Ventricular Rhythms and Asystole
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Ventricular arrhythmias arise from the ventricles and have a unique and sometimes bizarre appearance.
- Premature ventricular complexes occur singly or as part of a pattern.
- Ventricular tachycardia is a potentially lethal rhythm with a unique appearance
- In ventricular fibrillation, the heart quivers or “fibrillates,” rendering the ventricles unable to fill with blood.
- Asystole is often referred to as “flat line” and indicates there is no longer any electrical activity in the heart.
The QRS complex represents ventricular depolarization. When impulses are generated from the ventricles, the QRS complexes widen and are greater than 0.12 seconds. Other supraventricular rhythms may also present with prolonged QRS complexes if there is an impulse conduction disturbance from a supraventricular focus into the ventricles.
Normally, the atria contract first, followed by the ventricles, allowing blood to fill the ventricles. When the ventricles contract, a sufficient amount of blood is ejected into the systemic circulation. If the ventricles contract before the atria, the heart’s efficiency is significantly reduced because only a small amount of blood is available to supply the entire body.1
Ventricular arrhythmias include premature ventricular complexes, ventricular tachycardia, ventricular fibrillation, and idioventricular rhythms. The ventricular escape rhythm is the last line of defense in a heart with a severely compromised conduction system.
Related Video – Ventricular Rhythms and Asystole
The premature ventricular complex (PVC) is a single ectopic beat coming from an irritable focus that supersedes the sinoatrial (SA) impulse. It is not a rhythm but rather a single entity disrupting the core rhythm. It occurs earlier than expected in the cardiac cycle. PVCs have no P wave because the impulse originates in the ventricles, so there’s no atrial depolarization from the sinoatrial node. The QRS complex is wide and more than 0.12 seconds. A striking feature of PVCs making them easy to spot is the T wave morphology opposite the deflection of normal QRS complexes.Premature Ventricular Complexes
Related Video – ECG Rhythm Review – PVCs
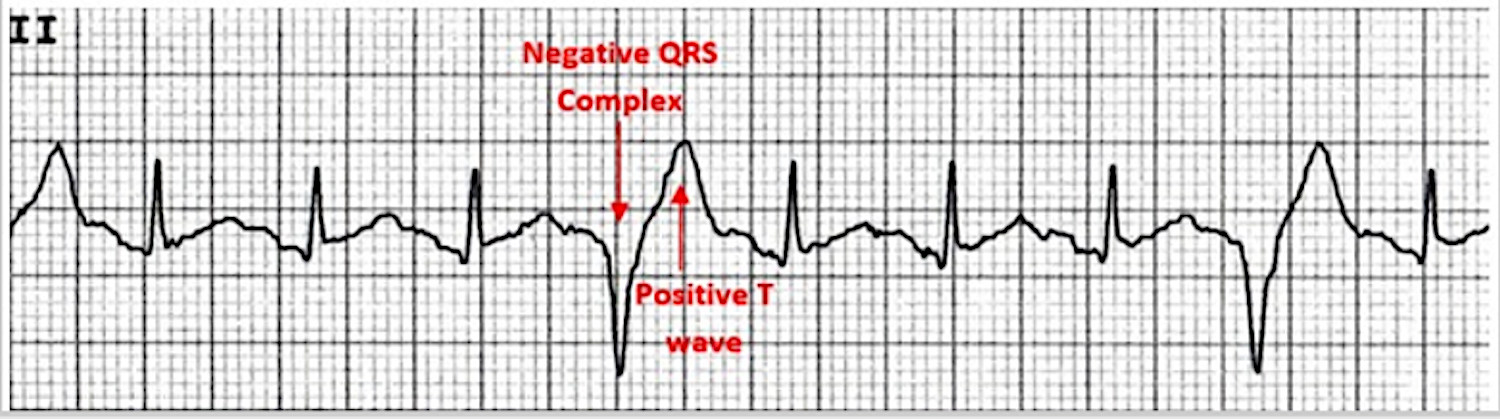
An ECG displays a QRS complex with a negative deflection followed by a T wave with a positive deflection.
