Acute Coronary Syndrome: Managing STEMI
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- EMS obtains a 12-lead ECG and sends it to the receiving hospital to decrease morbidity and mortality.
- STEMI is diagnosed based on specific parameters involving ST elevation on a 12-lead ECG.
- Fibrinolytics or percutaneous coronary intervention (PCI) is the mainstay STEMI treatment for patients fewer than 12 hours from the onset of their symptoms.
- Low-molecular weight heparin and IV nitroglycerin are adjunctive treatments used in STEMI.
ACS Management Based on 12-Lead ECG
Acute Coronary Syndromes Algorithm
EMS should obtain a 12-lead ECG for all ACS patients, and it should be sent to the receiving hospital, allowing the ED team to triage incoming patients for either PCI or fibrinolytic therapy.[1] The ED team must make this decision quickly as it can minimize the extent of myocardial injury, reduce morbidity, and reduce mortality.
Read: Acute Coronary Syndrome – Managing NSTEMI and Low Risk ACS
12-Lead ECG Findings in Patients with STEMI
To classify as myocardial infarction, ST elevation must be observed in at least two contiguous leads equal to 0.1 mV or greater (at least 1 small box) in all leads except V2 and V3. In women, leads V2 and V3 must have ST segment elevation greater than or equal to 0.15 mV (or 1 1/2 small boxes). ST elevation must be greater than or equal to 0.25 mV (or 2 1/2 small boxes) in men under 40. Men over 40 must have an ST elevation greater or equal to 0.2 mV (2 small boxes).
For patients with STEMI or presumably new left bundle branch block (LBBB) who are 12 hours or less from symptom onset, the goal is to provide fibrinolytics within 30 minutes of arrival in the ED or PCI (percutaneous coronary intervention) within 90 minutes of arrival.
While preparing the patient, clinicians may administer adjunctive therapies, as long as they do not delay the definitive reperfusion intervention.
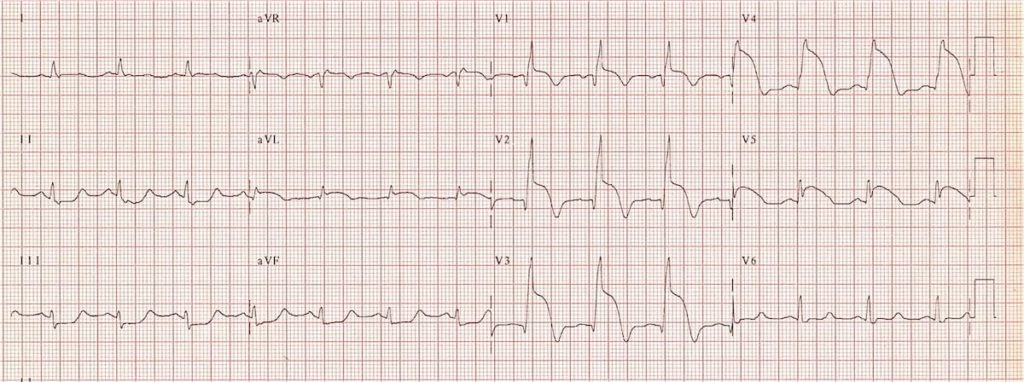
STEMI anteroseptal wall (V1-V4)[2]
Related Video – ST Segment Elevation Explained
When complete coronary artery occlusion occurs, it usually appears as STEMI on the 12-lead ECG. The gravity of complete occlusion warrants early reperfusion therapy with PCI or fibrinolytics, which preserve the myocardium. Studies have shown fibrinolytic therapy administered within the first hour of symptoms reduces mortality by 47%.[3]
Providers must minimize any delay in administration of reperfusion therapies. ACLS has described possible choke points which may cause delays as door to data, data to decision, and decision to drug (or PCI). Policies should be formulated to prevent delays. Studies show out-of-hospital transport contributes to 5% of delays, while ED evaluation causes 25% to 33% of delays.[4]
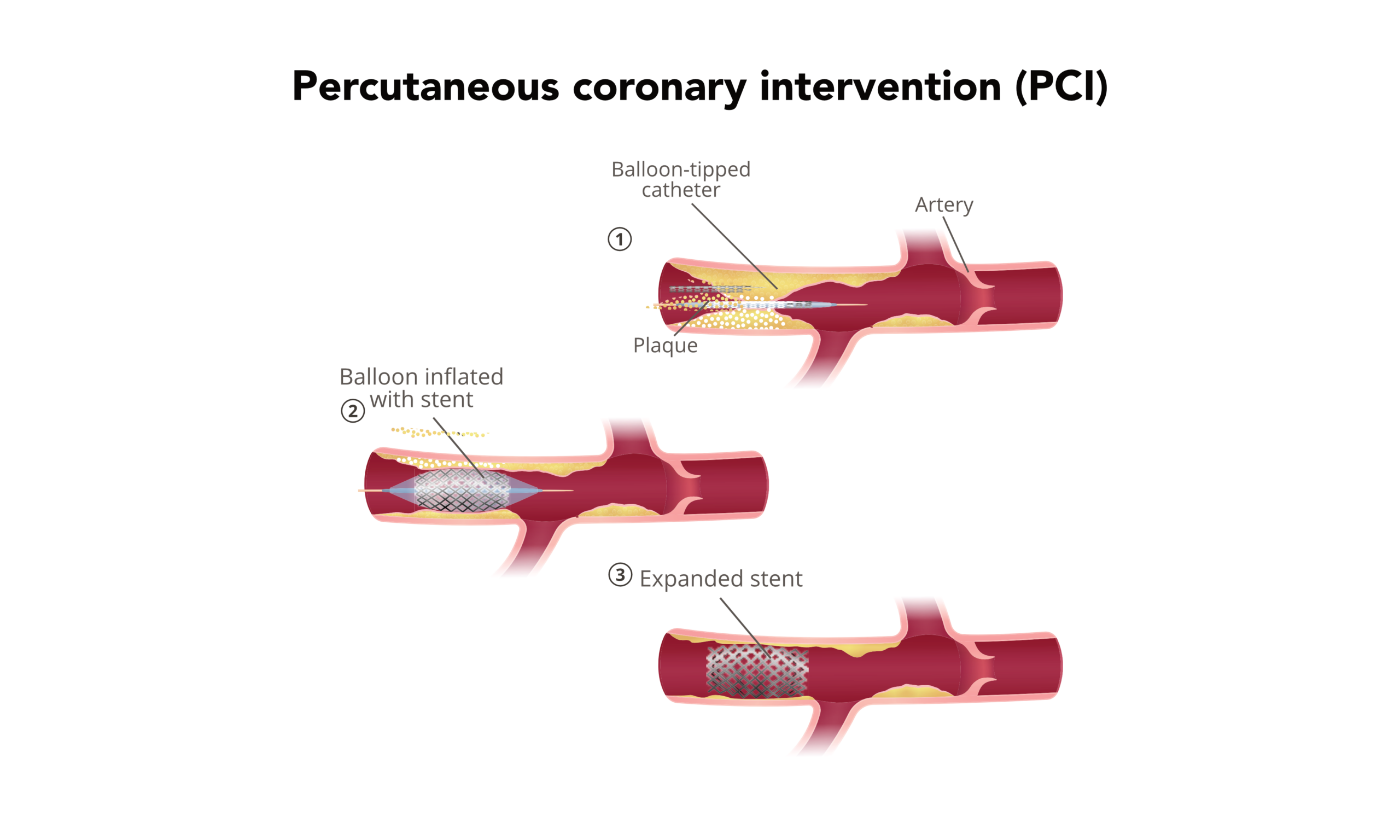
The fourth link in the STEMI chain of survival is definitive treatment. If PCI is the treatment of choice, door-to-balloon time is within 90 minutes. If the hospital is incapable of performing PCI, the patient must be transferred to a suitable institution. The time from first medical contact to device must be less than 120 minutes. If fibrinolysis is considered, door-to-needle time must be within 30 minutes. PCI utilizes stents to open and revascularize the totally occluded blood vessel. It’s preferred over fibrinolytic therapy. Studies show PCI offers greater advantages over fibrinolysis in terms of mortality, stroke, and reinfarction when intervention was administered 3–12 hours after the patient first experienced symptoms. The PCI procedure opens the occluded blood vessel to permit blood flow.Treatment: Reperfusion Therapy for STEMI with PCI
