Stroke: Assessment and Important Time Frames Outside of the Hospital
ACLS Certification Association videos have been peer-reviewed for medical accuracy by the ACA medical review board.
Article at a Glance
- Computed tomography (CT) is the most important diagnostic tool in acute stroke.
- Treatment for acute stroke may include fibrinolytic therapy or surgery (embolectomy).
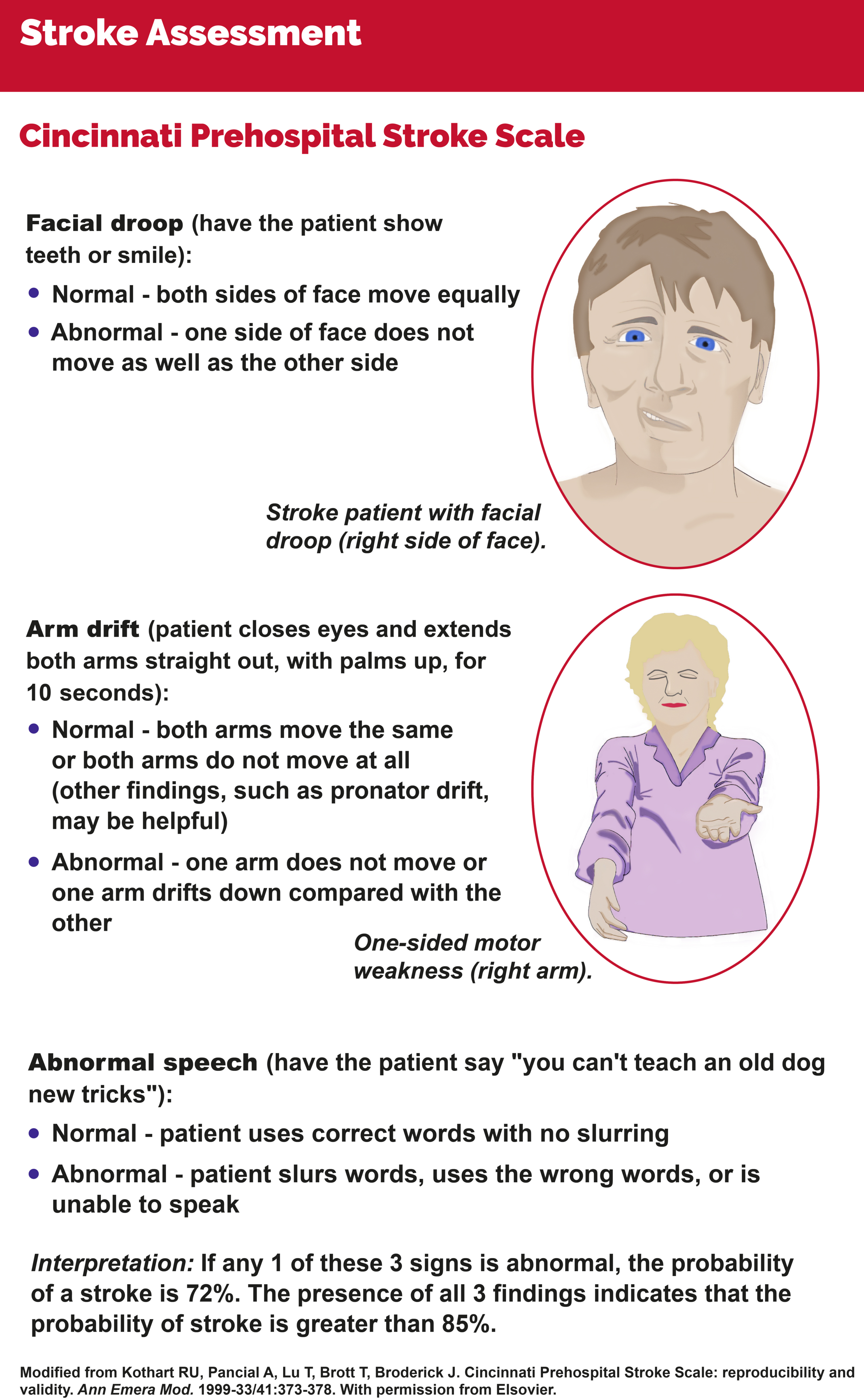
- The Cincinnati Prehospital Stroke Scale (CPSS) uses three metrics to determine the likelihood that an individual is experiencing an acute stroke.