Related Video – One Quick Question: What are PVCs (Premature Ventricular Contractions)?
During a PVC, a compensatory pause follows the ectopic beat. The underlying rhythm remains unchanged because the impulse generated from the ventricles does not affect the impulses from the sinoatrial node, enabling the SA node to discharge at the expected time.
In the figure below, the arrows indicate PVCs. A dropped R wave follows the PVC. That compensatory pause does not affect the core rhythm because the SA node discharges at its own pace.
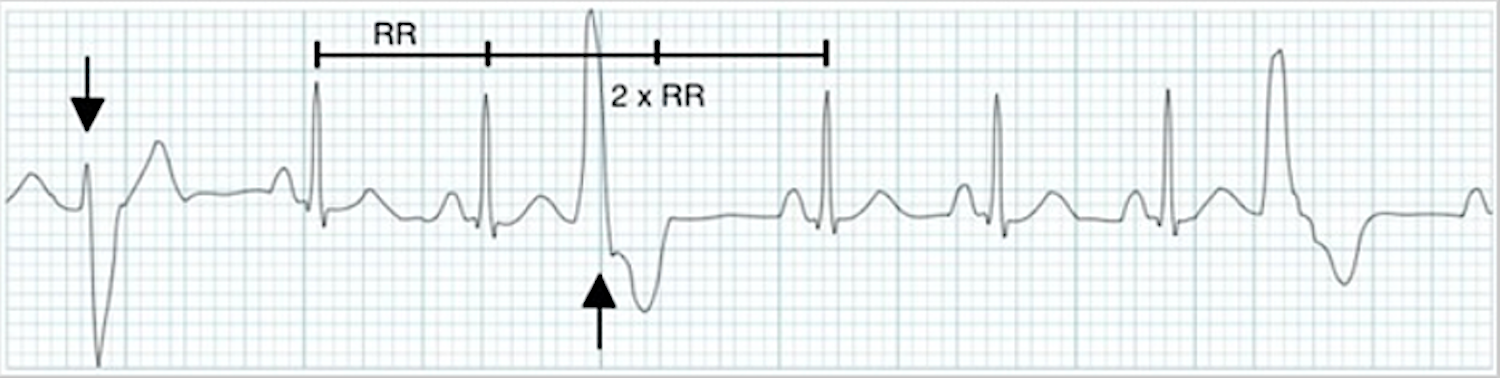
ECG tracing displays PVCs with a dropped R wave.
It’s possible a PVC occurs between regular complexes without disturbing the regular pattern of the sinoatrial node. That phenomenon is known as an interpolated premature ventricular complex.2
PVCs are caused by myocardial irritability. When multiple PVCs occur within one minute, it is pathologic. Chest pain associated with PVCs can be life-threatening. Clinicians must report PVCs in ECG documentation.
Unifocal PVCs originate from one irritable focus and have the same morphology throughout. Multifocal PVCs occur when multiple PVC morphologies are present. Multifocal PVCs are more serious than unifocal PVCs.Unifocal and Multifocal PVCs
When the R wave of a PVC overlaps the T wave of the core rhythm, it’s known as an R-on-T phenomenon. It’s the result of a relative refractory state of the T wave. Some of the charges are still polarized secondary to a strong ventricular depolarization, precipitating more dangerous rhythms, such as ventricular tachycardia or ventricular fibrillation.R-on-T Phenomenon
Clinicians must suspect increased myocardial irritability when PVCs occur in succession without a normal beat intervening. A couplet is two successive PVCs. Three or more PVCs in a row is known as a run. Clinicians should document the number of PVCs. When several PVCs occur in a row, the normal pacemaker can’t resume, causing significant irritability.Runs and Couplets
When a pattern forms between PVCs and normal beats, it’s known as grouped beating. When a PVC occurs between every other normal complex, it’s known as bigeminy. One PVC followed by two sinus complexes is known as trigeminy. If a PVC is followed by three sinus complexes, it’s a quadrigeminy. An ECG tracing displays bigeminy, where every second beat is a PVC. The underlying rhythm is sinus rhythm. An ECG tracing displays quadrigeminy, where every fourth beat is a PVC.Grouped Beating


Related Video – One Quick Question: How Can I Remember the PVCs?
