Respiratory Arrest and Airway Management: Ventilation Devices
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Mouth-to-mask ventilation with a one-way valve is a safe way to provide ventilations with little to no risk of contact with potentially infectious secretions.
- Bag-mask devices require practice to master.
- Supraglottic devices are fast and easy to insert.
- Mouth-to-mouth resuscitation is no longer encouraged for infection control reasons.
Mouth-to-mask ventilation is administered using a barrier device with a one-way valve to prevent contact with blood, vomitus, or other secretions.1 It is important to use a mask that is the correct size for the patient. It should not extend below the chin or encroach on the eyes. Once the correct mask size is determined, place the mask on the patient’s face, covering the nose and mouth. Although some barrier devices have a rounded mask, others have a triangular shape. The pointier edge of the triangularly shaped mask goes over the bridge of the nose, while the wider base covers the patient’s mouth and chin area below the mouth. While holding the mask firmly in place, the rescuer performs the head tilt-chin lift maneuver. The rescuer takes a normal breath in and delivers one breath over 1 second — this should result in visible chest rise in the patient. One breath is administered in the manner described every 6 seconds for a rate of 10 breaths per minute. The chest should relax fully in between breaths. One-way valve masks need to fit properly on the patient’s face. Many health professionals carry their own masks to have on hand in case of emergency. Many health professionals carry their own masks with them in case of emergency. While providing mouth-to-mouth ventilations used to be common, this practice is no longer recommended due to the risk of contracting an infectious illness from the patient (or spreading an illness to the patient), although the risk is exceptionally low. Most people are not inclined to perform mouth-to-mouth on a stranger. However, in certain out-of-hospital situations, providing mouth-to-mouth ventilations may be the only recourse. Providing mouth-to-mouth ventilations involves performing the head tilt-chin lift maneuver and holding the airway open with the palm of one hand on the forehead while simultaneously pinching the nostrils closed. With the other hand, the rescuer grasps the chin between the thumb and fingers and pulls it gently upward. A normal breath is blown into the patient’s mouth over 1 second to achieve adequate chest rise. One breath is given every 6 seconds. Room air is about 21% oxygen. When a person takes a normal breath and breathes out, 80% of the oxygen inhaled is still available; therefore, ventilating patients with the air from the lungs provides more than enough oxygen for the patient’s survival.2 Mouth-to-mouth ventilation is no longer recommended but may be indicated in certain situations. Read: Respiratory Arrest and Airway Management: Maintaining Airway PatencyMouth-to-Mask Ventilation


Related Video – Rescue Breathing for Adults
Related Video – Rescue Breathing for Children
