Adult Suspected Stroke Algorithm
Algorithm at a Glance
- The lay rescuer recognizes the signs and symptoms of a stroke and calls EMS quickly.
- EMS begins the assessment and treatment process and transports the patient as rapidly as possible.
- The patient bypasses the ED and is taken directly to the imaging suite, where the stroke team is waiting whenever possible.
- Personnel stabilize the patient and obtain an emergent head CT scan.
- The stroke team does a more in-depth neurological assessment to determine appropriate definitive treatment.
- In the case of a hemorrhagic stroke, the clinician immediately calls for expert consultation.
- In the case of a non hemorrhagic stroke and in the absence of contraindications, the clinician considers the administration of alteplase.
- Endovascular treatment (EVT) is considered for patients with non hemorrhagic stroke who are not alteplase candidates and for patients who received alteplase.
- Following definitive treatment, the patient is continued on the post stroke pathway as defined by the facility.
The Adult Suspected Stroke Algorithm provides a structured, time sensitive approach for recognizing, assessing, and managing patients with suspected acute stroke. This guide walks clinicians through early identification, imaging, decision making, and treatment pathways that are critical for improving neurologic outcomes and reducing disability.
Goals for the Management of Adult Suspected Stroke
The team must succeed in the following to successfully manage suspected stroke in adult patients:
- Quickly recognize stroke.
- Use brain imaging to rapidly differentiate between hemorrhagic and ischemic stroke.
- Complete the scan within 20 minutes of hospital arrival.
- Complete a review of the scan within 45 minutes of hospital arrival.
- Deliver the appropriate treatment based on the type of stroke as quickly as possible.
- Deliver fibrinolytic therapy within 45 minutes of hospital arrival.
- Provide EVT within 90 minutes for direct admits by EMS and 60 minutes for accepted transfer patients
- Admit to the appropriate stroke or neuro unit within 3 hours of hospital arrival.
Understanding Stroke: Types and Impact
A stroke occurs when blood flow to a part of the brain is interrupted or significantly reduced, depriving brain tissue of oxygen and nutrients. Without prompt treatment, brain cells begin to die, leading to potential long term neurologic deficits or death.
The two primary types of stroke are ischemic and hemorrhagic. Ischemic stroke results from an obstruction of blood flow, most commonly due to a thrombus or embolus. Hemorrhagic stroke occurs when a blood vessel ruptures, leading to bleeding within or around the brain. Rapid identification of stroke type is essential, as treatments differ significantly and delays can worsen outcomes.
Adult Suspected Stroke Algorithm Explained
This algorithm was created to present the steps for assessing patients presenting with stroke symptoms and determining management. All ACLS responders must be familiar with the AHA Stroke Algorithm:
Box 1: Identifying Signs of Possible Stroke
Acute ischemic stroke is a clinical condition in which there has been no blood circulation to a part of the brain, causing a sudden loss of brain function in the dependent area(s). The signs and symptoms of stroke can be temporary or permanent, depending on how long the area has been deprived of adequate blood flow.
Common signs of a possible stroke can be rapidly assessed using the BE FAST method. This screening tool helps clinicians and first responders identify stroke symptoms early and initiate urgent care.
BE FAST stands for Balance difficulties, Eye vision loss, Facial droop, Arm weakness, Speech difficulty, and Time to call emergency services. The presence of any of these signs should prompt immediate stroke activation and transport to an appropriate stroke capable facility.
Box 2: Critical EMS Assessments and Actions
A trained EMS responder uses a validated out-of-hospital stroke assessment tool such as the Cincinnati Prehospital Stroke Scale (CPSS) and makes a presumptive diagnosis in < 1 minute.
The sooner EMS personnel bring the patient with suspected stroke to a suitable institution, the better the chances for appropriate treatment. That is because only a dedicated stroke care facility can provide the definitive therapy efficiently and effectively.
