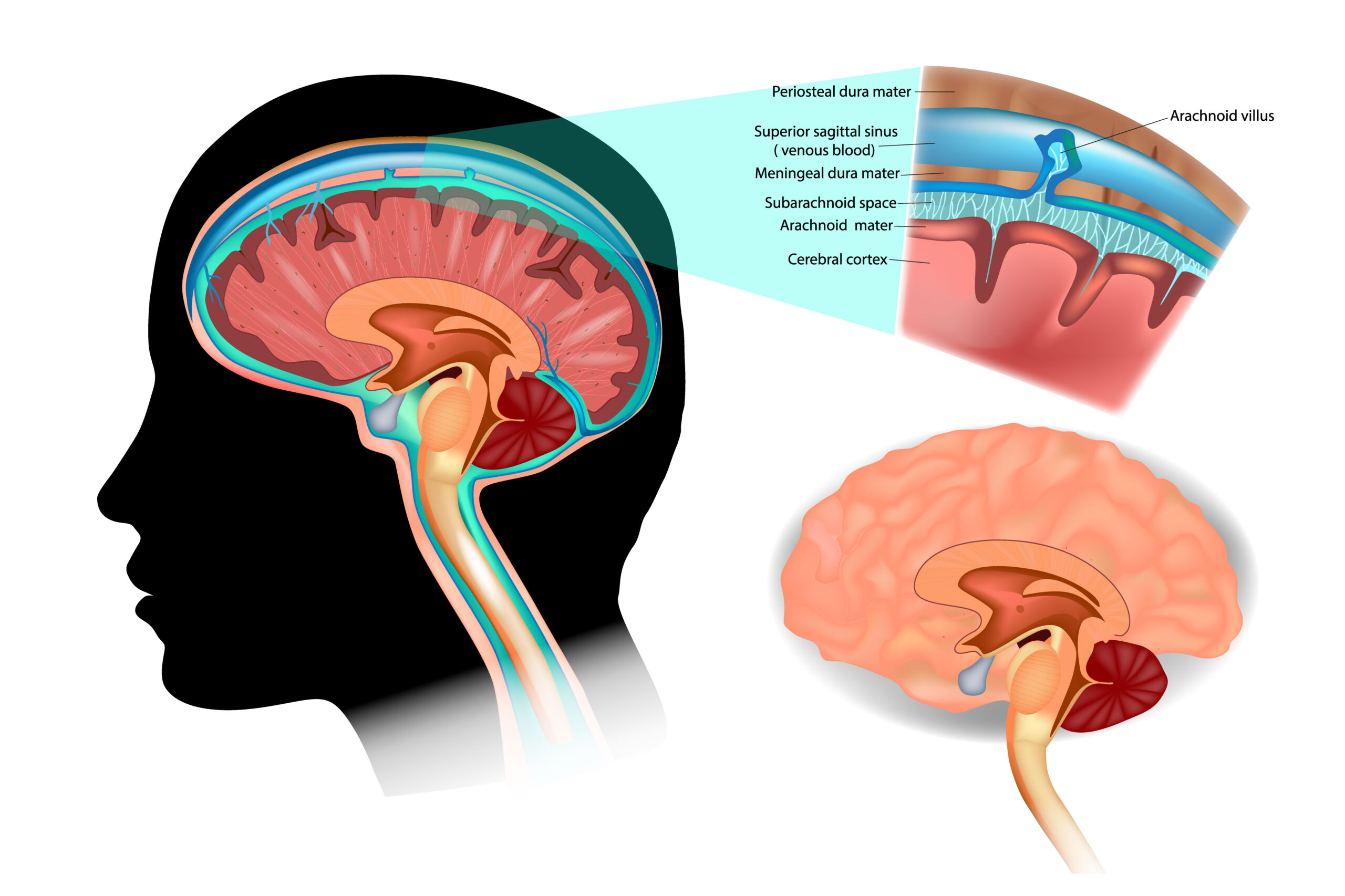
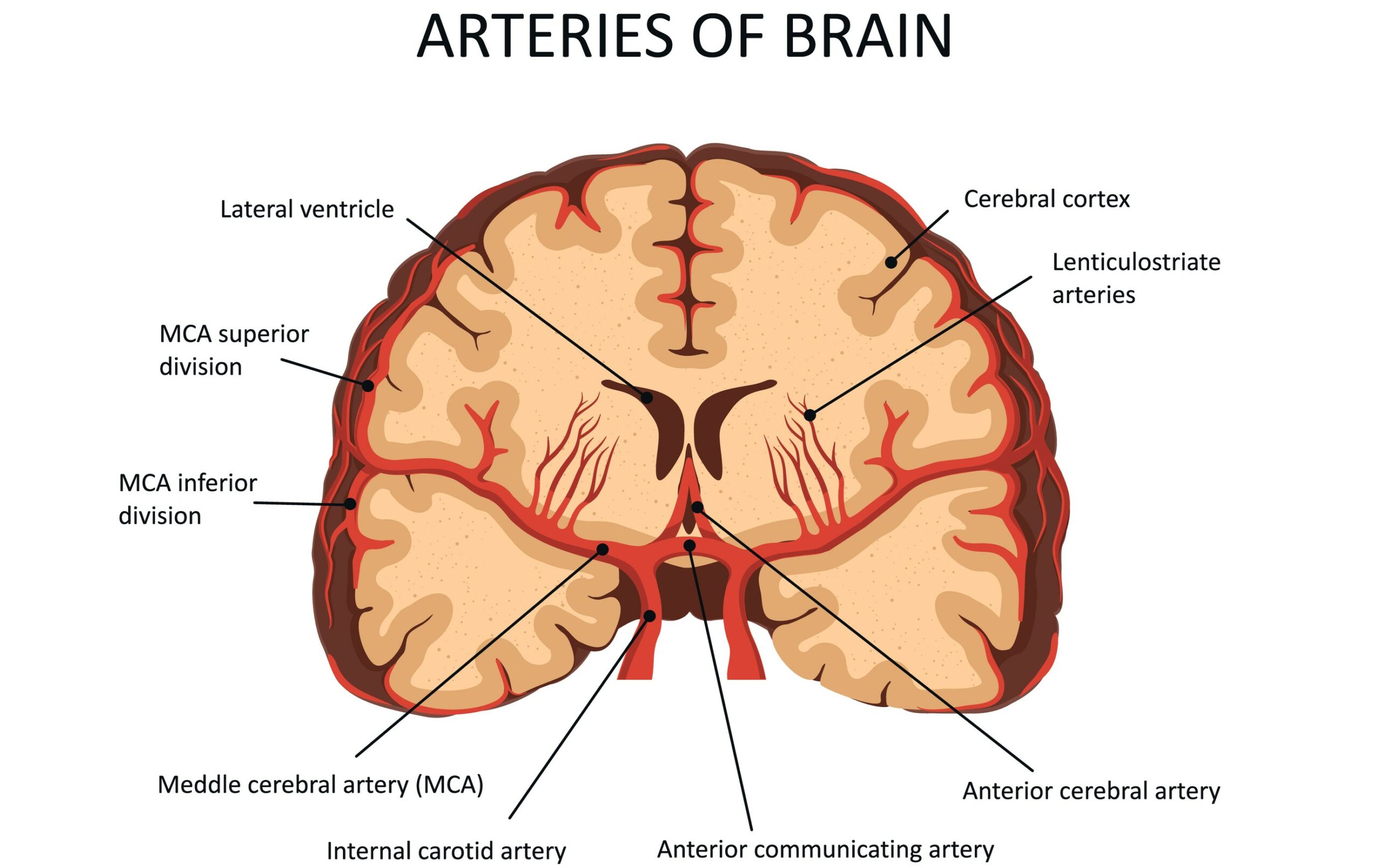
Increased ICP arises from: The CSF, blood, and brain tissue are the three main elements that occupy the skull. If there is an increase in any of these elements, the ICP will increase. Respiratory acidosis can eventually lead to increased intracranial pressure. Changes in these elements occur for different reasons. For example, an increase in CSF is observed in meningitis, an increase in blood or cerebral blood flow is seen during trauma, and an increase in brain tissue is associated with trauma that causes tissue swelling and edema.Intracranial Pressure Etiology
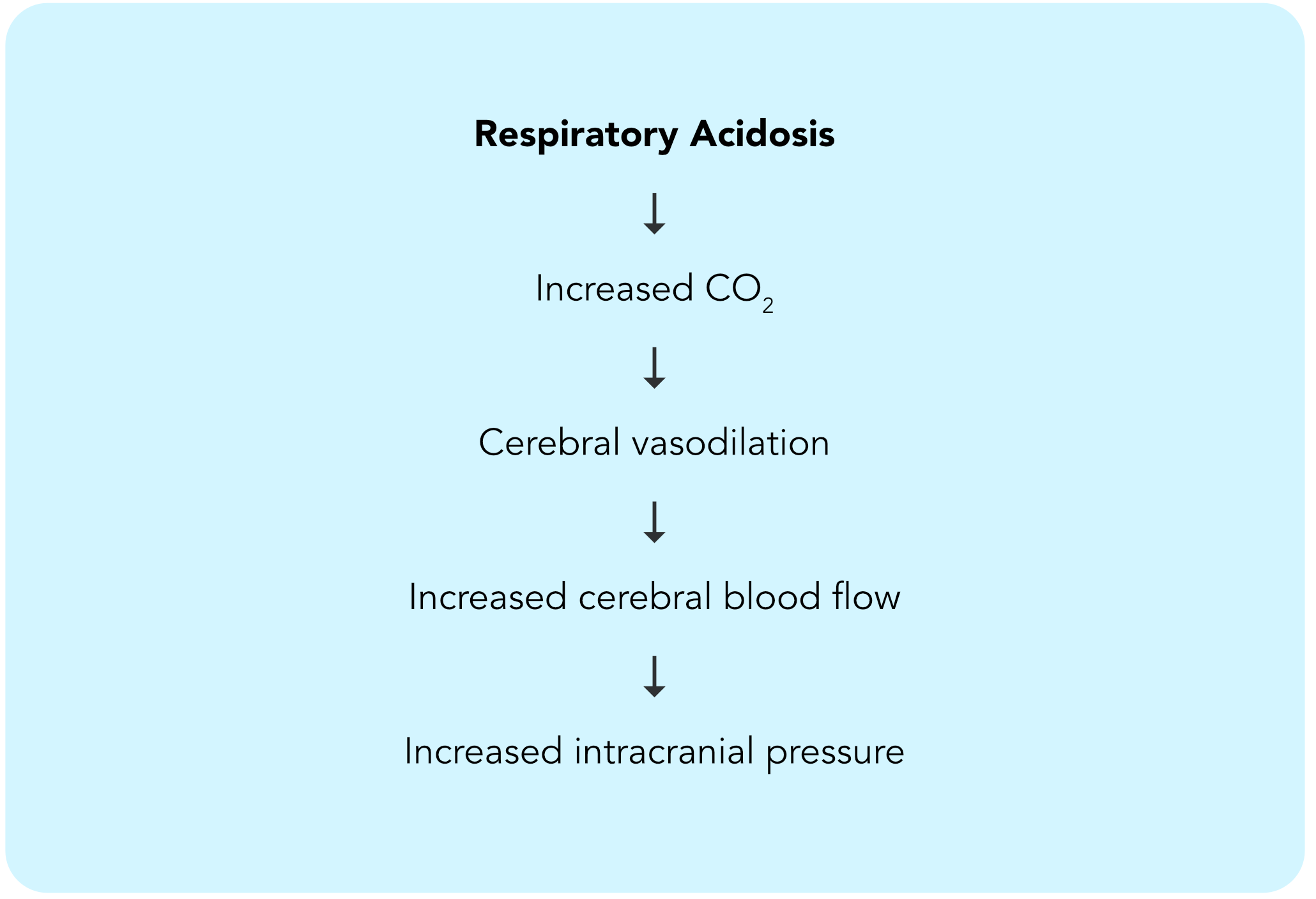
Related Video – What is the Neurological Assessment?
