Adult Tachycardia with a Pulse Algorithm
Algorithm at a Glance
- The responder identifies tachycardia and assesses the patient to determine if the heart rate is appropriate for the patient’s condition.
- If possible, the responder identifies and treats the cause of the tachycardia.
- Vagal maneuvers may be attempted if the patient’s condition allows it.
- If the patient is symptomatic, the team considers administering sedation followed by synchronized cardioversion.
Related Video – Understanding the Adult Tachycardia with a Pulse Algorithm
Goals for the Management of Adult Tachycardia
The team must succeed in the following goals to successfully manage tachycardia:
- Identify the tachycardia rhythms, including:
-
- Sinus tachycardia
- Atrial fibrillation
- Atrial flutter
- Supraventricular tachycardia (SVT)
- Wide complex tachycardia
- Identify symptomatic tachycardia with a pulse.
- Appropriately treat the patient with symptomatic tachycardia with a pulse.
Adult Tachycardia Algorithm Explained
This algorithm was created to outline the steps for assessing patients presenting with symptoms and managing their tachycardia.
Box 1: Assessing Appropriateness of Heart Rate for Patient’s Condition
A fast heart rate may be due to a physiologic response to stress, such as dehydration or fever. Significant tachyarrhythmia, however, is a heart rate > 150 bpm. Clinicians agree that when the heart rate is < 150 bpm, patients are unlikely to experience symptoms and instability unless there is preexisting impaired ventricular function.
When diagnosing a patient, the clinician must distinguish whether the tachyarrhythmia is a primary cause of the patient’s symptoms or a result of physiologic stress from other disease conditions.
Some causes of tachycardia are tachyarrhythmia and physiologic stress.
Box 2: Identifying and Treating the Underlying Cause
Hypoxemia can cause tachycardia, which is quite common. The team treats symptomatic patients based on the signs and symptoms of increased breathing effort (e.g., tachypnea and intercostal retractions). Oxygen saturation should be determined immediately using a pulse oximeter and oxygen administered to the hypoxemic patient.
The patient should be monitored carefully using a cardiac monitor and with intermittent blood pressure readings. A 12-lead ECG can better evaluate the tachyarrhythmia diagnosis, but cardioversion should not be delayed if it is indicated.
At this stage, the team looks at the possible causes of tachyarrhythmia and treats it promptly. A decision to seek expert help may be made at any time during the management of tachycardia.
Box 3: Tachycardia with Persistent Symptoms
After initial evaluation and treatment with airway and oxygen supplementation, the patient may have ongoing symptoms. The clinician determines that the symptoms are due to the tachyarrhythmia and diagnoses it as the primary cause.
Unstable symptoms are secondary to reduced cardiac output, as the heart beats too fast or ineffectively due to a lack of coordination between the atria and ventricles. Especially when persistent, this arrhythmia can cause hypotensive symptoms, altered mental status, chest discomfort, acute heart failure, and signs of shock.
If the patient is hemodynamically stable, the team proceeds to Box 4. If hemodynamically unstable, they proceed to Box 5.
Box 4: Synchronized Cardioversion
Before administering synchronized cardioversion to a patient with unstable tachyarrhythmia, the team attempts to establish IV or IO access for possible sedation. Although sedation is preferable for the conscious patient, cardioversion should not be delayed if the patient is unstable, as cardiac arrest may ensue.
Synchronized cardioversion is a method of delivering a shock that is in sync with the QRS complex (delivered at the peak of the R wave). A shock during the relative refractory period of the cardiac cycle in tachyarrhythmias can produce VF, thus worsening the condition of the patient.
Related Video – Synchronized Cardioversion for Tachycardia
Key Takeaway
Indications for Synchronized Cardioversion
- Unstable SVT
- Unstable atrial fibrillation
- Unstable atrial flutter
- Unstable monomorphic (regular) VT
If the tachyarrhythmias have polymorphic QRS complexes (i.e., torsade’s de pointes) in the ECG tracing, synchronization cannot occur. Thus, attempting synchronized cardioversion would be ineffective, and the team should treat torsade’s de pointes like VF with unsynchronized defibrillation.
Some patients with a regular, narrow complex tachycardia may respond to adenosine administration rather than cardioversion.
No data are available to recommend one type of biphasic defibrillator over another. Responders should follow the manufacturer’s recommended energy level to maximize the chances of first shock success.
Box 5: Is the QRS Complex Regular or Wide?
1. Wide-Complex Tachycardia
If the patient is stable and does not require immediate cardioversion, it must be determined whether the QRS is normal or wide (> 0.12 seconds).
An unstable patient diagnosed with wide complex tachycardia should be presumed to have VT, and the appropriate treatment is cardioversion. The team proceeds to Box 6.