Related Video -Understanding Infant Rescue Breathing
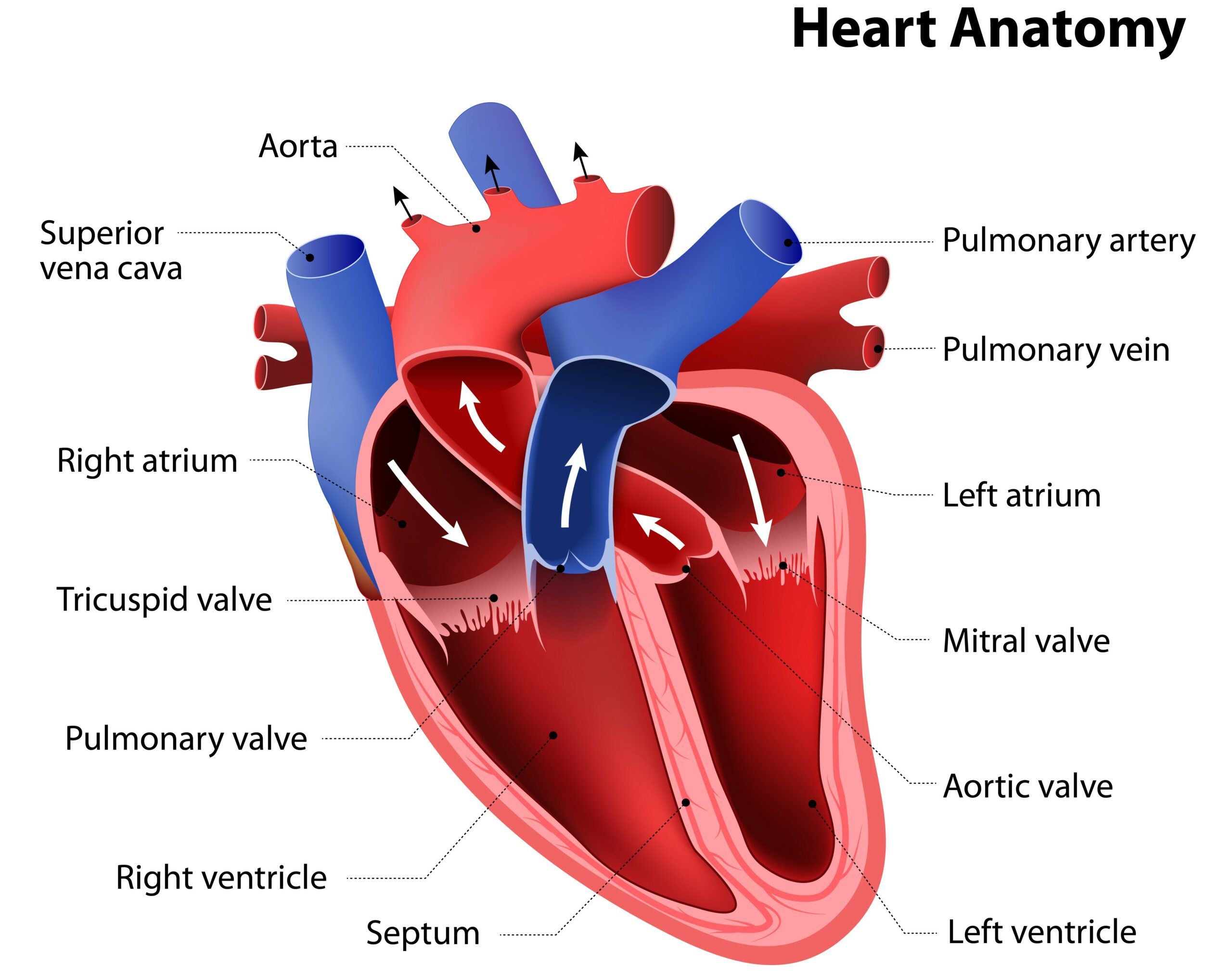
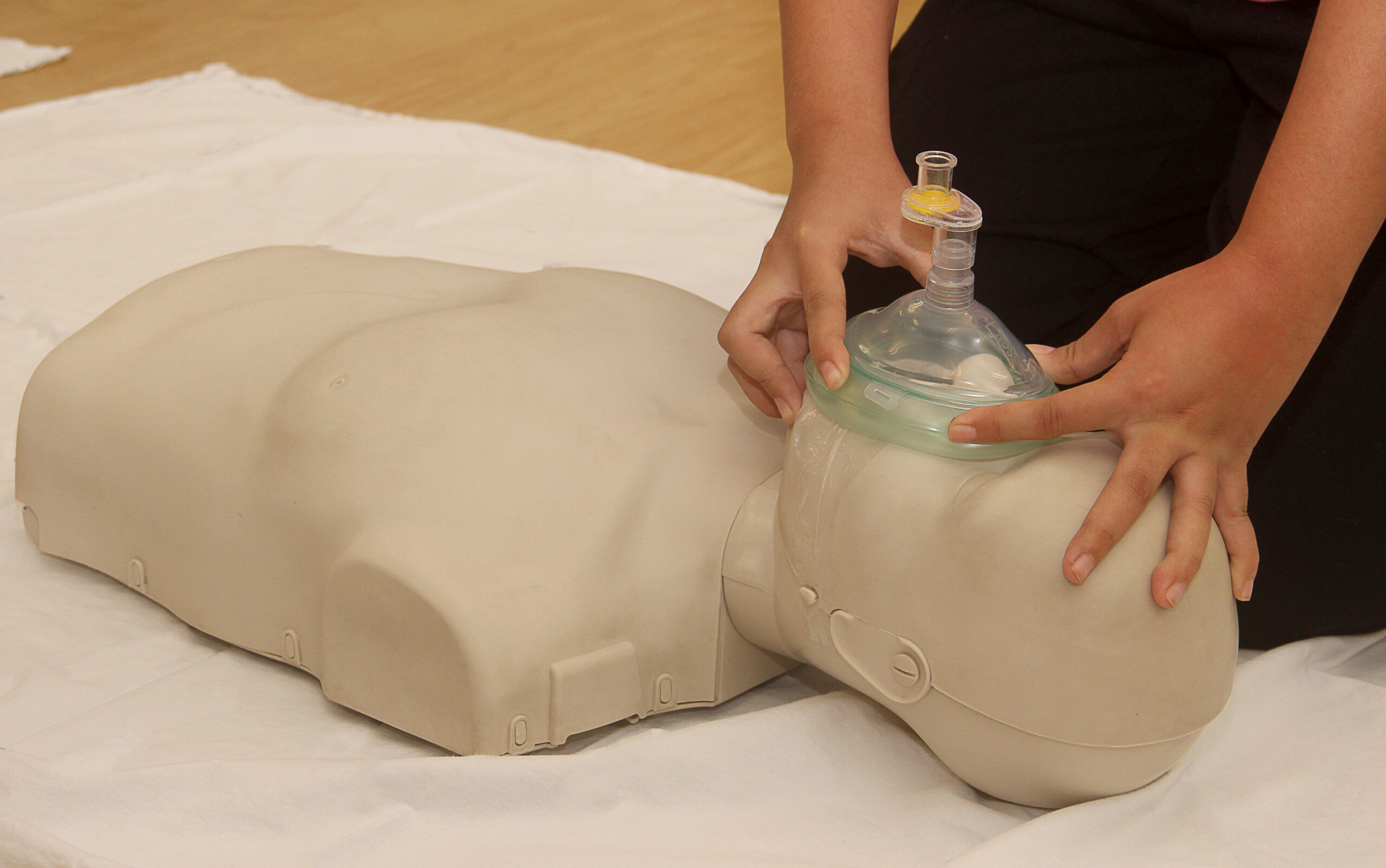
When available, a bag-mask device is a more effective tool to provide positive-pressure ventilation to patients who are not breathing or who are breathing ineffectively.3 Bag-mask ventilation allows oxygen-enriched air to be pushed into the patient’s lungs, and then from the lungs into the bloodstream to support vital organs. Mastering the bag-mask device requires much practice. It can be especially difficult for people with small hands. Sometimes it is easier to “bag” a patient with two people, one to hold the mask in place and one to squeeze the bag. Bag-mask devices have three main parts: the mask portion, which seals around the nose and mouth to prevent air from escaping; the bag part that is attached to 100% oxygen and squeezed to deliver the oxygen-enriched air; and the reservoir bag, which should be fully inflated when the bag-mask device is attached to 100% oxygen (15 L/minute). Some bag-mask devices are self inflating and can still be used in the absence of a compressed oxygen source. In the absence of a compressed gas source, these bag-mask devices deliver 21% oxygen. The rescuer uses the correctly sized face mask to form a tight seal over the patient’s nose and mouth, securing the mask in place by using the third, fourth, and fifth digits of the nondominant hand to hook under the mandible and lift it. It is important that the rescuer avoids putting pressure on the soft tissues of the neck beneath