Assessing Appropriateness for Clinical Condition
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Sinus tachycardia is a common response to a physiologic stress of some kind.
- Inappropriate sinus tachycardia is diagnosed when no cause can be found for sinus tachycardia.
- Tachyarrhythmias generally present with a heart rate greater than 150 beats per minute.
- It is important to assess the patient with tachyarrhythmia to ascertain their tolerance of the rhythm and what might be causing it.
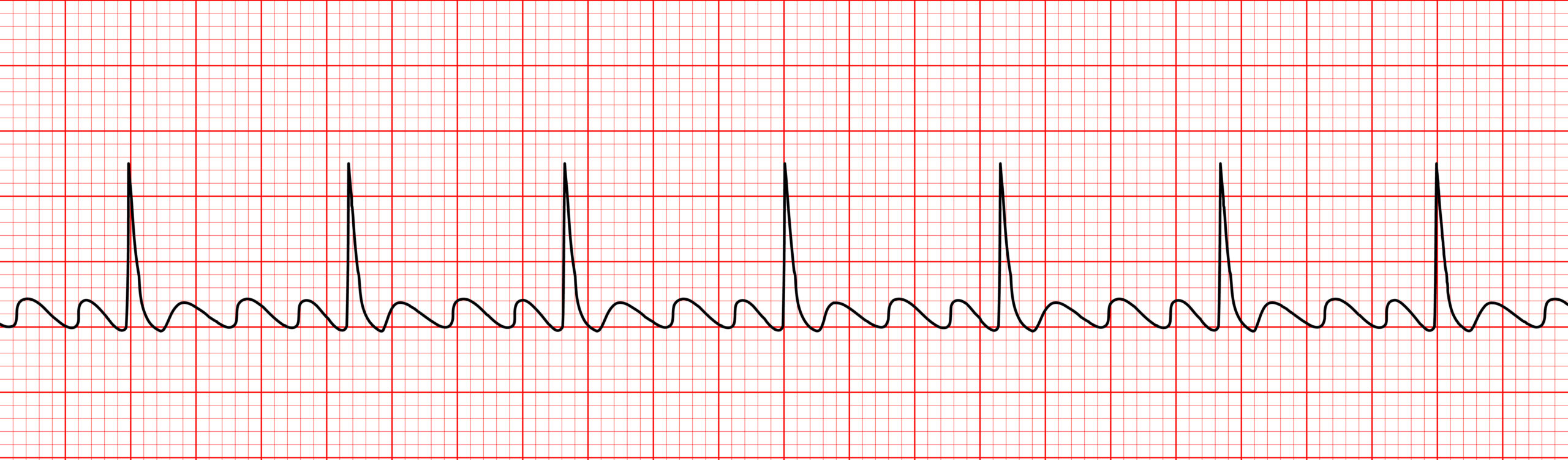
Tachycardia with a Pulse Algorithm
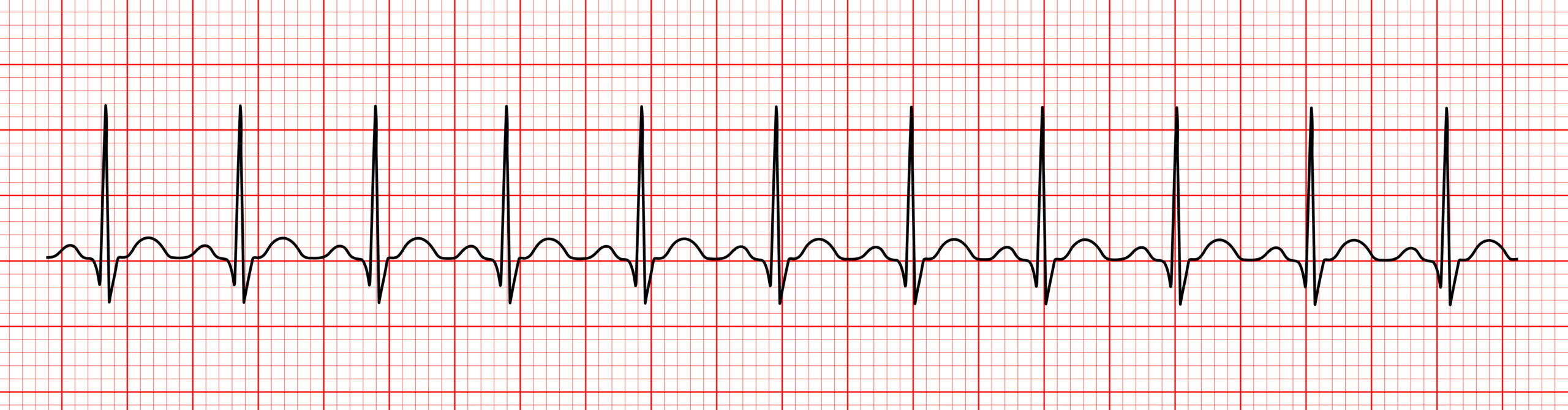
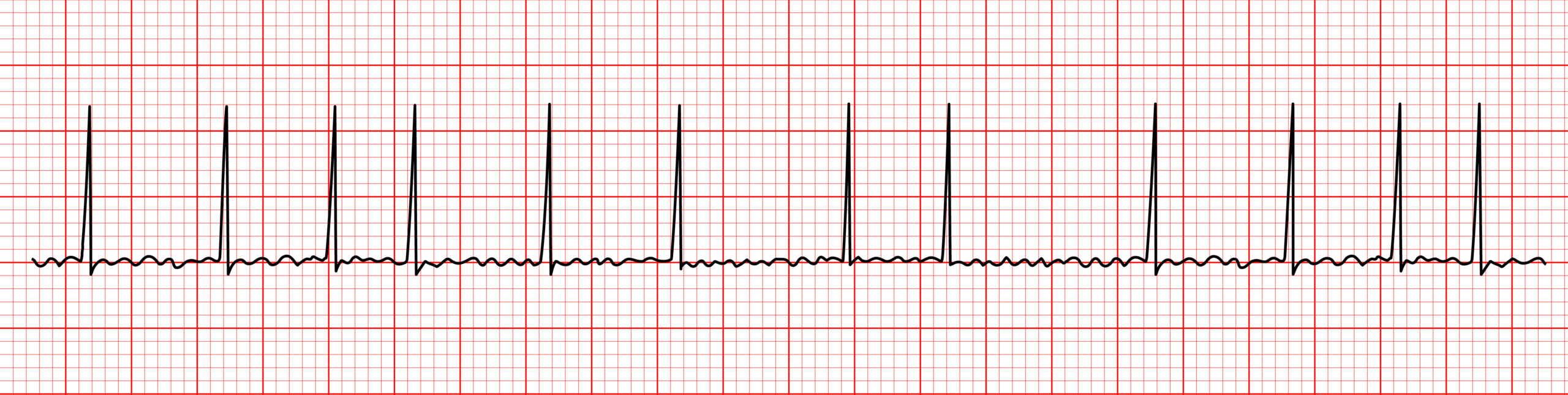
Tachycardia in adults is defined as a heart rate greater than 100 beats per minute.1 It is a common response to physical stimulation or chemical stimulation (e.g., exercise, caffeine, or cocaine). Strong emotions (e.g., fear or anxiety) can also trigger sinus tachycardia. Sinus tachycardia occurs when the cardiac impulse begins in the sinoatrial node and travels the expected route. On an ECG, a P wave will occur before each QRS complex, and the morphology of the T wave, width of the QRS complex, and other parameters will be as expected for sinus rhythm, only the rate will be faster than normal. Sinus tachycardia is a common response to physical stimulation such as exercise. It is important to determine the underlying cause of sinus tachycardia. Other causes of sinus tachycardia besides those mentioned above include the body’s