- The 8 Ds of Stroke Care represent diagnosis, treatment, and potential chokepoints in the system of care.
- The Adult Suspected Stroke algorithm is used to direct care actions in the pre-hospital and emergency department (ED) setting, as well as generalized stroke care.
Part of the training of an advanced cardiac life support (ACLS) team member is the initial diagnosis and management of acute stroke in the out-of-hospital care setting. Likewise, ACLS providers must know what to do when triage has sent an acute stroke patient to the ED.
The most important diagnostic tool for acute stroke patients is a CT scan of the head to confirm if the stroke is secondary to ischemia1, in which fibrinolytic therapy is recommended, or secondary to an intracerebral bleed where surgery is the recommended intervention.
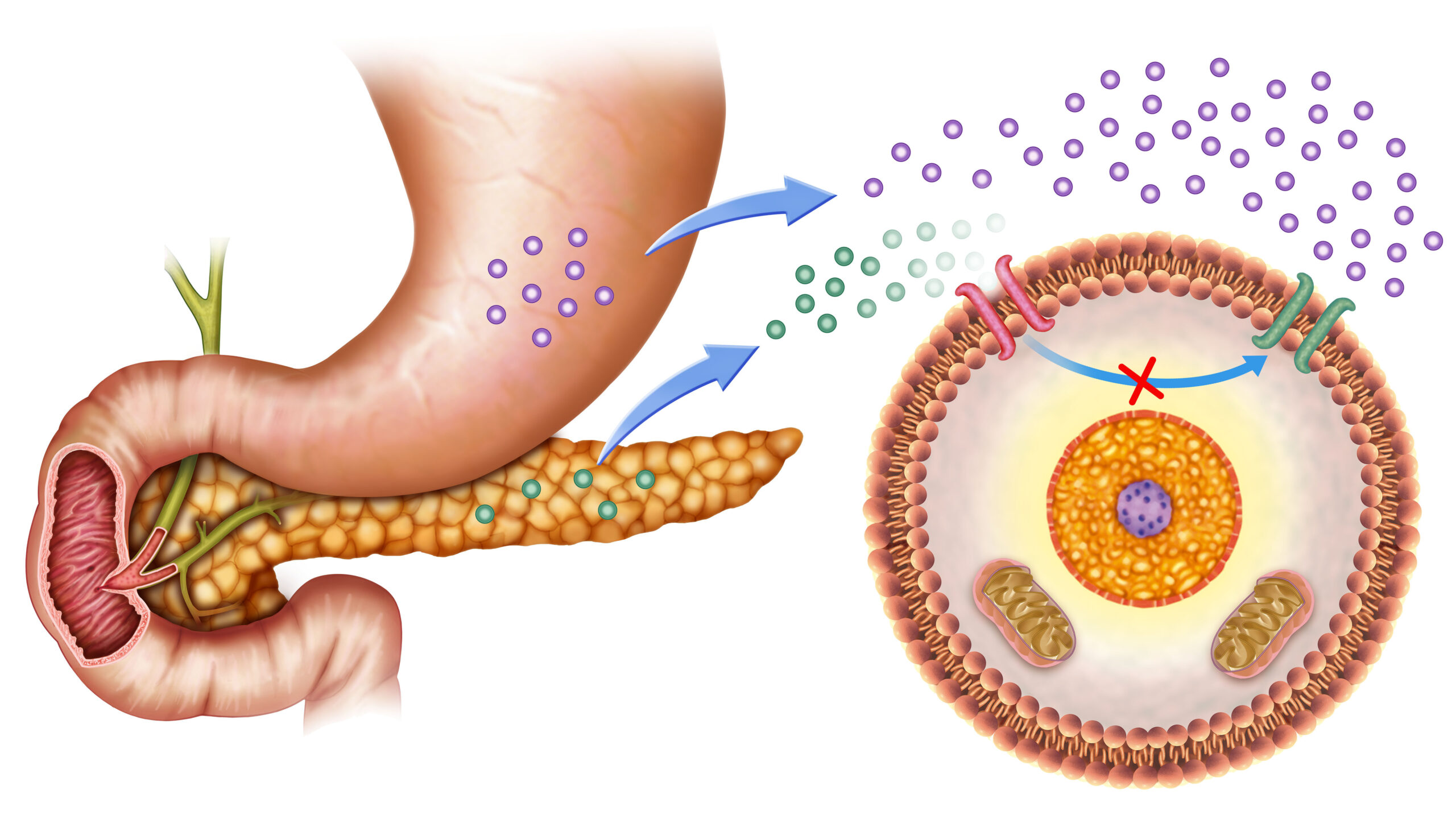
Studies show that most acute strokes are ischemic and patients are therefore candidates for fibrinolytic therapy. An electrocardiogram (ECG) may be of value to determine the presence of arrhythmia and myocardial infarction because they may indicate an embolic stroke. However, an ECG does not take precedence over a CT scan.