Providers administer fibrinolytic therapy to ACS patients with a significant J-point ST segment elevation MI or with a LBBB. 50% of patients undergoing fibrinolytic therapy achieve normal blood flow. Fibrinolytic therapy includes several pharmacologic agents: recombinant tissue plasminogen activator (rtPA), reteplase, and tenecteplase.[5] Fibrinolytic therapy must be administered within 12 hours of chest discomfort onset, and when PCI is not available within 90 minutes of first EMS contact. It may also be administered in patients with true posterior MI where the ST segment depression in the precordial leads is equivalent to ST segment elevation in the rest of the ECG leads. Fibrinolytic therapy is contraindicated if the onset of symptoms is more than 12 hours.Treatment: Fibrinolytic Therapy for STEMI
Related Video – Checklist for Fibrinolytic Therapy for STEMI Patients
Unfractionated or low-molecular weight heparin (LMWH) is an adjunct used for PCI and fibrinolytic therapy. Specific high-risk situations where heparin may improve the patient’s outcome include LV mural thrombosis, atrial fibrillation, and venous thromboembolism. Clinicians should exercise caution as these treatments may cause intracerebral bleeding and hemorrhage. An experienced professional should guide the adjunct usage. IV nitroglycerin relieves chest discomfort symptoms in patients with ischemic syndromes to improve pulmonary edema and decrease elevated blood pressure. That delivery mode is preferred because the dosage is easily controlled and titrated according to the patient’s needs. IV nitroglycerin is indicated in STEMI when the chest discomfort is persistent despite sublingual or spray administration of nitroglycerin as well as in patients with pulmonary edema that complicates STEMI and can be used for induced hypertension secondary to complicated STEMI.Treatment: Heparin & IV Nitroglycerin
Related Video – One Quick Question: Why Can’t You Use Nitroglycerine for an Inferior Wall MI?
EMS should obtain a 12-lead ECG for potential STEMI patients and send it to the receiving hospital. The preferred treatments for patients less than 12 hours from symptom onset are fibrinolytics or percutaneous coronary intervention. Other, adjunctive treatments include low-molecular weight heparin and IV nitroglycerin.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. American Heart Association. Systems of Care for ST-Segment–Elevation Myocardial Infarction: A Policy Statement From the American Heart Association. 2021.
2. Burns E, Buttner R. Anterior Myocardial Infarction. Life in the Fast Lane. March 20, 2021. Accessed May 10, 2021.
3. Elif Yilmazel Ucar. Update on Thrombolytic Therapy in Acute Pulmonary Thromboembolism. Eurasian J Med. 2019.
4. American Red Cross. Focused Update and Guidelines 2020. 2020.
5. Muhammad U. Baig; Jeffrey Bodle. Thrombolytic Therapy. National Library of Medicine. 2021.