normal response to pain, blood loss, or fever, all of which can be identified and treated. Hyperthyroidism may also cause sinus tachycardia. Hyperthyroidism must be diagnosed through blood tests, but suggestive physical signs might be present, such as excess sweating, thyroid enlargement, or exophthalmos.2Sinus Tachycardia

Inappropriate sinus tachycardia is diagnosed when no underlying cause for the tachycardia can be found. In these individuals, their heart rate increases with no provocation and may be as high as 150 beats per minute. Diagnosis of inappropriate sinus tachycardia will likely involve a variety of testing, including bloodwork, an ECG or Holter monitor worn for 24 to 48 hours, a chest X-ray, and an echocardiogram to rule out heart disease. The prevalence of inappropriate sinus tachycardia is unknown, but it appears to be most common in women between the ages of 15 and 50 years of age. When symptoms are bothersome, beta-blockers or calcium channel blockers may be prescribed. Sinus Tachycardia Read: The Tachycardia with a Pulse AlgorithmInappropriate Sinus Tachycardia
Related Video – ECG Rhythm Review – Sinus Tachycardia
When a tachyarrhythmia is present, the heart rate is likely to be greater than 150 beats per minute and symptoms are more likely. In addition to a quick but thorough history and physical, clinicians should assess the overall health of the individual’s cardiovascular system. Problematic tachyarrhythmias are more likely to occur in individuals