EMS personnel can provide supportive treatments to lessen the effects of stroke during transport to the ED. Interventions by EMS en route to the stroke center include:
- Ensuring proper management of the patient’s ABCs
- Initiating stroke protocol
- Providing oxygen for patients with oxygen saturation<94%, or if oxygen saturation cannot be determined
- Checking the patient’s blood glucose levels with appropriate treatment of hypoglycemia
- Performing a rapid neurological assessment within 1minute using an appropriate tool
- Attempting to establish the time when symptoms started
- Determining the nearest stroke center
- Alerting the receiving facility
- Transporting the patient to the stroke center
Key Takeaway
- When a designated Stroke Center is available, transfer the suspected stroke patient to that unit. studies show better patient outcomes in hospitals with dedicated stroke units.
Box 3: Arrival Imaging Suite or ED
Best practice is for the EMS team to bypass the ED and take the patient directly to the imaging suite where the stroke team is awaiting arrival. When the patient arrives, the in-hospital team completes their assessment and stabilizes the patient within 10 minutes.
The stroke team, consisting of qualified nurses, a neurovascular consultant, and an emergency physician, performs the patient’s neurologic assessment. These team members take a focused patient history, perform a physical examination, and determine the time of the onset of stroke symptoms.
The neurologic assessment also makes use of an evaluation tool such as the National Institutes of Health Stroke Scale (NIHSS) or the Canadian Neurological Scale exam. Neurologic assessment by the stroke team and the CT scan should be completed within 20 minutes of the patient’s arrival.
Critical to the treatment of acute ischemic stroke is determining the time of symptom onset confirmed by multiple informants, who may include the patient, family members, and other potential witnesses. The healthcare staff asks when the patient was last known to be healthy.
The general assessment and stabilization process should include:
- Assessing and managing ABCs and vital signs
- Delivering oxygen to keep the oxygen saturation > 94%
- Completing an emergent CT scan of the brain upon arrival or as soon as radiology is ready if the patient is not brought directly to the imaging suite by EMS
- Activating the stroke team if not activated prior to the patient’s arrival
- If not completed by EMS, establishing IV access and obtaining blood samples
- Assessing and treating hypoglycemia
- Performing a basic neurologic assessment using the hospital’s prescribed tool. An excellent tool is the National Institutes of Health Stroke Scale (NIHSS).
- Obtaining an ECG—this should not delay the CT scan
Box 4: CT Scan Interpretation to Determine Cause of Stroke
The most crucial factor in treating acute stroke is to ascertain whether the patient’s symptoms are due to ischemia or hemorrhage. Hence, an important imaging modality is an on contrast CT scan of the head. The scan not only detects ischemia or hemorrhage but may also identify if other anatomic anomalies within the brain may have precipitated the stroke.
Key Takeaway
- The head CT scan must be obtained within 20 minutes of ED arrival.

A Mobile CT Stroke Unit.

Helicopters efficiently airlift patients.
If the patient is transferred to an institution where a CT scanner is not available, the patient must first best be stabilized and then transferred to a higher level of care. Anticoagulation medications must not be given to patients until a CT scan has ruled out the possibility of intracerebral hemorrhage.

A patient awaits a CT scan.
Box 5: Hemorrhagic Stroke Protocol Initiation
If the CT scan detects hemorrhage, a specialist such as a neurologist or neurosurgeon will be consulted to assess the patient for possible surgical intervention and other appropriate treatments.
Box 6: Fibrinolytic Therapy with Alteplase Considered for Patients with Acute Ischemic Stroke
Alteplase is the only currently recommended fibrinolytic medication for nonhemorrhagic stroke. If the team administers alteplase within 3 hours of symptom onset, the patient is likely to have a better outcome. Some patients may be given alteplase up to 4.5 hours after the onset of symptoms. The best results are obtained when the intervention is done in an institution with a specialized stroke unit following the NINDS protocol.
The earlier the treatment is given, the better the outcomes will be. In this step, the patient is reassessed to determine whether the symptoms are quickly resolving. If so, fibrinolytic therapy may not be necessary.