Management of acute stroke means immediately determining patients who are eligible for fibrinolytic therapy to increase survival rates with optimal neurologic outcomes. There is a strict time frame in which to administer these life-saving drugs.
The National Institute of Neurological Disorders (NINDS) aims to achieve at least an 80% success rate in meeting treatment times when the stroke algorithm is used.
Related Video – Understanding the Stroke Algorithm
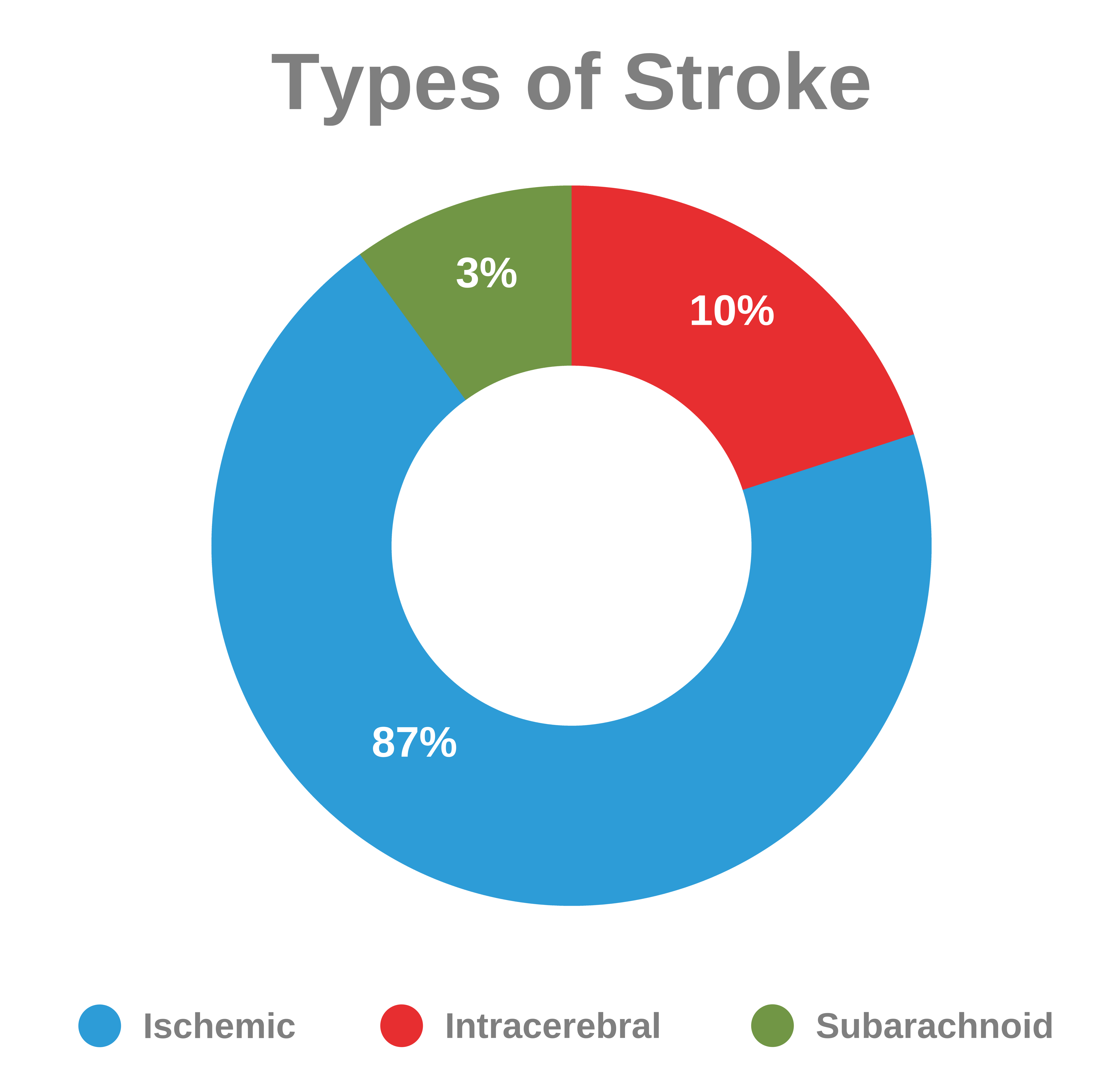
The three main types of stroke are ischemic, intracerebral, and subarachnoid.
