Checklist for Fibrinolytic Therapy
Key Considerations: Fibrinolytic Checklist Overview
- The fibrinolytic checklist is a convenient way for the team leader to quickly recall the indications and contraindications for fibrinolytic therapy.
- For ACS with symptoms that began > 12 hours before presentation to the ED, the clinician considers a PCI transfer.
- For ACS with symptoms that began < 12 hours before presentation to the ED, the clinician considers the administration of fibrinolytic after assessing for contraindications and risk.
Goals for the Fibrinolytic Checklist
The clinician will:
- Understand the importance of timing in the checklist.
- Understand the use of ECG findings to determine the patient’s appropriateness for fibrinolytic therapy.
- Understand relative and absolute contraindications for the use of fibrinolytic.
Box 1: Timing of Symptoms
If the patient’s ACS symptom duration is > 12 hours, they are outside the window for fibrinolytic therapy, and the clinician considers a transfer for PCI. If the symptoms began < 12 hours before presentation, the team proceeds to Box 2.
Tissue plasminogen activator(tPA) is a type of fibrinolytic that breaks up blood clots.
Box 2: ECG Findings
The team leader evaluates the patient’s ECG and makes a diagnosis.
If the 12-lead ECG shows a STEMI or new left bundle branch block (LBBB), the team proceeds to Box 3. If STEMI or LBBB is not apparent, the checklist is discontinued.
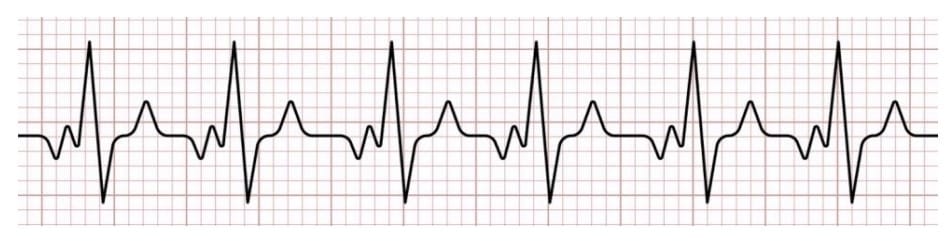
TA 12 – lead ECG evaluates the heart’s electrical activity
ST elevation myocardial infarction is identified on ECG by persistent ST segment elevation in two or more contiguous leads, reflecting acute coronary artery occlusion. Clinicians should assess lead distribution, magnitude of elevation, and reciprocal changes. A new or likely new left bundle branch block in the setting of ischemic symptoms is treated as a STEMI equivalent, as it can obscure ST-segment interpretation and represents high-risk coronary pathology.
Box 3: Contraindications to Fibrinolytic Therapy
The clinician answers each question to ascertain whether fibrinolytic therapy may be contraindicated. If the answer to any of the questions is yes, the clinician must use their best clinical judgment to determine if the team should proceed to treatment. Providers should also evaluate reversible causes such as the Hs and Ts when considering fibrinolytic therapy.
If the benefits of fibrinolytic outweigh the risks, the team proceeds to Box 4.
Box 4: Is the Patient at High Risk?
The team determines the answers to the following questions:
- Is the heart rate > 100 bpm and SBP < 100 mm Hg?
- Does the patient have symptoms of pulmonary edema?
- Does the patient have signs or symptoms of shock?
- Are there other contraindications to fibrinolytic therapy?
If the answer to any of these questions is yes, the team proceeds to Box 5. Otherwise, they proceed with the administration of fibrinolytic.
Identifying high-risk features allows clinicians to escalate care and select the most appropriate reperfusion strategy rapidly. Patients with shock, pulmonary edema, or hemodynamic instability experience significantly better outcomes when advanced interventions such as PCI are pursued early rather than delayed fibrinolytic therapy.
Box 5: Considering Transfer to a Cardiac Catheterization Lab for PCI Therapy
If the patient is NOT a candidate for fibrinolytic therapy, the clinician considers transferring the patient to the in-house cardiac catheterization lab or to a hospital with those facilities. The team must not delay PCI therapy if it is available. Percutaneous coronary intervention (PCI) performed in the cath lab is preferred when available, as it offers improved outcomes for ST elevation myocardial infarction (STEMI) patients compared with fibrinolysis. See Acute Coronary Syndrome: Managing STEMI and ACS and STEMI Systems of Care for more information on PCI and STEMI care pathways.
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.