The following table lists the inclusion and exclusion criteria for patients with ischemic stroke who may be eligible for alteplase treatment
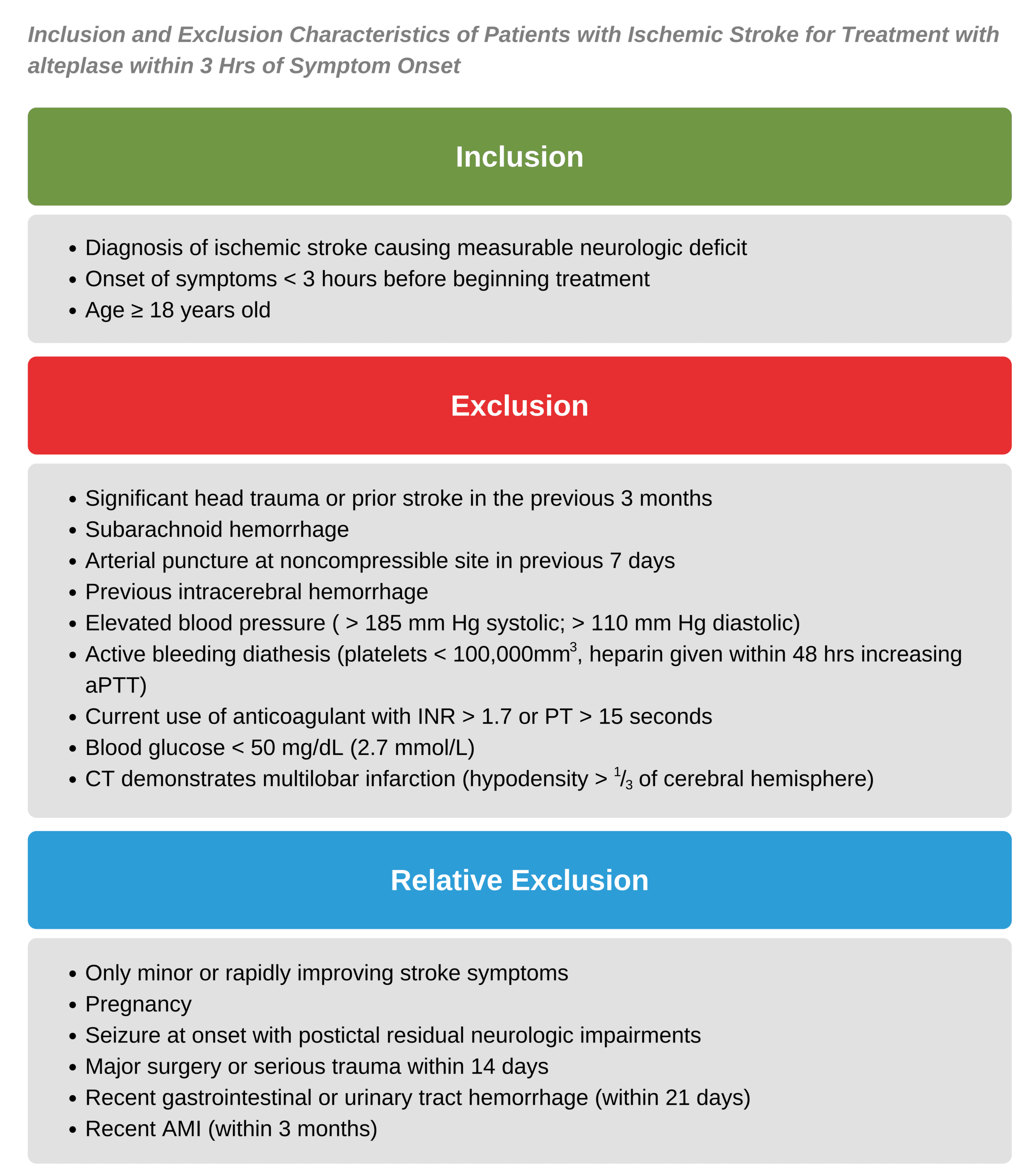
Inclusion and Exclusion Characteristics of Patients With Ischemic Stroke for Treatment With Alteplase Within 3 Hrs of Symptom Onset
Extending the time-dependent criteria for alteplase therapy after the onset of acute stroke symptoms may be possible in certain circumstances.