If a defibrillator is not immediately available in a case of witnessed, monitored unstable ventricular tachycardia, the responder can attempt a precordial thump unless doing so would delay definitive treatment.
If the QRS is < 0.12 seconds, the team proceeds to Box 7.
VT is a common form of wide-complex tachycardia. SVT with aberrancy, pre-excited tachycardias, and ventricular paced rhythms are also wide-complex tachycardias that can either be VT or SVT with aberrancy. The only difference is that SVT with aberrancy is, as the name suggests, supraventricular.
To distinguish between the two, the team can treat SVT with aberrancy with AV-nodal blocking agents. However, patients with VT may suffer precipitous hemodynamic deterioration if erroneously administered an AV-nodal blocking agent. An electrocardiographic differentiation between the two is not always possible. It is critical to seek expert consultation when there is difficulty in determining the patient’s rhythm.
The team must determine if the wide-complex tachycardia has a regular or irregular rhythm. If it has a regular rhythm, then it is likely due to VT or SVT with aberrancy. An irregular rhythm is due to atrial fibrillation (AF) with aberrancy, pre-excited AF, or torsades de pointes. Teams may need to seek expert help in diagnosing wide-complex tachycardia.
Box 6: Therapy for Wide-Complex Tachycardia
It is ideal first to identify if the wide-complex tachycardia is due to VT or SVT with aberrancy and determine the proper treatment as suggested in the algorithm. If the team is unable to distinguish between the two, it is reasonable to treat the patient with IV adenosine to provide a diagnostic benefit if the patient is stable.
Continuous ECG monitoring is necessary. If the rhythm changes to sinus after adenosine, then the wide-complex tachycardia was due to SVT with aberrancy. If the rhythm does not improve, then adenosine has not affected the rhythm (apart from idiopathic VT, which is rare).
Adenosine 6 mg is administered as a rapid IV push followed by a 20 mL normal saline flush. If the rhythm fails to convert, then it can be followed with 12 mg of adenosine. A defibrillator is always on standby when giving this treatment. At this point, the team leader considers an antiarrhythmic infusion and expert consultation.
Related Video – Adenosine – ACLS Drugs
If the patient is unstable, adenosine might cause the rhythm to revert to VF, which is more detrimental, causing hemodynamic failure. Hence, unstable wide-complex tachycardia is a contraindication for adenosine.
Key Takeaway
- Adenosine and verapamil should NOT be used in unstable wide-complex tachycardias.
Verapamil should not be used for wide-complex tachycardia unless it is supraventricular in origin.
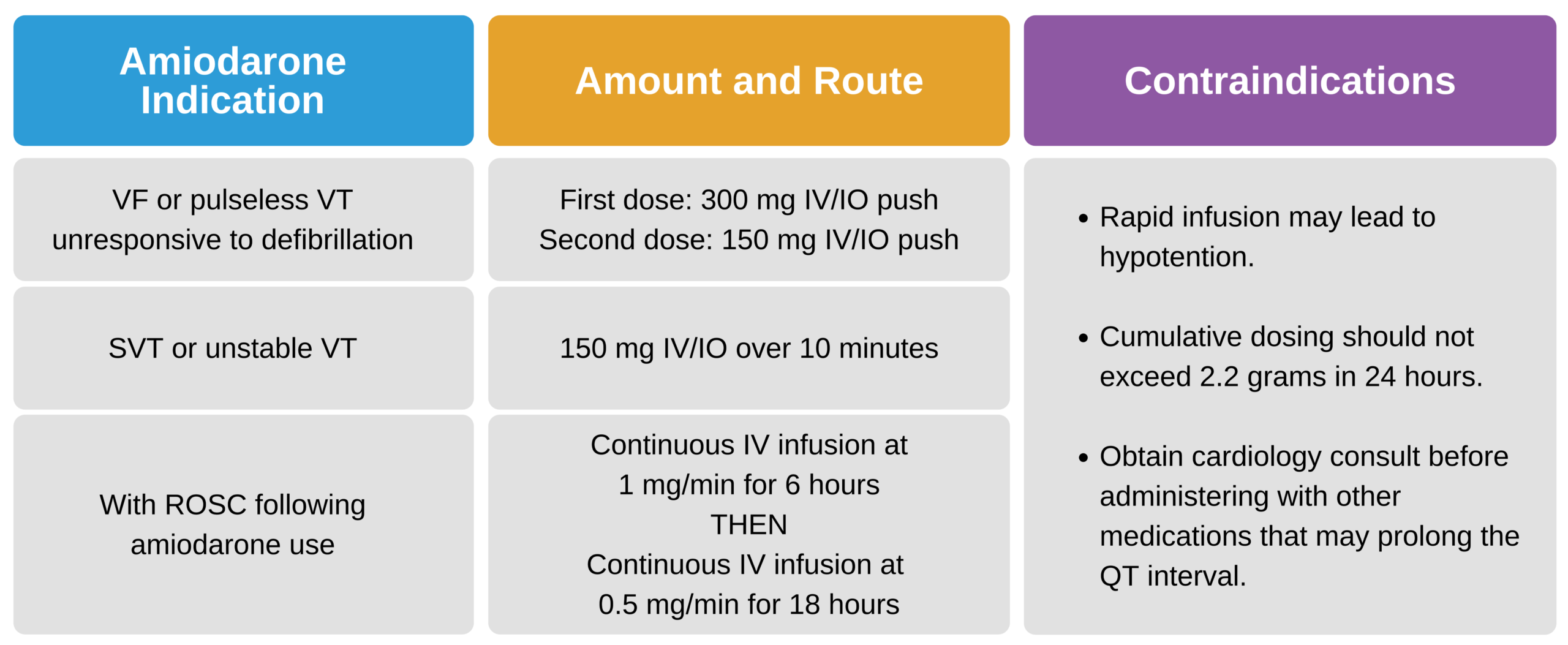
It is appropriate to give IV antiarrhythmics such as procainamide, amiodarone, or sotalol for wide-complex tachycardias. However, for patients with prolonged QT intervals, procainamide and sotalol should be avoided.