A patient presents with respiratory acidosis. This presentation is fairly common in patients with emphysema and chronic obstructive pulmonary disease (COPD) and occurs when the amount of carbon dioxide (CO2) in the body increases. Because CO2 is a potent vasodilator and readily crosses the blood-brain barrier, the patient may experience neurological changes. When CO2 enters the brain, it causes cerebral vasodilation, which increases cerebral blood flow. The increase in blood flow and amount of blood in the brain leads to increased intracranial pressure. Note: the pathway to increased ICP may differ based on etiology. However, the signs and symptoms will be the same. Respiratory acidosis can eventually lead to increased intracranial pressure. Read: Peripheral Vascular DiseaseA Case to Illustrate Increased ICP
There are both early and late-stage signs and symptoms for increased ICP. It is important for the provider to recognize the early signs and symptoms and correct the underlying etiology. If the underlying etiology is not addressed, it can lead to brainstem herniation. Once the late-stage signs and symptoms present, brainstem herniation is imminent. The early signs and symptoms of ICP are: In the early stages of ICP, the patient may seem “off” after previously being calm, alert, and oriented. They will increasingly become restless and agitated and may report a headache (from pressure on the meninges) or nausea and vomiting (from pressure on the medulla — the vomiting center of the brain).What Are the Signs and Symptoms?
