Diabetic Ketoacidosis (DKA)
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Diabetic ketoacidosis (DKA) is primarily a complication seen in patients with type 1 diabetes.
- The main cause of diabetic ketoacidosis is the stress response, which can be triggered by infection or illness.
- Clinicians will learn about the etiology, pathophysiology, signs and symptoms, and complications of diabetic ketoacidosis.
DKA is primarily a complication of type 1 diabetes mellitus. When a patient with type 1 diabetes experiences stress, they may contract DKA. Patients with type 2 diabetes contract hyperglycemic hyperosmolar syndrome (HHS).Overview of DKA
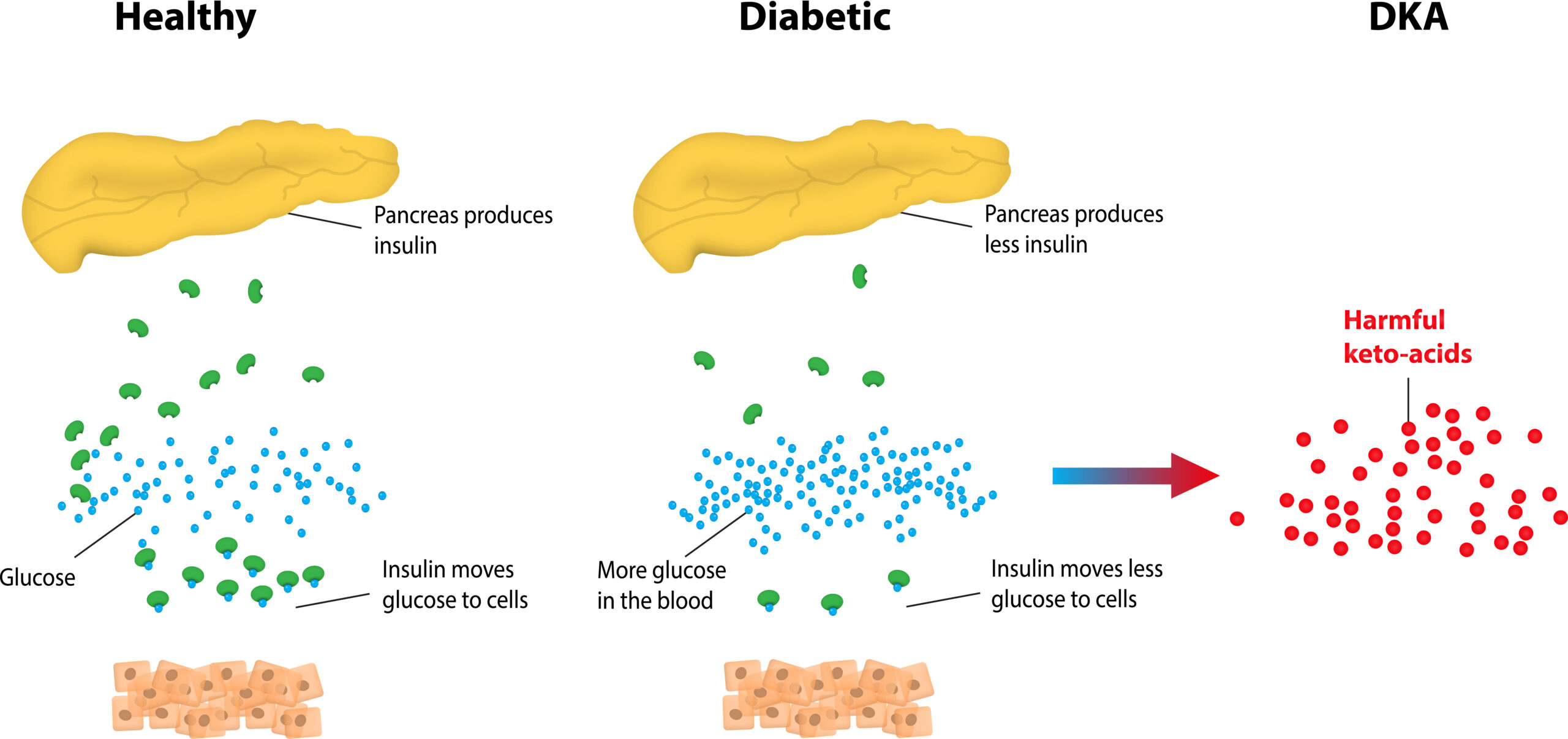
DKA presents in a type 1 diabetes patient when insulin is very poorly controlled, resulting in the production of blood acids called ketones DKA often occurs when a patient has experienced stress, typically an illness. Other stressful situations may cause DKA, such as psychological or workplace stress. It can also be caused by problems with insulin therapy, such as pump failure or missed insulin doses. A stomach virus or the flu can stress the body and lead to diabetic ketoacidosis.Etiology of DKA

The patient’s stress response causes a release of stress hormones. The primary hormone is cortisol which is the opposite of insulin and raises blood glucose. It also increases epinephrine and norepinephrine, the flight or fight hormones. They also increase blood glucose. Type 1 diabetes is an autoimmune disorder where the beta cells don’t produce adequate insulin. A stressor increases stress hormones and blood glucose, and type 1 diabetics don’t have the insulin to protect against the increase, leading to DKA.Pathophysiology of DKA