the mandible. The rescuer then forms a C with the thumb and index finger and holds the mask firmly to maintain a tight seal against the face. They must avoid the temptation to push down on the mask; doing so can occlude the airway. With the other hand, the rescuer squeezes the bag hard enough to cause the chest to rise. One breath is delivered over 1 second at a rate of one breath every 6 seconds. Breaths should be coordinated with chest compressions if the patient is in cardiac arrest. The rise of the patient’s chest should appear as though they are taking a natural breath. The rescuer needs to avoid excessive ventilation, as this can cause stomach insufflation, aspiration, damage to the lungs, and other problems. An oropharyngeal airway can also be used in conjunction with a bag-mask device to maintain an open airway.Bag-Mask Devices
Related Video – Understanding Bag Valve Mask Usage During CPR
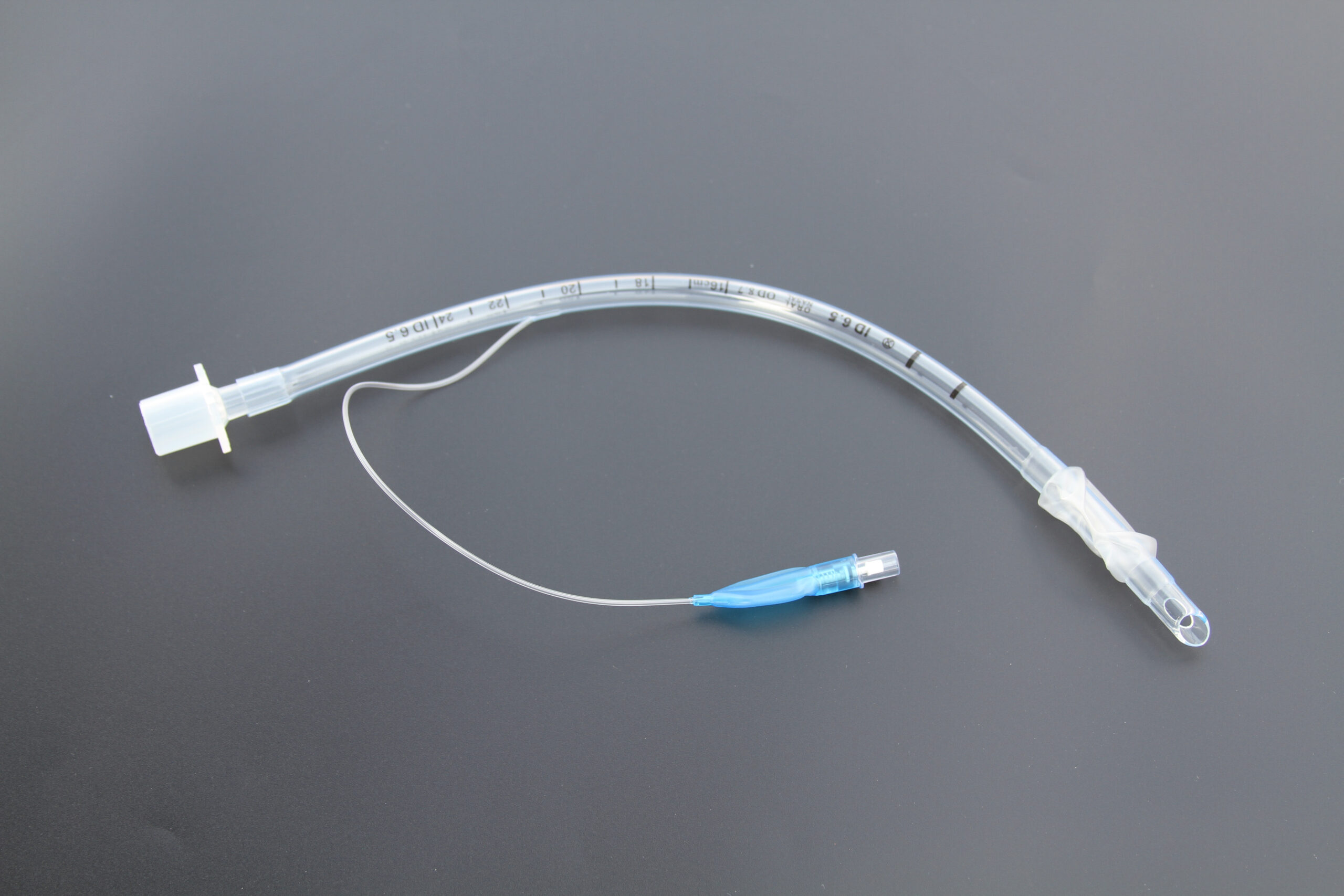
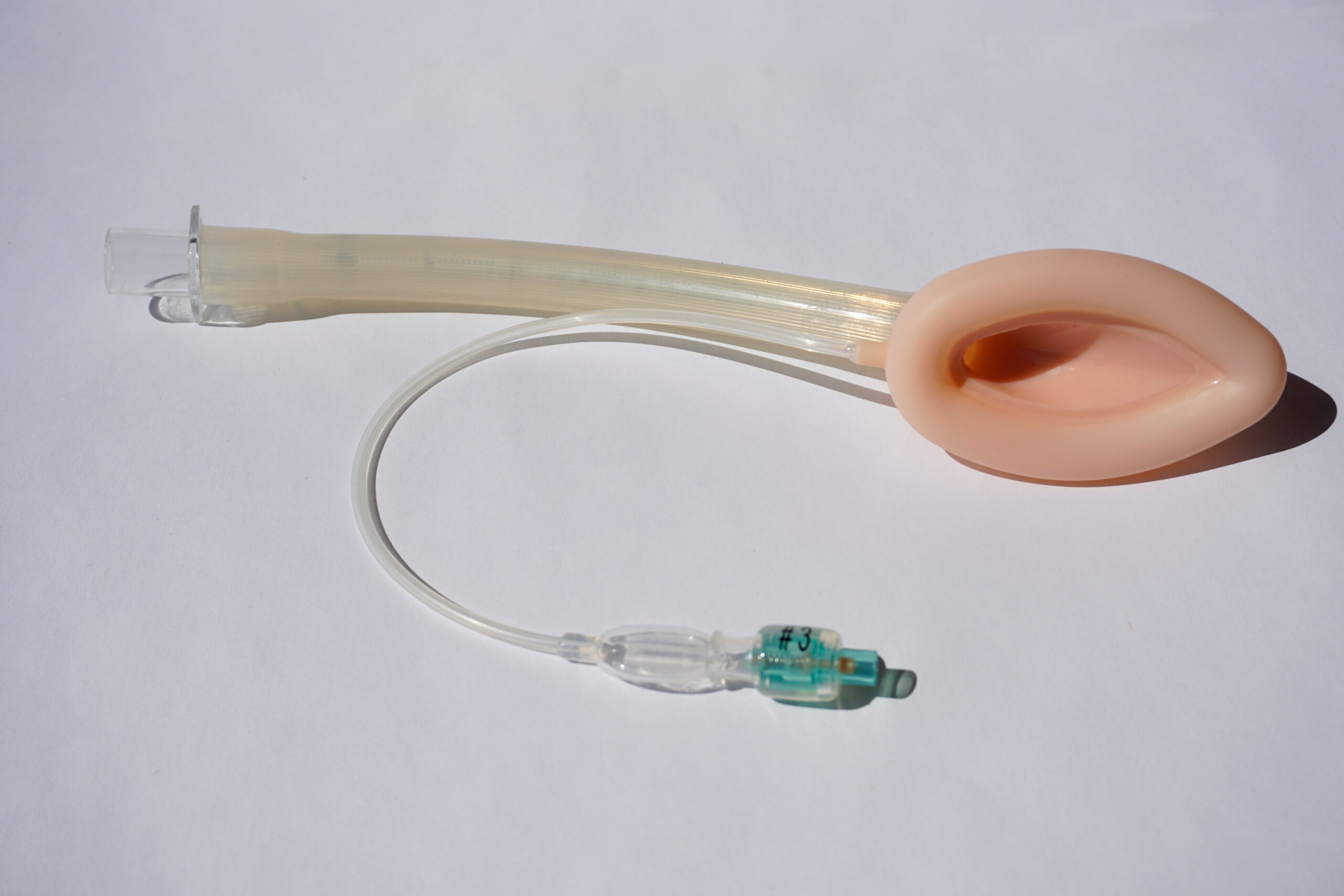
There are two main supraglottic devices. Both have advantages and disadvantages. The laryngeal mask airway (LMA) is composed of a ventilation tube attached to a small mask inserted into the mouth to cover the supraglottic structures at the hypopharynx.4 Laryngeal tubes (LTs) are airway devices used to intubate the esophagus, which is far easier than intubating the trachea. These tubes come with two cuffs: one that can be inflated to block the esophagus and one to block the trachea. The cuff that is ultimately inflated depends on whether the esophagus or trachea is