with valvular disease, prior myocardial infarction, or reduced pumping function. When the patient with tachyarrhythmia is relatively stable, an ECG can provide information about the underlying cause of the arrhythmia, as well as identify the arrhythmia itself.3 An electrocardiogram measures the electrical activity of the heart using electrodes placed on the skin. An evaluation of symptoms can also point to the seriousness of the tachyarrhythmia. Individuals with a tachyarrhythmia will report palpitations (an abnormal sensation of the heart racing, fluttering, or skipping beats), lightheadedness, shortness of breath, exercise intolerance, and fatigue. More serious symptoms that should prompt swift action include chest pain, signs of heart failure, altered mental status, low blood pressure, or signs of shock. When serious signs and symptoms are present, immediate intervention is necessary, such as medications or synchronized cardioversion.Tachyarrhythmias
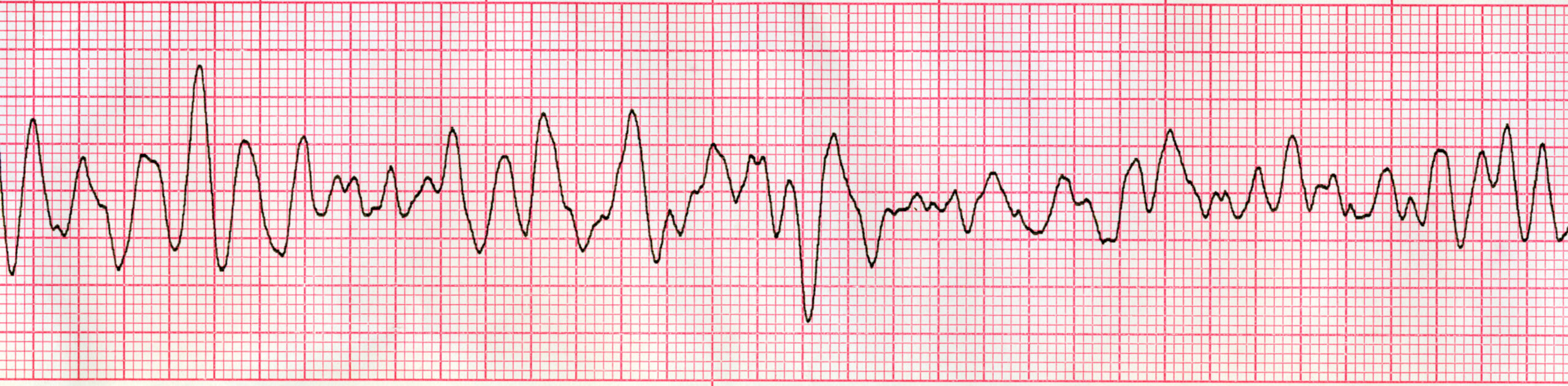
Sinus tachycardia is the most common cause of tachycardia and is usually a normal physiologic response to a treatable condition, such as hypotension, blood loss, fever, pain, or anxiety. A common tachyarrhythmia is atrial fibrillation. Up to 1% of the population has atrial fibrillation, and it is estimated that after age 80 years, this number rises to approximately 9%.4 As the population ages, so too will the number of individuals living with this tachyarrhythmia. Atrial Fibrillation