Related Video – SIADH vs. Diabetes Insipidus
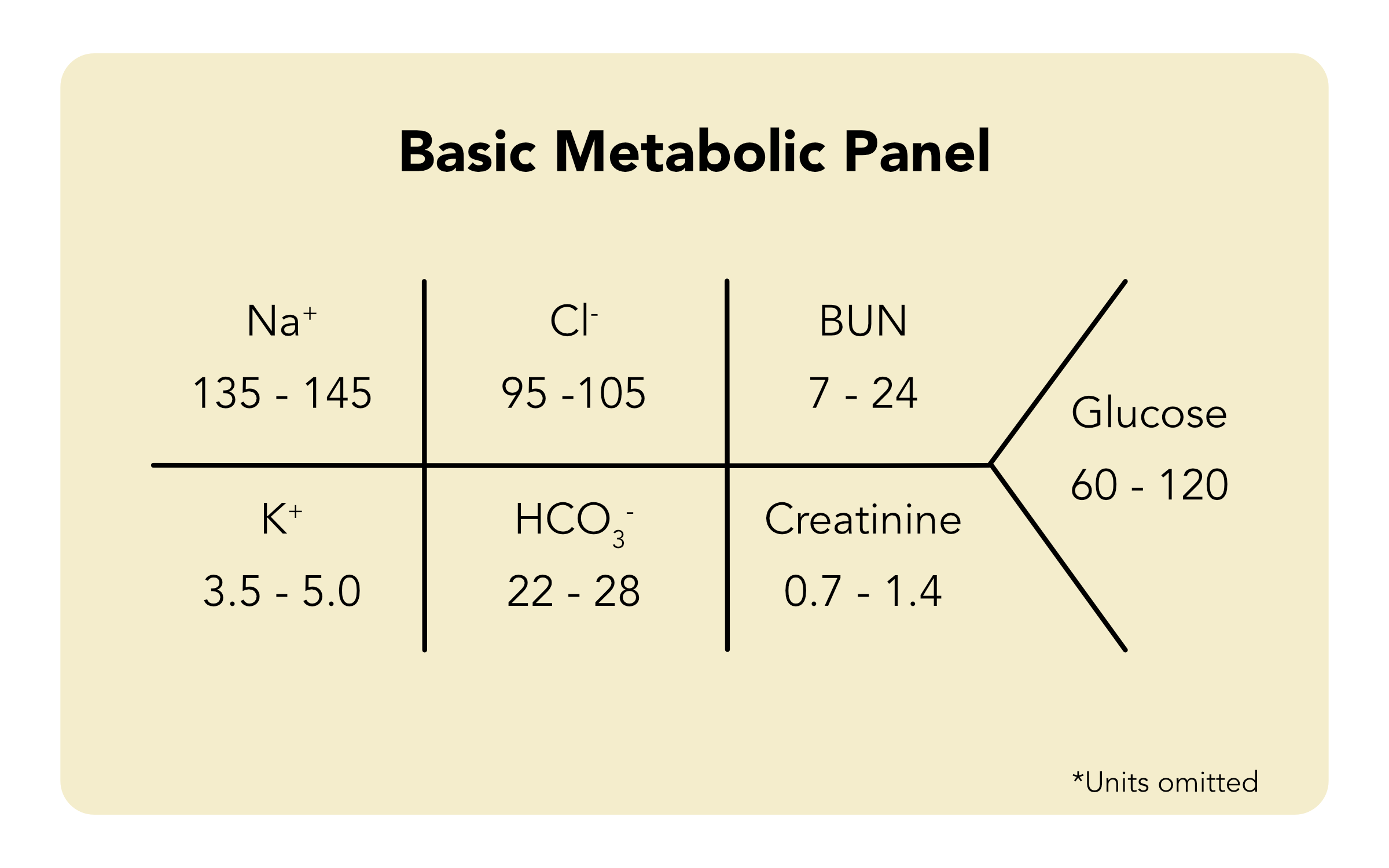
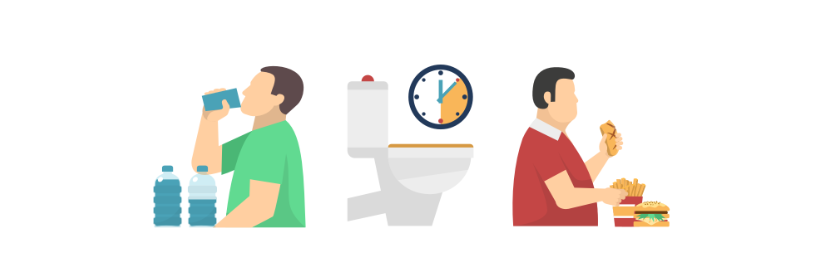
The number one sign of DKA is hyperglycemia, or high levels of blood glucose. Insulin deficiency may also cause lipolysis (the breakdown of fats). Lipolysis occurs because there’s no insulin to protect the body. Insulin protects the body from breaking down fat to be used for energy because lipolysis byproducts are fatty acids converted into keto acids. An increase of keto acids throws the body into a state of metabolic acidosis. During diabetic ketoacidosis, fats break down into keto acids. A ketone test determines the level of ketones in the blood. To recall the symptoms of DKA, clinicians remember the “three Ps”: Read: Hyperosmolar Hyperglycemic Syndrome Below, each symptom is detailed. Polydipsia is extreme thirst and occurs in DKA patients for several reasons, mainly because the patient’s serum osmolality is extremely elevated. The blood is very concentrated due to the tremendous increase in blood glucose, so the body must dilute itself, causing the patient’s extreme thirst. Polyuria is frequent, excessive urination due to osmotic diuresis. When the patient starts urinating, glucose spills out into the urine. Glucose has osmotic pulling power, so wherever it goes urine follows. That is a huge factor with DKA because the blood glucose is so elevated. Polyphagia is when the patient is extremely hungry. Without insulin, there is no way to feed the cells. Insulin acts as a key to “unlock” adipose tissue, muscle tissue, and liver cells, allowing glucose to flow inside the cells. If insulin doesn’t