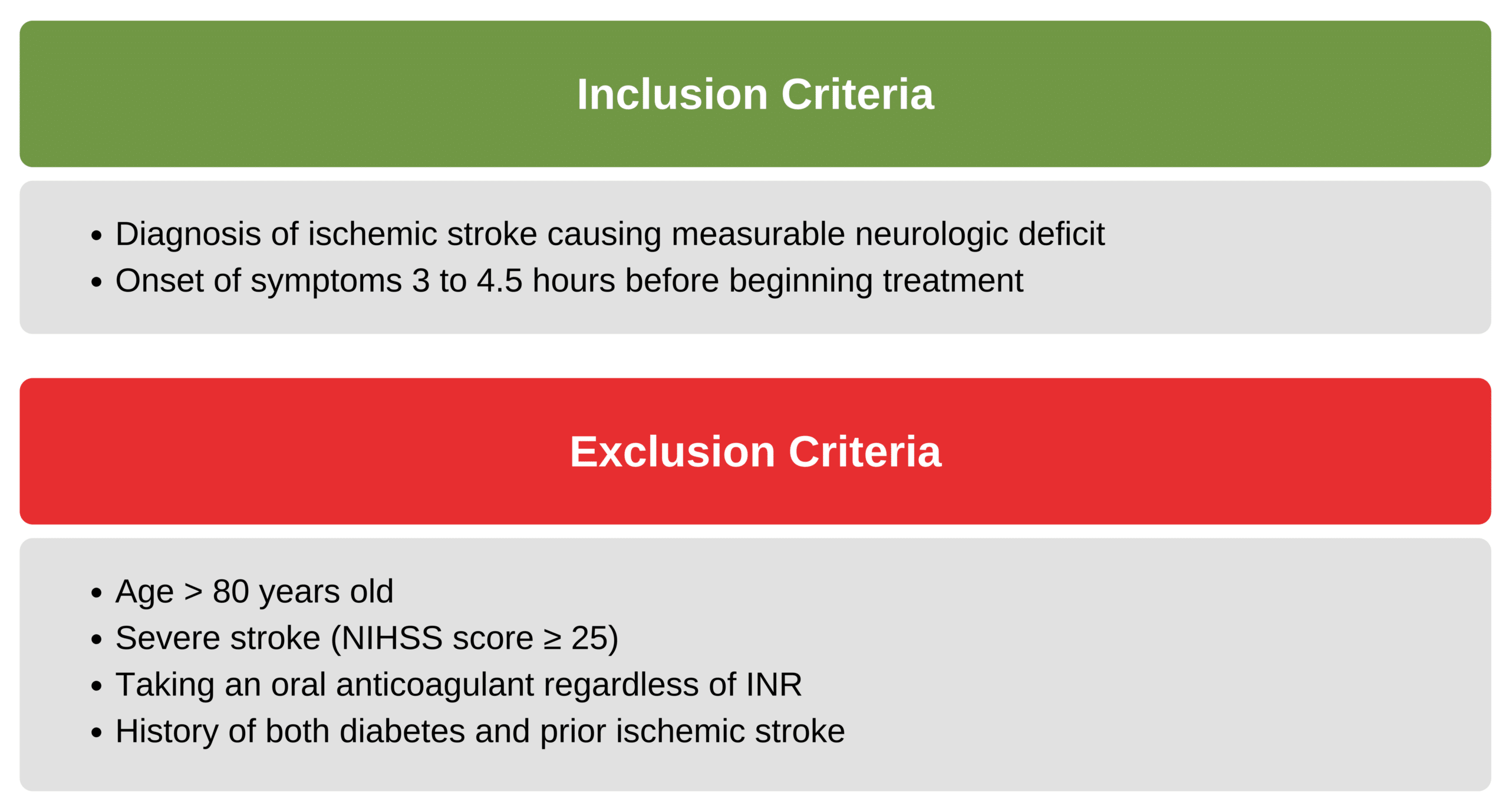
The next table provides additional inclusion and exclusion criteria for patients who may be eligible to receive alteplase between 3 hours to 4.5 hours from the onset of symptoms:
The most significant adverse effect of fibrinolytic therapy is intracranial hemorrhage. Cardiac rhythm disturbances, including wide complex tachycardia, should also be monitored during treatment. Minor and major bleeding complications may also occur elsewhere in the body. Other adverse reactions to alteplase are angioedema and transient hypotension.