intubated (most often the esophagus is intubated). Advantages: The LMA and LT can be inserted quickly and are far easier to insert than endotracheal tubes. They can be used on patients who have difficult airways. These devices can free rescuers’ hands needed for other tasks. Both devices can be inserted blindly, without use of a laryngoscope. Disadvantages: There is an increased risk of aspiration, as the airway is not as well protected as with an endotracheal tube. In rare cases where the devices fail, hypotension, hypoxia, and tachycardia may occur, which can lead to suboptimal outcomes. It can be more difficult to auscultate for breath sounds when these devices are used, thus capnography is critically important. Laryngeal Mask Device (LMA) Laryngeal Tube (LT) Mouth-to-mask ventilation is the preferred method of delivery to protect both the rescuer and the patient. Ventilation devices are designed to assist in delivering breaths to maintain effective ventilation in a patient experiencing respiratory arrest.Supraglottic Devices

More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. American Heart Association. Adult Basic Life Support. 2000.
2. Stallinger A, Wenzel V, Oroszy S, et al. The effects of different mouth-to-mouth ventilation tidal volumes on gas exchange during simulated rescue breathing. Anesth Analg. 2001.
3. Joshua T. Bucher; Rishik Vashisht; Megan Ladd; Jeffrey S. Cooper. Bag Mask Ventilation. National Library of Medicine. 2022.
4. Leslie V. Simon; Klaus D. Torp. Laryngeal Mask Airway. National Library of Medicine. 2022.