Whenever antiarrhythmic therapy fails, it is appropriate to try cardioversion, and the team leader should consider expert consultation.
Procainamide can terminate hemodynamically stable monomorphic VT. It can be administered via IV infusion at a rate of 20–50 mg/min until termination of the arrhythmia or an adverse reaction occurs. Common adverse reactions include hypotension and an increase in QRS duration. The maintenance infusion should be set at a rate of 1–4 mg/min. Patients with congestive heart failure or a prolonged QT interval should not be given procainamide.
Sotalol is given at a dosage of 100 mg (1.5 mg/kg) via slow IV push over 5 minutes. This is an appropriate treatment for monomorphic VT in hemodynamically stable patients. It is not to be used in patients with prolonged QT intervals.
Amiodarone can be used to prevent recurrent monomorphic VT or to treat patients with coronary artery disease with low ejection fraction and refractory ventricular arrhythmias. In ACLS, amiodarone is now considered a first-line antiarrhythmic for cardiac arrest since studies show it increases the chance of ROSC.
Related Video – Amiodarone – ACLS Drugs
Regular Narrow-Complex Tachycardia
Sinus Tachycardia
Sinus tachycardia is a product of physiologic stimulus from clinical conditions such as fever, anemia, or shock. It is defined as a rate > 100 bpm.
Patients with sinus tachycardia do not require specific drug treatment. However, when symptoms persist, treatment is indicated depending on the underlying cause.
In cases with reduced cardiac function, the cardiac output might be reliant on a fast heart rate. And treating these patients to normalize heart rate may cause more harm.
Supraventricular Tachycardia
Most SVT rhythms are caused by a reentrant circuit, which produces impulses that travel circularly within the myocardium. QRS complexes < 0.12 seconds are considered narrow and are characteristic of SVT. SVT can also present with wide QRS complexes (> 0.12 seconds) if there is a pre-existing bundle branch block or a rate-dependent aberrancy.
These reentrant circuits can occur above the ventricles, such as in the atrial myocardium, causing atrial fibrillation(AF) or atrial flutter (AFL). They can also occur in the AV node itself.
If the circuit has both limbs in the AV node, it results in an AV-nodal reentry tachycardia (AVNRT). If the circuit has one limb in the AV node and the other is an accessory pathway, it is known as an AV reentry tachycardia. Combined, these are known as paroxysmal supraventricular tachycardia (PSVT). They create a regular rate exceeding 150 bpm. AVNRT does not exhibit a P wave.
An excited automatic focus can cause supraventricular tachycardias. The focus forms a gradual increase or decrease in the heart rate, similar to impulses in the sinoatrial (SA) node. They can also cause ectopic atrial tachycardias, multifocal atrial tachycardias (MATs), and junctional tachycardias. They are challenging to treat and do not respond to synchronized cardioversion. Regulating them with drugs can slow the conduction through the AV node, which slows the ventricular rate.
Box 7: Narrow Complex Tachycardia
For a narrow-complex tachycardia, the team obtains IV or IO access and a 12-lead ECG. It is reasonable to attempt vagal maneuvers and adenosine. The team leader may order β-blockers or calcium channel blockers and call for an expert consultation.
Box 8: Persistent Tachycardia
In the presence of refractory tachycardia, the team determines the underlying cause and considers adding antiarrhythmic medications.
More Free Resources to Keep You at Your Best
Editorial Note
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.