Related Video – Neurogenic Shock Versus Spinal Shock
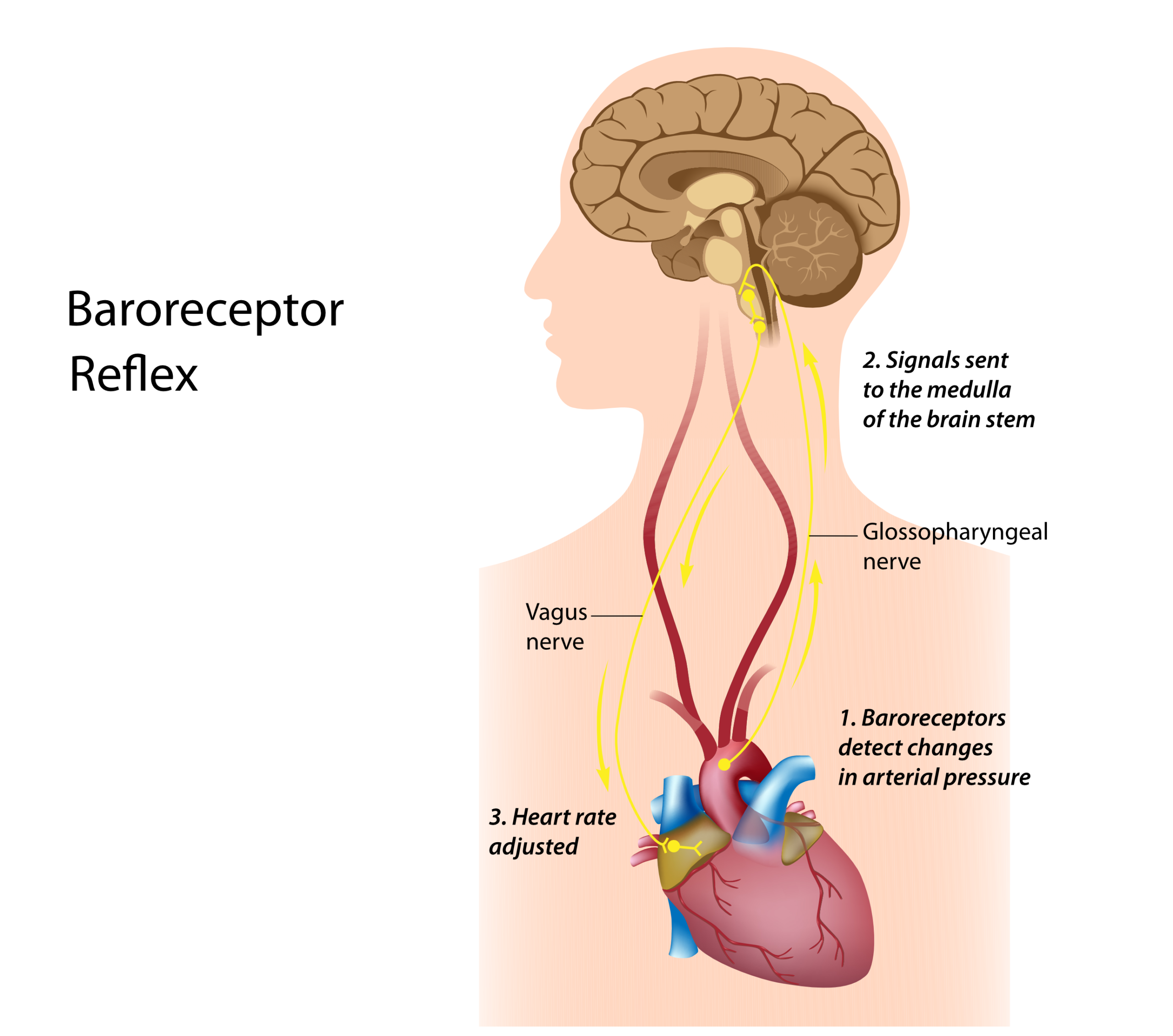
The Cushing triad is a late but also unique presentation of symptoms caused by increased ICP. The Cushing triad includes an increase in the systolic blood pressure, a decrease in the heart rate (bradycardia), and a decrease in the respiratory rate. It is important to understand why the symptoms within the triad occur: However, as the systolic blood pressure increases, a similar increase will not be seen in the diastolic pressure. Instead, what will result is a widened pulse pressure The baroreceptors in the carotid artery sense changes in blood pressure. When the baroreceptors sense increased blood pressure, the body’s response is to slow the heart rate. The symptoms of the Cushing triad will present in the late stages of ICP when the brainstem is about to herniate. That is why it is essential for the provider to be vigilant of early signs and symptoms of increased ICP to treat the underlying condition and prevent the patient from progressing to the late stages of ICP. Even though ICP has multiple etiologies, it always presents with the same signs and symptoms. It is important for the provider to recognize and treat the early signs and symptoms to keep the patient from progressing to late-stage signs and symptoms, known as the Cushing triad, and ultimately, brainstem herniation.Cushing Triad: A Unique Set of Symptoms
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.