Atrial flutter is a tachyarrhythmia that is more common in men and in those with chronic obstructive pulmonary disease (COPD) and heart failure. Its incidence increases with age. It is estimated to be at least two times more common than paroxysmal supraventricular tachycardia (PSVT). Atrial Flutter PSVT is twice as common in women than in men. It is far more common in people over the age of 65. Atrioventricular nodal reentrant tachycardia (AVNRT) accounts for approximately 60% of cases, with atrioventricular (AV) reciprocating tachycardias responsible for 30% of cases and atrial tachycardia responsible for 10%.5 Paroxysmal Supraventricular Tachycardia (PSVT) For ventricular tachyarrhythmias, prevalence is dependent on the type and duration. For ventricular tachycardia (VT), the most common cause is ischemic heart disease, and it often occurs following myocardial infarction. Scar formation caused by inflammatory diseases, such as amyloidosis and sarcoidosis, may also cause VT. For ventricular fibrillation (VF), coronary artery disease (CAD) is the most common cause. Dilated or hypertrophic cardiomyopathies may lead to VF in some cases. Torsades de pointes, or polymorphic ventricular tachycardia, may be caused by electrolyte imbalances, long QT syndromes, or the use of certain medications (e.g., digitalis). Polymorphic VT seems to be more common in women. Monomorphic Ventricular Tachycardia Torsades de pointes (a type of polymorphic ventricular tachycardia where the QT interval