allow glucose into the cells, they go into a state of starvation and cause polyphagia. The three Ps are polydipsia, polyuria, and polyphagia. A patient in any state of acidosis has hyperkalemia. Clinicians start these patients on insulin to drop their potassium. Acidosis and hyperkalemia go hand in hand just like alkalosis and hypokalemia. Patients with metabolic acidosis will also complain of stomach pain, nausea, and vomiting. The body is trying to rid itself of the extra acid.Signs and Symptoms

Polydipsia
Polyuria
Polyphagia
Related Video – What are SIADH and DI?
Hypokalemia is the worst outcome for a DKA patient, and it is responsible for the majority of DKA fatalities. Hospitals have certain protocols for DKA patients to avoid hypokalemia. Clinicians first hydrate patients with normal saline then, when the patient is stabilized, they administer a hypotonic solution to decrease the patient’s serum osmolality. The patient will eventually receive IV fluids using 5% dextrose in water (D5W) instead of normal saline because clinicians don’t want to drop their blood glucose too rapidly, as rapid drops in serum osmolality are dangerous. Clinicians should also add some potassium to the patient’s IV fluids to avoid hypokalemia. Clinicians must remember hypokalemia poses the greatest threat to DKA patients. The patient should come in hyperkalemic, as the DKA treatment drastically drops potassium levels. Also, the patient is most likely experiencing ongoing stomach issues and vomiting. Prolonged vomiting leads to hypokalemia, so clinicians must monitor potassium levels in DKA patients.Potential Complications of DKA
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.