Read: Introduction to ECG Interpretation
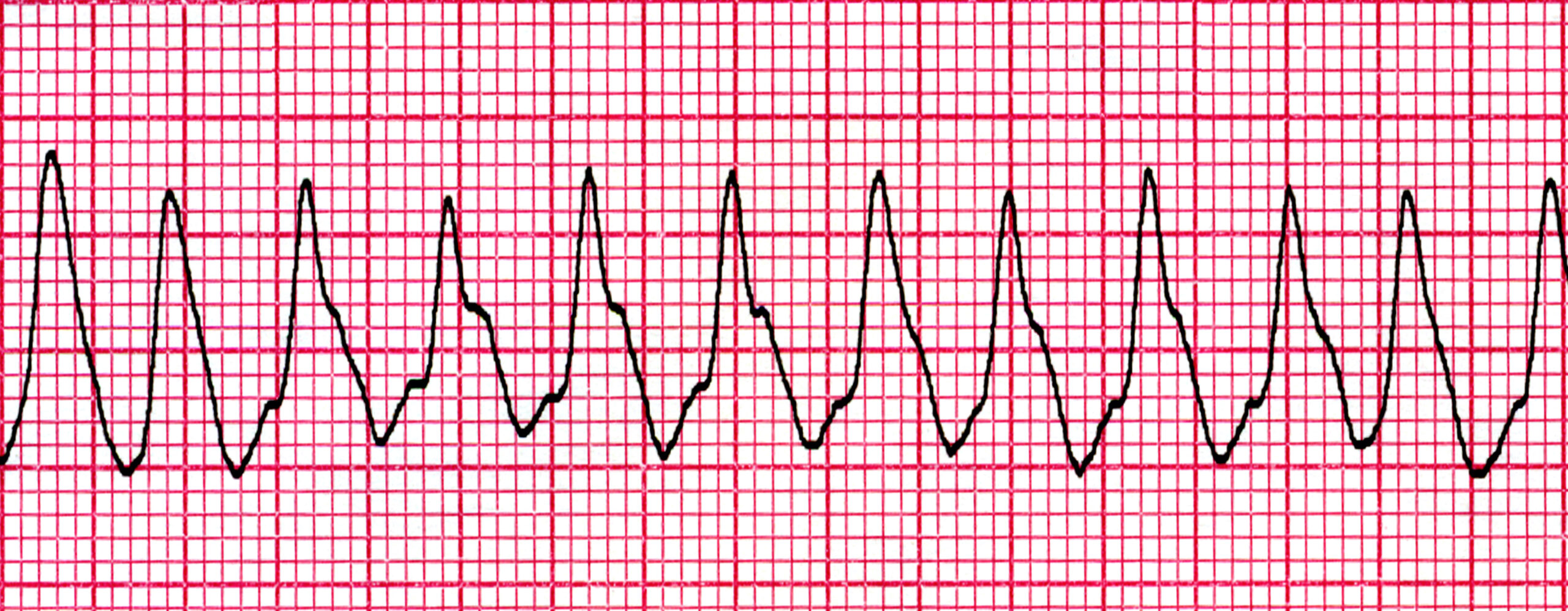
Ventricular tachycardia (VT) originates from an extremely irritable focus that overrides the higher pacemaker sites, causing a sustained PVC run. VT is classified as an arrhythmia and has a rate of 150 to 250 beats per minute (bpm).3 The R-R interval may have a slightly irregular appearance, but the complexes are generally uniform in morphology. Like PVCs, VT will have bizarre-looking QRS complexes 120 milliseconds (0.12 seconds) or longer and a T wave deflection opposite the R waves. P waves will not be seen before the QRS complexes. VT patients will have serious signs and symptoms due to the insufficient blood flow to the body as the ventricles are beating too quickly to fill with blood. Most patients will be unconscious, and a pulse may or may not be felt. Patients in slow VT may be conscious.4 An ECG strip showing ventricular tachycardia.Ventricular Tachycardia
Related Video – ECG Rhythm Review – Ventricular Tachycardia
In ventricular fibrillation (VF), an extremely irritable ventricular focus causes impulses to fire in such a chaotic manner the ventricles begin fibrillating. In essence, the heart merely quivers rather than beating forcefully. Ventricular fibrillation is a lethal arrhythmia because the fibrillating heart does not send blood to the rest of the body.5 VF has a distinct pattern and is one of the easiest arrhythmias to identify. There are no waves or complexes. It is a simple, grossly chaotic