is prolonged) Ventricular Fibrillation Sinus tachycardia is a common response to a physiological stressor. Tachycardia in adults is defined as a heart rate that is greater than 100 beats per minute, whereas tachyarrhythmias generally present with a heart rate greater than 150 beats per minute. It is important to assess the patient with sinus tachycardia and tachyarrhythmia to determine their tolerance of the rhythm and the potential underlying cause.Epidemiology
Related Video – ECG Rhythm Review – Atrial Fibrillation
Related Video – ECG Rhythm Review – Atrial Flutter
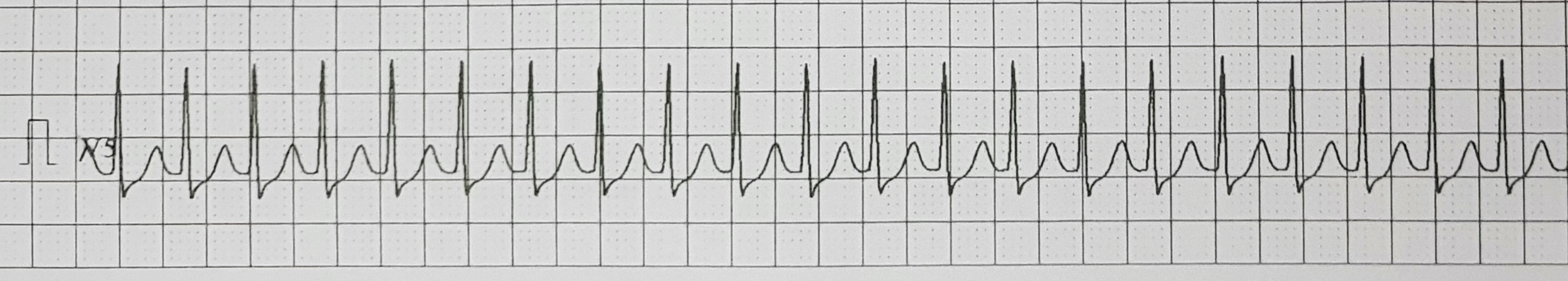
Related Video – ECG Rhythm Review – Supraventricular Tachycardia (SVT)
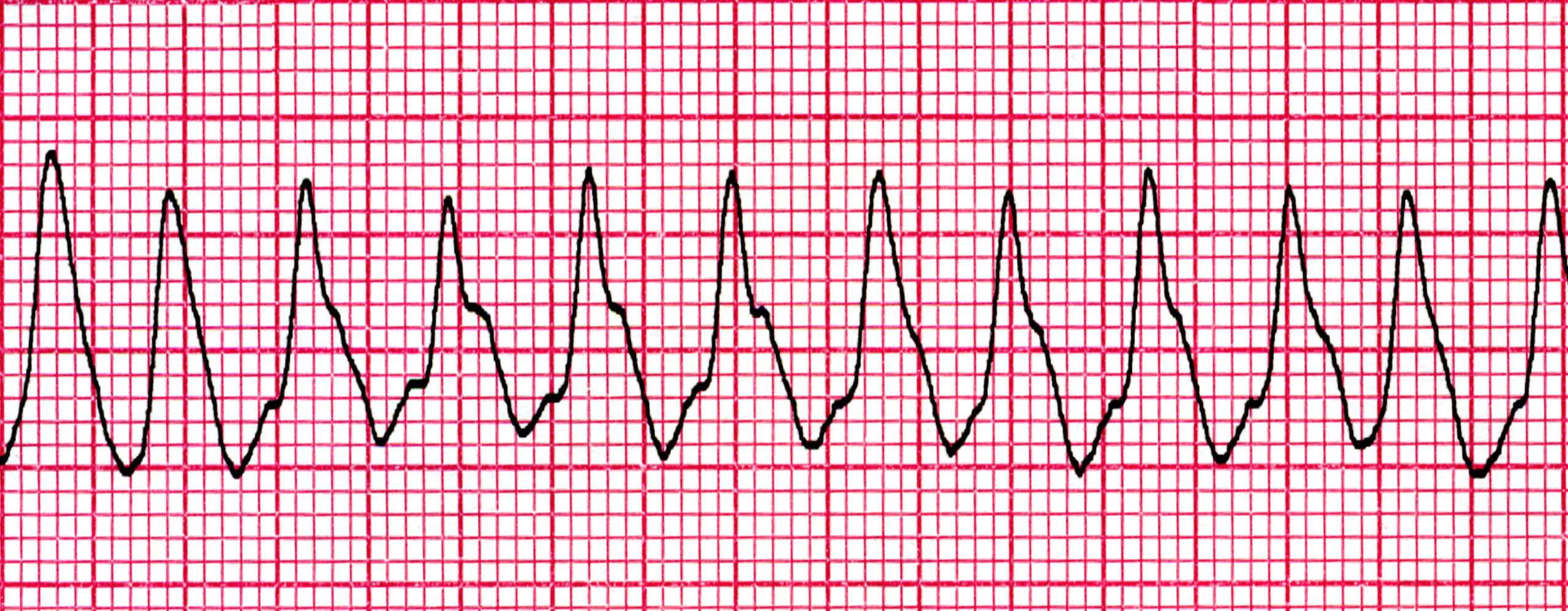
Related Video – ECG Rhythm Review – Ventricular Tachycardia
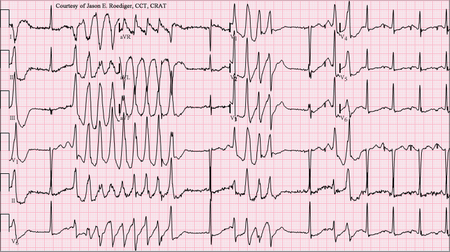
Related Video – ECG Rhythm Review – Polymorphic Ventricular Tachycardia (Torsades de Pointes)
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Mayo Clinic. Tachycardia. 2023.
2. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Hyperthyroidism (Overactive Thyroid). 2021.
3. Ashley EA, Niebauer J. London. Cardiology Explained. National Library of Medicine. 2004.
4. Zeid Nesheiwat; Amandeep Goyal; Mandar Jagtap. Atrial Fibrillation. National Library of Medicine. 2023.
5. Christiana Schernthaner, Franz Danmayr, Bernhard Strohmer. Coexistence of Atrioventricular Nodal Reentrant Tachycardia with Other Forms of Arrhythmias. National Library of Medicine. 2014.