Treatment of Bradyarrhythmias
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Atropine is the first-line drug of choice for the treatment of symptomatic bradycardia unless contraindicated.
- Alternative drugs are dopamine and epinephrine. They’re administered via intravenous infusion and are titrated to patient response.
- Transcutaneous pacing is an alternative to drug therapy, though it is a stopgap measure.
- Clinicians should consult a cardiologist when treating patients with bradyarrhythmias.
Adult Bradycardia With a Pulse Algorithm
Read: Bradyarrhythmias
Atropine is an anticholinergic drug used as a first-line therapy for symptomatic bradycardia.1 It antagonizes the muscarinic-like actions of acetylcholine and other choline esters by blocking parasympathetic influences, increasing heart rate and atrioventricular conduction. It can be used to temporarily improve bradyarrhythmias until a more permanent solution is found, such as applying a transvenous pacemaker.Atropine
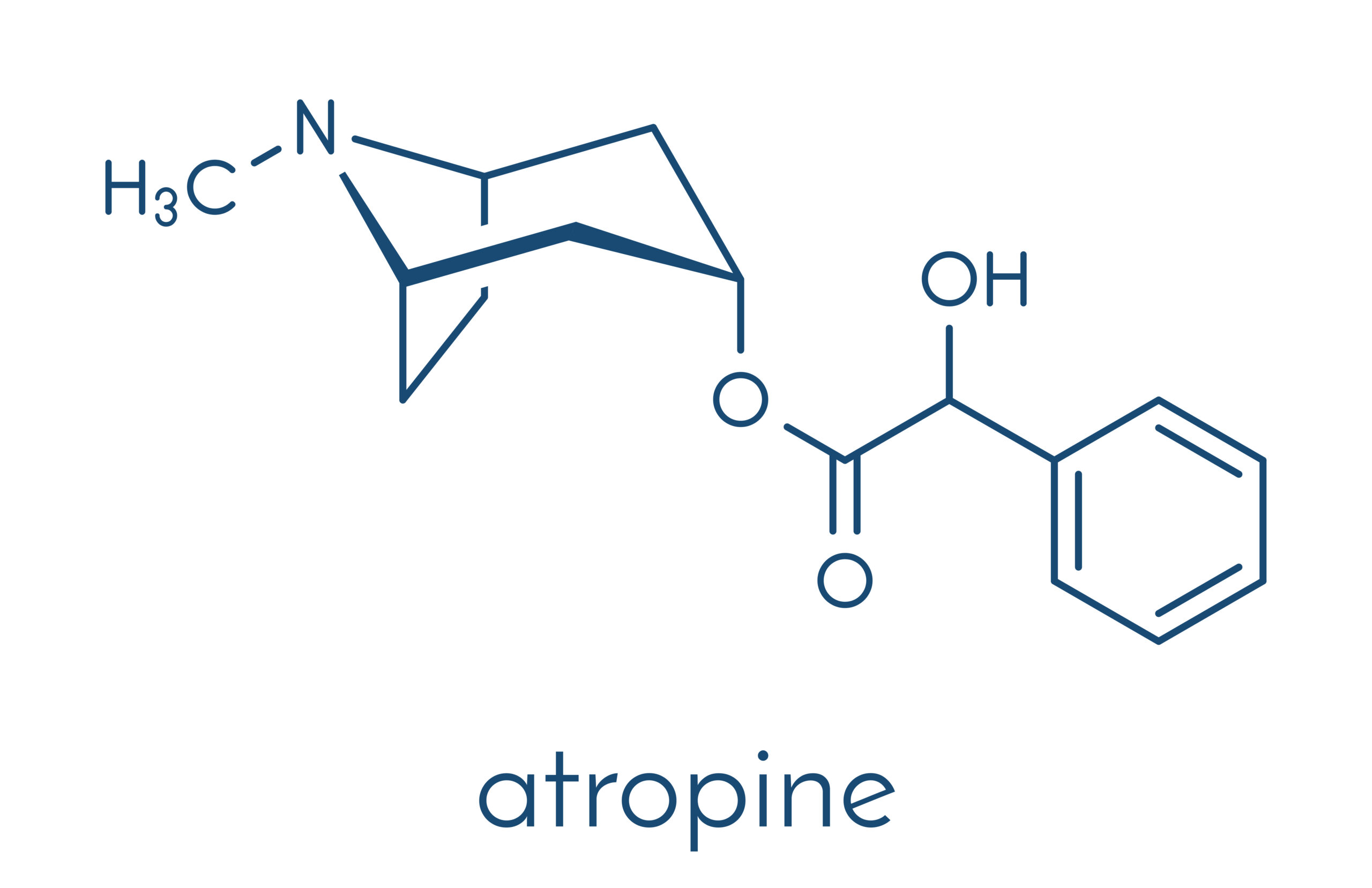
Atropine is an anticholinergic drug which increases the heart rate and atrioventricular conduction.
To correct bradycardia, an intravenous bolus of atropine 0.5 mg is administered every 3–5 minute as needed, up to 3 mg.2 Clinicians must remember administering atropine in a dose lower than 0.5 mg may worsen bradycardia.
Clinicians should carefully administer atropine to patients with acute myocardial infarction because increasing the heart rate may also increase the oxygen demand of myocytes, further worsening the ischemia or infarction.
Related Video – Atropine – ACLS Drugs
Atropine is ineffective for patients who have had a heart transplant because they lack vagal innervation essential for the antimuscarinic effects of atropine.3 Bradyarrhythmias unlikely to respond to atropine include second-degree AV block (Mobitz type 2) and third-degree AV block with a wide QRS complex, representing a non-nodal block. Clinicians treat the lower blocks with transcutaneous pacing. Transcutaneous pacing is a temporary intervention to treat symptomatic bradycardia until transvenous pacing is employed. In the event atropine and transcutaneous pacing cannot be administered, transvenous pacing is the best option. Clinicians should refer to a specialist in these cases.Transcutaneous/Transvenous Pacing
Transcutaneous Pacing
If atropine is contraindicated, fails to achieve its therapeutic effect, or transcutaneous pacing isn’t available, dopamine and epinephrine are administered. They may be given if the bradycardia is caused by a beta-blocker or calcium-channel-blocker overdose.Other Medications
Dopamine is a catecholamine with alpha- and beta-adrenergic effects to increase heart rate. At higher doses, it causes vasoconstriction. Clinicians should be cautious if the patient is at risk for acute myocardial infarction or myocardial ischemia. Dopamine is administered via intravenous infusion at a rate of 5–20 mcg/kg/min and is titrated according to the patient’s response. This drug must be tapered slowly.Dopamine
Related Video – Dopamine – ACLS Drugs
Epinephrine has the same effects as dopamine and is administered via intravenous infusion at a rate of 2–10 mcg/min, titrated according to the patient’s response.Epinephrine
Related Video – Epinephrine – ACLS Drugs
Per the American Heart Association, if bradycardia produces symptoms and the patient is unstable, the initial treatment is atropine. If atropine is ineffective, alternative medications such as dopamine or epinephrine may be administered while waiting for a more definitive intervention such as transcutaneous pacing and, ultimately, emergency transvenous pacing. It’s mandatory that clinicians consult a specialist.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Kevin McLendon; Charles V. Preuss. Atropine. National Library of Medicine. 2022.
2. American Heart Association. Management of Symptomatic Bradycardia and Tachycardia. 2005.
3. San Mateo County Emergency Medical Services. Symptomatic Bradycardia. 2019.