fibrillatory pattern. Patients in VF will be unconscious, apneic, and lack any palpable pulses. VF is often preceded by ventricular tachycardia. The “cure” for both VT and VF is electricity. Defibrillation “shocks” the heart out of its chaotic rhythm, allowing the heart’s normal pacemaker to take over again.Ventricular Fibrillation
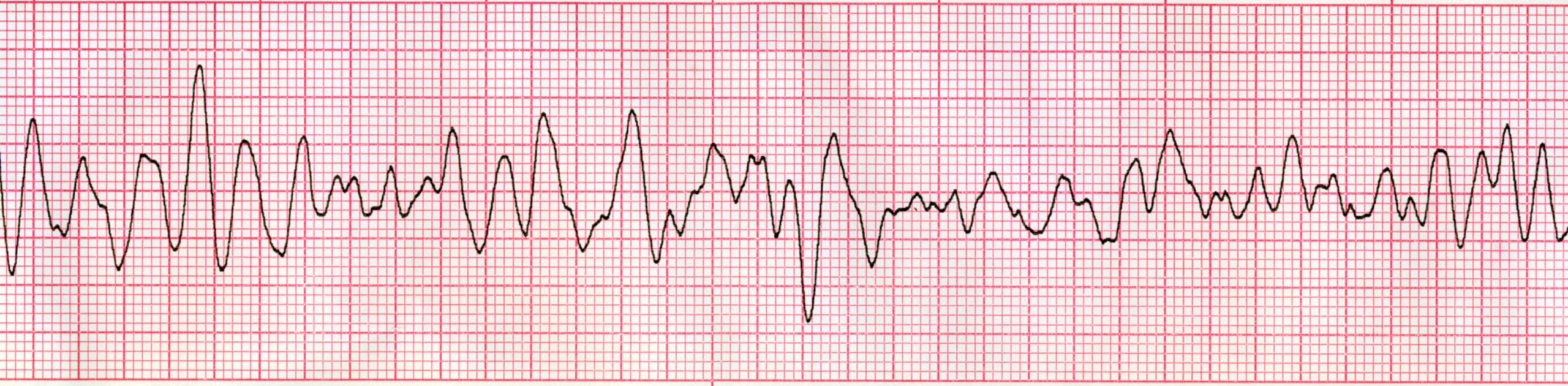
Ventricular fibrillation is treated with defibrillation with the goal of restoring a normal rhythm.
Related Video – ECG Rhythm Review – Ventricular Fibrillation
An idioventricular rhythm is produced by an escape beat. When higher pacemaker sites fail to produce an impulse, a ventricular escape rhythm takes place in the form of an idioventricular rhythm. Idioventricular rhythms have a rate of 20–40 bpm. If the rate is slower than 20 bpm, it is an agonal rhythm because the heart is on the brink of ceasing all activity. An accelerated idioventricular rhythm is possible when the rate is above 40 bpm. An idioventricular rhythm is produced by an escape beat. Because the impulse is generated from the ventricles, there are no P waves. The escape mechanism has taken over the failed atrial pacemaker sites. Clinicians will observe very slow ventricular complexes with a regular rhythm which may occasionally be irregular. The ventricular complexes are 120 milliseconds (0.20 seconds) or longer.Idioventricular Rhythm

Related Video – ECG Rhythm Review – Idioventricular Rhythm
- RATE: 20–40 bpm; can be slower (agonal) or faster (accelerated).