Box 7: Fibrinolytic Candidacy Decision Point
In this step, the patient is reassessed to determine whether symptoms are quickly resolving. If so, fibrinolytic therapy may not be necessary.
Box 8: Informed Consent and Alteplase Administration
After it is determined that the patient is a candidate for fibrinolytic therapy, the attending physician must discuss the risks and benefits of alteplase with the patient or a family member. After all questions are answered, and the consent has been signed, the attending physician proceeds with the treatment.
The team should not give anticoagulants or antiplatelet therapy for 24 hours after administering alteplase or until a follow-up CT scan at 24 hours reveals that there is no intracranial hemorrhage present.
Box 9: Evaluate for Endovascular Therapy
Patients who are not candidates for fibrinolytic therapy with alteplase are next evaluated for EVT. Patients receiving alteplase should also be assessed for EVT candidacy.
Endovascular Therapy
Selected patients with ischemic stroke can also receive EVT. This treatment is directed toward resolving a clot that may have formed in the intracerebral blood vessels by disrupting its integrity or removing it and restoring blood flow to the associated brain tissue.
Patients who are not candidates for alteplase should still be evaluated for treatment with EVT. The AHA also recommends EVT for some patients (especially those with large vessel occlusions) in addition to alteplase treatment.
Patients appropriate for EVT are among the following:
- Pre-stroke Modified Rankin Scale (mRS) score of 0 to 1
- Acute ischemic stroke receiving intravenous alteplase within 4.5 hours of symptom onset
- Causative occlusion of the internal carotid artery or proximal middle cerebral artery (MCA)
- Age 18 years and older
- NIHSS score of 6 or more
- Alberta Stroke Program Early CT score (ASPECTS) of 6 or greater
- Treatment can be initiated (via groin puncture) within 6 hours of the onset of symptoms
The clinician should treat any patients meeting the criteria with EVT in addition to IV alteplase.
Box 10: Decision Point for EVT
The team decides whether to proceed with EVT and obtains consent as appropriate.
Box 11: Patient Quickly Taken to Cath Lab for EVT
Patients who qualify for EVT are taken rapidly to the cath lab.
Box 12: Patient Taken to Neurological ICU Following EVT
After the EVT procedure, the patient is admitted to a hospital inpatient unit capable of providing neurological intensive care. The appropriate post-stroke pathway is initiated.
Box 13: Patient Transferred to Stroke Unit, ICU, or Higher Level of Care
Patients with hemorrhagic stroke are transferred to the appropriate inpatient unit or moved to a hospital equipped to provide the appropriate level of care. Patients with nonhemorrhagic strokes who are not EVT candidates are also admitted to a stroke unit, neurological ICU, or transferred to a location with the appropriate level of care. The appropriate post-stroke pathway is initiated.
Understanding the Adult Suspected Stroke Algorithm
The Adult Suspected Stroke Algorithm outlines a step by step clinical pathway designed to ensure rapid recognition, evaluation, and treatment of stroke. It emphasizes early neurologic assessment, timely imaging, and decision making that directly affects patient outcomes.
The video below explains how the algorithm functions in real clinical settings, highlighting key time goals, decision points, and the importance of coordinated team response when managing suspected stroke patients.
Stroke Assessment and Important Time Frames Outside the Hospital
This video focuses on early stroke recognition and pre hospital priorities, highlighting how EMS actions and time based decisions influence treatment eligibility. It reinforces the importance of rapid assessment, early notification, and minimizing delays before hospital arrival.
How Do You Treat a Stroke?
This video explains treatment strategies once stroke has been identified, including imaging based decision making and therapy selection. It supports the algorithm steps above by connecting diagnosis with appropriate medical and interventional treatment options.
What are the Immediate Therapies for Stroke?
This video reviews immediate therapies used in acute stroke care, emphasizing interventions that preserve brain tissue and reduce complications. It aligns with the algorithm by reinforcing rapid treatment once stroke type and eligibility have been determined.
Hypertensive Medications For Stroke
This video discusses blood pressure management in stroke patients and explains why careful control is essential during acute treatment. It complements the stroke algorithm by addressing supportive care that helps prevent secondary injury.
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