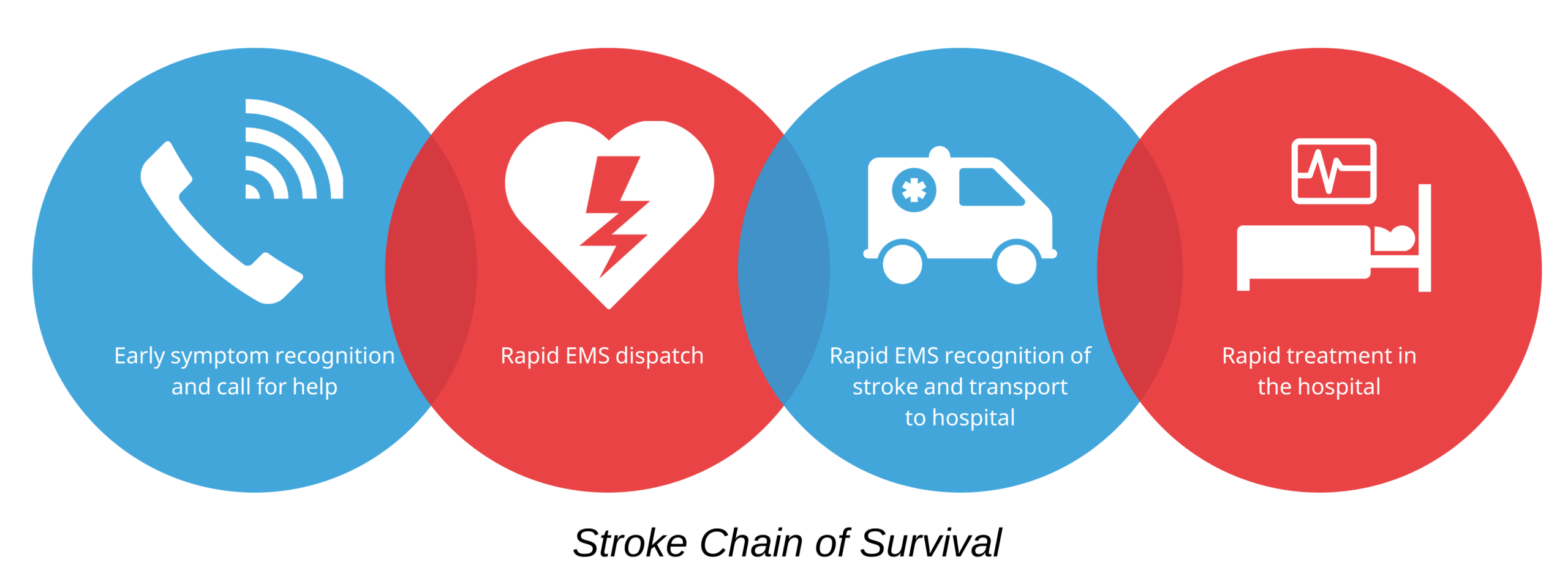
Intravenous fibrinolytic therapy is only useful if it is given within 3–4.5 hours after onset of symptoms of acute ischemic stroke.2 Endovascular therapy may be pursued if it is performed within 6 hours after the onset of symptoms. Therefore, it is crucially important to elicit the exact time of symptom onset from the patient or relatives. Recognizing the clinical signs and symptoms of acute stroke remains a challenge for the community, and studies have shown that, in most cases of stroke, the onset of symptoms occurs at home. Family members often do not recognize acute stroke symptoms even in high-risk patients (i.e., those diagnosed with atrial fibrillation or hypertension). A proposed system of care is the Stroke Chain of Survival where the community, emergency medical services (EMS), and institutions work together to manage acute stroke. Stroke Chain of Survival The first link represents the recognition of stroke signs and symptoms by the patient’s family members, or the patient themself, who then call EMS. The second link is the immediate dispatch of EMS to the patient’s location. The third link is the transport of the patient to a suitable institution via EMS, with providers performing the pre arrival notification to the receiving hospital. The fourth and final link is the diagnosis and treatment of stroke in hospital.Time Frames for Acute Stroke Care
The 8 Ds of stroke care represent diagnosis, treatment, and potential delays in stroke management3: Read: Advanced Airways: Endotracheal IntubationThe 8 Ds of Stroke Care