- RHYTHM: regular.
- P WAVES: none.
- PR INTERVAL: none.
- QRS COMPLEX: wide and bizarre; 0.12 seconds or longer.
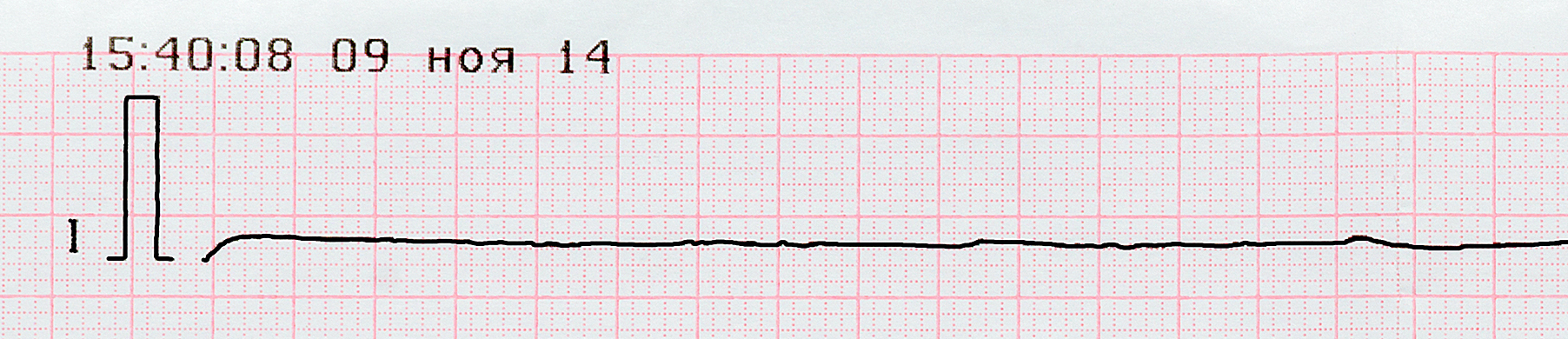
Asystole is when all the electrical activity in the heart stops, resulting in a straight or “flat line” pattern.6 It is a lethal arrhythmia and almost always is resistant to resuscitation efforts. The patient in asystole is, for all intents and purposes, deceased. Clinicians must ensure patients with a flat isoelectric line are truly in asystole and not another rhythm such as a fine VF. They should also rule out machine or operator error by checking the rhythm in several leads other than Lead ll. Asystole is represented by a “flat line,” which is a cessation of electrical activity.Asystole
Related Video – Hs and Ts: Treating Asystole
Ventricular arrhythmias come from the ventricles. They have fairly unique and bizarre ECG appearances. Premature ventricular complexes either occur solely or with others. VT is potentially lethal while in VF the heart’s ventricles can’t fill with blood. Asystole occurs when the heart lacks electrical activity. Each ventricular arrhythmia has its own heart rate, rhythm, P wave placement, PR interval, and QRS complex.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Jordan King; David R. Lowery. Cardiac Output. National Library of Medicine. 2021.
2. Yasar Sattar; Muhammad F. Hashmi. Ventricular Premature Complexes. National Library of Medicine. 2022.
3. Khashayar Farzam; John R. Richards. Premature Ventricular Contraction. National Library of Medicine. 2022.
4. Mayo Clinic. Ventricular Tachycardia. 2022.
5. Mayo Clinic. Ventricular Fibrillation. 2021.
6. Cleveland Clinic. Asystole. 2021