The CPSS simplifies the clinical diagnosis of acute stroke for ACLS providers and is especially useful in out-of-hospital situations so that the provider can rapidly transport the patient to an appropriate stroke facility with prior notification to the ED staff.4 Providers use the Cincinnati Prehospital Stroke Scale to assess the patient for stroke prior to arrival at the hospital. The CPSS includes three clinical signs that an acute stroke patient may present with: There is a 72% chance of stroke if a patient presents with one clinical sign or symptom, and an 85% chance of acute stroke if a patient demonstrates all three clinical signs and symptoms.5Stoke Assessment
Related Video – Hypertensive Medications For Stroke
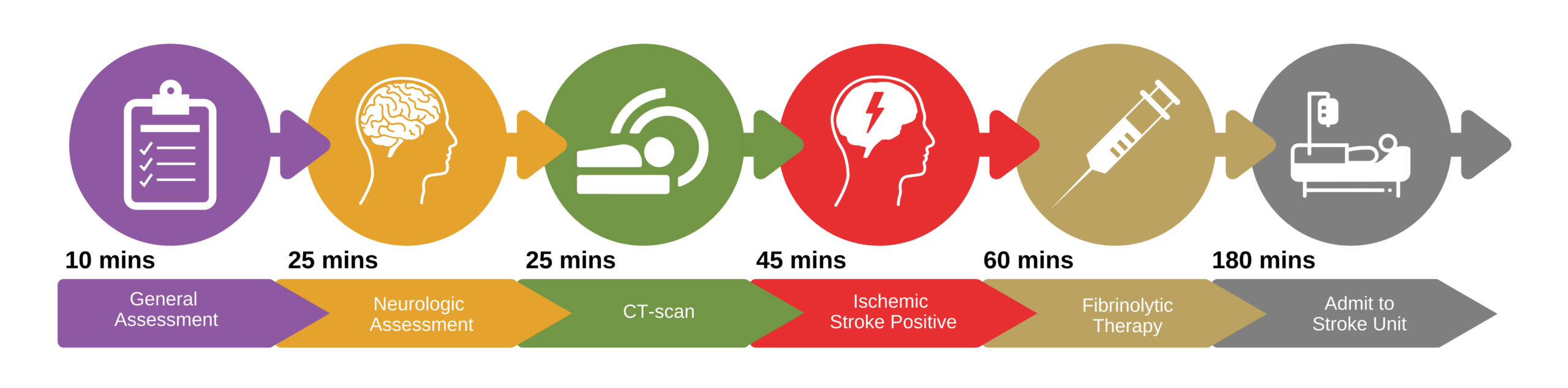
The NINDS set critical time periods for assessment and treatment of stroke, with fibrinolytic therapy for acute stroke patients starting as soon as possible after the patient arrives in the ED. The ideal time for treatment is within 60 minutes. NINDS emphasizes that the critical period for administration of fibrinolytic therapy (timed from the onset of symptoms) is 3 hours, or 4.5 hours in select patients. The administration of endovascular therapy must be administered within 6 hours from the onset of symptoms. Admission to a stroke unit or a critical care unit should be within 3 hours from when the patient enters the ED. Critical time periods for assessment and treatment of stroke.Critical Time Periods
The Stroke Algorithm
Suspected Stroke Algorithm
The stroke algorithm is divided into several time periods for the rapid diagnosis and management of acute stroke.
The algorithm emphasizes the duties that EMS should perform for the immediate assessment and stabilization of the patient, it demonstrates the neurologic assessment by the stroke team in a capable stroke treatment facility, and it shows the importance of a CT scan in diagnosis between ischemic and hemorrhagic stroke.
The algorithm also stratifies the appropriateness of fibrinolytic treatment for an acute ischemic stroke patient and provides instructions for general stroke care.
Acute ischemic stroke is brought about by a significantly decreased perfusion to a portion of the brain, causing a sudden loss of function.6
Patients will present with signs and symptoms of stroke depending on the severity of the stroke (how and where the brain is affected). Symptoms may be intermittent or constant.
Patients will present with unilateral weakness or numbness of the face, arms, or legs. Mental confusion, slurred speech, and difficulty in understanding are clinical signs as well. Some patients may report vision loss in one or both eyes.
Patients or other people with the patient must immediately call 9-1-1 for help at the first sign of stroke.
It is recommended that experienced EMS bring the patient to the ED. However, about one-half of patients are brought to the ED by family members, denying the patient the initial steps in management for acute stroke at the pre-hospital level and transfer with proper endorsement to a competent healthcare institution.
Trained EMS personnel can transfer the patient to a facility that is competent in handling stroke patients. EMS personnel can also describe the patient’s situation properly to the receiving hospital. That allows the hospital to prepare for the incoming patient and provide care within the critical time period.
EMS uses the CPSS to determine if the patient is experiencing symptoms of an acute stroke. Immediate transfer of an acute stroke patient to a suitable institution increases the success of their management. EMS can provide the initial steps in managing the patient while in transit. EMS ensures that the patient’s airway, breathing, and circulation are being managed effectively. Supplemental oxygen is provided when the O2 saturation is less than 94%. EMS personnel can also check the patient’s blood glucose level during this time. That is important because hypoglycemia and hyperglycemia can sometimes be confused with stroke symptoms. It is important for EMS to determine when symptoms started to establish a neurologic baseline. If the patient wakes up with stroke symptoms, the neurologic baseline is assumed to be the last time the patient was seen to be normal. A family member or companion must be consulted to confirm the onset of symptoms. EMS performs a quick history and physical examination focused on acute stroke symptoms and relays their findings to the healthcare facility of choice. That allows the receiving hospital or stroke unit to prepare to receive an acute stroke patient.Critical EMS Assessments and Actions
In patients experiencing acute stroke, there are established critical time frames of care and treatment that begin prior to the patient arriving at the hospital. It is essential that EMS personnel know what to look for in acute stroke and communicate appropriately with the receiving hospital or stroke unit.Summary
More Free Resources to Keep You at Your Best
Editorial Sources
ACLS Certification Association (ACA) uses only high-quality medical resources and peer-reviewed studies to support the facts within our articles. Explore our editorial process to learn how our content reflects clinical accuracy and the latest best practices in medicine. As an ACA Authorized Training Center, all content is reviewed for medical accuracy by the ACA Medical Review Board.
1. Dale Birenbaum, MD, Laura W. Bancroft, MD, and Gary J. Felsberg, MD. Imaging in Acute Stroke. West Jem. 2011.
2. Mònica Millán, Laura Dorado, and Antoni Dávalos. Fibrinolytic Therapy in Acute Stroke. Current Cardiology Reviews. 2010.
3. Ghabaee Mojdeh, Balali Pargol, Pourghaz Bahareh. Stroke Patient Workflow: Optimizing and Simplifying of the 8Ds in Acute Stroke Care. Journal of Registry Management. 2021.
4. Edward C. Jauch, Brett Cucchiara, Opeolu Adeoye, William Meurer, Jane Brice, Yvonne (Yu-Feng) Chan, Nina Gentile and Mary Fran Hazinski. Adult Stroke. American Heart Association. 2010.
5. Christy Pu, Jiun-Yu Guo, Yu-Hua-Yeh, and Placide Sankara. Comparison of knowledge on stroke for stroke patients and the general population in Burkina Faso: a cross-sectional study. AIMS Public Health. 2020.
6. Mayo Clinic. Stroke. 2022.